Antibiotics for the intestines
Intestinal infections are the second most common disease.
ARVI traditionally takes first place. But antibiotics are used to treat the intestines in only 20% of all diagnosed cases. The indication for prescribing drugs is the development of the following symptoms:
- significant increase in body temperature;
- cutting pain in the abdomen;
- diarrhea occurring more than 10 times a day;
- uncontrollable vomiting;
- signs of developing dehydration.
Drugs from the antibiotic category can be prescribed for dysbiosis, colitis and stool disorders (diarrhea).
Antibiotics to treat intestinal infections
The cause of infectious damage to the gastrointestinal tract is the penetration of pathogenic microflora into the human body. These can be staphylococci, protozoa, enteroviruses, salmonella, etc.
The indication for the use of drugs from the category of antibiotics is the lack of positive dynamics of treatment from previously prescribed drugs. But when dysentery or cholera is diagnosed, they are prescribed to be taken immediately.
To treat intestinal pathology, medications from the following categories can be used:
- cephalosporins;
- fluoroquinolones;
- tetracyclines;
- aminoglycosides;
- aminopenicillins.
If we talk about specific drugs, the most often prescribed are:
- Levomycetin. Broad-spectrum antibiotic. Very effective against Vibrio cholerae. Recommended in the absence of a therapeutic effect after taking other medications. Prohibited for use in children.
- Tetracycline. Practiced for the treatment of intestinal infections caused by salmonella and amoebas. Effective against the causative agent of anthrax, plague, psittacosis. Long-term treatment with drugs of this group can provoke the development of dysbiosis, therefore, after tetracycline antibiotics, the patient is recommended to take synbiotics.
- Rifaximin. The drug is less aggressive than tetracycline, and therefore can be prescribed to both adults and children.
- Ampicillin. A semi-synthetic agent that is effective against a large number of pathogens. Allowed for children and pregnant women.
- Ciprofloxacin (from the group of fluoroquinolones). Does not cause dysbiosis.
- Azithromycin (from the group of macrolides). Suppresses the growth of pathogenic microflora in three days. The safest medicine with virtually no side effects.
- Amoxicillin.
Pseudomembranous colitis is a dangerous complication of antibiotic treatment
The widespread spread of infectious diseases and the impossibility of their treatment without the participation of chemotherapy drugs leads to the development of undesirable reactions. Most antibiotics have side effects such as nephrotoxicity, hepatotoxicity, and allergic reactions. Antimicrobial agents are not selective, having a detrimental effect on both harmful microorganisms and healthy intestinal flora. The result is diarrhea. But not everyone knows about the existence of such a side effect of antimicrobial drugs as pseudomembranous colitis. MedAboutMe will tell you what kind of disease this is and how it manifests itself.
The use of antibiotics for dysbacteriosis
When dysbiosis develops, medications from the group of antibiotics are prescribed to suppress pathogenic bacteria. Most often, drugs from the following groups are recommended for use:
- penicillins;
- tetracyclines;
- cephalosporins;
- quinolones.
Metronidazole may also be prescribed.
Since antibiotics already have a detrimental effect on the state of the microflora of the digestive tract, they are used for dysbiosis of the small intestine, accompanied by malabsorption syndrome and motility disorders.
The following drugs are most often prescribed for the treatment of dysbiosis:
- Amoxicillin. A semi-synthetic drug from the penicillin group. Gives good results when taken orally, as it is resistant to the aggressive gastric environment.
- Alpha Normix. Non-systemic broad-spectrum antibiotic. The active substance is rifaximin. Indicated for dysbiosis caused by diarrhea and infectious pathologies of the gastrointestinal tract.
- Flemoxin Solutab. Semi-synthetic drug of the penicillin group. Has a bactericidal effect.
- Levomycetin. Broad-spectrum antimicrobial agent. Prescribed for the treatment of dysbacteriosis caused by intestinal infection and pathologies of the abdominal organs. It can also be prescribed as an alternative drug if previously selected medications have not given a positive result.
With the development of dysbiosis of the large intestine, the following are prescribed:
The drugs are effective against yeast, staphylococcus and proteus, which are the main cause of colon dysbiosis. The drugs do not have a significant effect on the state of natural microflora.
Additional diagnosis of this inflammation
The most suitable method for the combination of speed (less than one hour) and efficiency of pathogen detection is considered to be the latex agglutenation method, which makes it possible to detect enterotoxin A, produced by Clostridium difficile, in the patient’s stool with an 85% probability. Bacteriological testing is also possible, but it is not available everywhere, takes more time and is quite expensive.
In addition, it is possible to use computed tomography as an aid, which can detect thickening of the intestinal walls and the appearance of inflammation in the abdominal cavity.
What is Crohn's disease and how is it treated?
Antibiotics for colitis
Treatment of colitis of bacterial origin is impossible without a course of antibiotics. For nonspecific ulcerative inflammation of the colon, medications of this category are prescribed in the event of a secondary bacterial infection.
In the process of treating pathology, the following can be used:
- group of sulfonamides for mild/moderate disease;
- broad-spectrum agents for severe disease.
In order to prevent the development of dysbiosis, the patient is recommended to take probiotics. This could be Nystatin or Colibacterin. The latter contains live E. coli, which contribute to the restoration and normalization of microflora.
For colitis, the following medications may be prescribed:
- Alpha Normix. A broad-spectrum agent with a pronounced bactericidal effect, which helps reduce the pathogenic load.
- Furazolidone. A drug from the nitrofuran group. Has an antimicrobial effect.
- Levomycetin. The product is active against pathogenic microflora and also exhibits a bactericidal effect. Since numerous side symptoms may develop while taking Levomycetin, the dosage and treatment regimen should be selected individually. Intramuscular administration of the drug is possible.
Self-treatment of colitis with antibiotics is completely unacceptable. A qualified specialist must select medications and determine the dosage regimen. It is also necessary to inform the doctor about all medications taken in order to exclude the development of negative reactions due to drug interactions.
Symptoms
In mild cases, pseudomembranous colitis is manifested by the development of diarrhea while taking antibiotics. Moreover, after discontinuation of antibacterial therapy, the symptoms of the disease completely disappear.
Severe and moderate forms can develop both during the use of antibiotics and after their discontinuation (within 10 days after stopping antibiotic therapy).
The first symptom of pseudomembranous colitis in such cases is severe watery diarrhea. In severe cases, stool resembles rice water. Large fluid losses lead to dehydration and impaired water-electrolyte metabolism, which is clinically manifested by tachycardia, paresthesia (a feeling of crawling on the skin), decreased muscle tone and cramps.
In especially severe cases, an admixture of blood is noticeable in the stool from the first days, up to bloody diarrhea. Then, against the background of diarrhea and symptoms of dehydration, signs of intoxication develop:
- weakness;
- headache;
- loss of appetite;
- body temperature rises (usually up to 38 o C);
- cramping pain appears along the large intestine.
The typical localization of pain in pseudomembranous colitis is the projection of the sigmoid colon (lower abdomen on the left).
There are fulminant forms with a fatal outcome. The cause of death in most cases is toxic expansion of the colon followed by perforation. Some malignant forms resemble cholera - the death of the patient occurs due to rapid dehydration of the body, leading to hyperkalemia and cardiac arrest.
Antibiotics for the intestines
Intestinal infections are the second most common disease. ARVI traditionally takes first place. But antibiotics are used to treat the intestines in only 20% of all diagnosed cases.
The indication for prescribing drugs is the development of the following symptoms:
- significant increase in body temperature;
- cutting pain in the abdomen;
- diarrhea occurring more than 10 times a day;
- uncontrollable vomiting;
- signs of developing dehydration.
Drugs from the antibiotic category can be prescribed for dysbiosis, colitis and stool disorders (diarrhea).
Antibiotics to treat intestinal infections
The cause of infectious damage to the gastrointestinal tract is the penetration of pathogenic microflora into the human body. These can be staphylococci, protozoa, enteroviruses, salmonella, etc.
The indication for the use of drugs from the category of antibiotics is the lack of positive dynamics of treatment from previously prescribed drugs. But when dysentery or cholera is diagnosed, they are prescribed to be taken immediately.
To treat intestinal pathology, medications from the following categories can be used:
- cephalosporins;
- fluoroquinolones;
- tetracyclines;
- aminoglycosides;
- aminopenicillins.
If we talk about specific drugs, the most often prescribed are:
- Levomycetin. Broad-spectrum antibiotic. Very effective against Vibrio cholerae. Recommended in the absence of a therapeutic effect after taking other medications. Prohibited for use in children.
- Tetracycline. Practiced for the treatment of intestinal infections caused by salmonella and amoebas. Effective against the causative agent of anthrax, plague, psittacosis. Long-term treatment with drugs of this group can provoke the development of dysbiosis, therefore, after tetracycline antibiotics, the patient is recommended to take synbiotics.
- Rifaximin. The drug is less aggressive than tetracycline, and therefore can be prescribed to both adults and children.
- Ampicillin. A semi-synthetic agent that is effective against a large number of pathogens. Allowed for children and pregnant women.
- Ciprofloxacin (from the group of fluoroquinolones). Does not cause dysbiosis.
- Azithromycin (from the group of macrolides). Suppresses the growth of pathogenic microflora in three days. The safest medicine with virtually no side effects.
- Amoxicillin.
Approach to treatment of intestinal colitis with medications
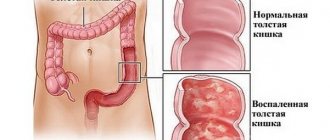
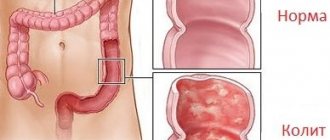
Colitis is an inflammation of the large intestine (from the Latin kolon - large intestine).
The main symptom of the disease is pain in the lower abdomen. The causes are poisoning, infections, poor quality food, stress, allergies and parasites. Colitis can be acute - occurs quickly with severe pain, nausea and diarrhea, and chronic - constant discomfort with a constant feeling of heaviness, loss of appetite and nausea. To avoid complications and consequences that involve surgical intervention (for example, intestinal ischemia), it is better to immediately take care of your health condition and begin treatment.
Use of medications
Therapy for intestinal colitis helps prevent serious complications - this is the main reason why it is worth immediately preventing the development of the disease.
The treatment complex usually consists of:
- hormonal drugs (corticosteroids);
- anti-inflammatory drugs;
- antihistamines;
- sedatives;
- analgesics;
- anti-diarrhea medications;
- antibiotics;
- vitamins and probiotics.
Is it wise to use medications?
Medication is the only reasonable option when colon inflammation occurs. If colitis progresses, it can lead to intestinal ischemia, diverticulosis, peritonitis and microcolitis.
One could rely on folk remedies, but these are only half-measures that will not bring quick results, if they can help with anything at all.
Followers of folk remedies say that infusions and herbs are gentle on the intestines, but the same result can be achieved by using drugs and probiotics together.
Only medications can cope with the situation, since there is no need for surgery.
The direction of action of drugs and a review of the most effective drugs
Only the use of a complete medicinal complex will help to quickly cope with colitis and the complications that it causes.
Each type of drug solves individual problems:
- Anti-inflammatory medications are aimed at relieving inflammation that causes bloating and discomfort.
- Antibiotics and corticosteroids and anti-allergy medications are responsible for eliminating infections, pathogenic bacteria and allergies. They perform the most important function in the treatment of colitis - eliminating the original source of the disease.
- Analgesics help manage pain
- Diarrhea medications eliminate the side effects of nausea and loose stools.
- Sedatives help normalize the nervous system, which is in an irritated state due to intestinal problems.
- Vitamins restore the level of nutrients in the body that are washed away by diarrhea, and probiotics normalize the intestinal microflora with the help of beneficial bacteria.
Festal
Used for acute intestinal disorders: ulcerative and intestinal colitis, pancreatitis. The active ingredient - pancreatin - helps the absorption of nutrients and saturates with bile, which normalizes the general condition of the intestines. Used for gastric resection. Combines well with antibiotics, vitamins and analgesics. Prescribed by a doctor when the main symptom is diarrhea.
Panzinorm
Panzinorm is an enzyme preparation. They are usually prescribed for enzyme deficiency due to dysbacteriosis. In the case of colitis, dysbiosis will accompany the disease, so it is necessary to take it. Helps cope with constipation.
No-shpa
The medicine is especially good for chronic colitis, since its main function is to quickly relieve the spasm that accompanies chronic colitis. It is precisely because a spasm can appear at any time that the medicine is used everywhere.
Sulfasalazine
The active substance - sulfaperidine - accumulates in the connective tissue of the intestines, which allows you to get rid of streptococci, gonococci, E. coli and other bacteria that can cause colitis. In addition, it has anti-inflammatory activity.
Bellasthesin
The benzocaine and belladonna extract included in the composition help eliminate spasms and reduce the level of acidity, which provokes intestinal inflammation.
Bifidumbacterin
The bifidobacteria included in the composition eliminate diarrhea and nausea and normalize the intestinal microflora.
Treatment of the disease
Drug therapy should be prescribed by a gastroenterologist and carried out under his supervision.
However, there are basic rules that should not be forgotten:
- take antibiotics and probiotics at different times;
- take medications strictly on time;
- follow the diet prescribed by your doctor;
- give up alcohol and smoking;
- Do not eat fermented milk products while taking antibiotics.
Antibiotics are prescribed if colitis was caused by an intestinal infection. Doctors recommend taking antibacterial drugs precisely in the presence of infection. If the disease has another cause, antibiotics can only harm the intestines and stomach, which will not speed up the healing process.
Three types of infections cause colitis:
- Bacterial infection.
- Parasitic infection.
- Viral infection.
- Colitis is often provoked by salmonella and shigella, then salmonellosis develops and the risk of developing shigella dysentery.
– how to restore the body after antibiotics?
Antibacterial therapy
There are two types of antibiotics that are used for colitis: sulfonamides and “broad-spectrum” antibiotics. Sulfonamides are prescribed when the disease is mild to moderate in severity.
If treatment continues for a long time and the patient is prescribed several drugs at once, this provokes dysbiosis - a process when the beneficial microflora of the stomach and intestines is destroyed. In such cases, taking pribiotics and probiotics is indicated.
The following medications are commonly used:
Painkillers
There is an opinion that painkillers themselves provoke gastric colitis (ibuprofen, aspirin, naproxen), since they have a detrimental effect on the stomach and intestines, disrupting the microflora and destroying their very structure. However, their use cannot be avoided due to severe pain.
An approximate list of helpful analgesics:
Loperamide helps because it is an opioid against diarrhea in inflammatory bowel disease. Due to the removal of inflammation, it will decrease.
Rectal suppositories
Many doctors prescribe rectal suppositories because when drugs are taken orally, the level of effectiveness decreases as they end up in the stomach.
Once in the rectum, the active ingredients are quickly absorbed and do not lose their effectiveness.
- Salofalk;
- Clotrimazole;
- Gyno-peveril;
- Ciclopirox.
Restoration of microflora
The use of painkillers and antibiotics, especially after long-term treatment, threatens dysbacteriosis. To return the stomach and intestines to a healthy state, it is strictly necessary to take probiotic products that will restore the bacterial level.
You can use the following tools:
- Enterol;
- Fluvir;
- Hilak Forte;
- Linux;
- Acipol;
- Hilak;
- Lactobacterin;
- Olin.
Normalization of motor skills
Colitis constantly causes spasms and pain that you cannot get used to. Some spasms continue after successful therapy. This is caused by the conditioned reflex action of the gastrointestinal tract, when contraction occurs “out of habit.”
To normalize the gastrointestinal tract system and not worry about it, use the following drugs from the group of prokinetics and antispasmodics:
Vitamin intake
To restore balance in the gastrointestinal tract and activate the restoration process in the mucous membrane of the colon, you need the presence in it of the required amount of fatty acids (proteins, fats, carbohydrates), mineral salts (sodium, calcium, phosphorus, magnesium, iodine) and vitamins B, F, PP , P, D, E and others.
Can be used as pure vitamins sold in pharmacies, or vitamin complexes:
- Supradin;
- Multi-tabs;
- Duovit;
- Vitrum;
- Centrum;
- Alphabet.
Optimum Nutrition vitamins are good for quick recovery. There is a division for men and women. This vitamin complex has a high concentration of vitamins and is sufficiently purified for better absorption by the body.
How long does medication treatment last?
Since colitis is not an ordinary disease, treatment takes quite a long time. Success can only be achieved with full compliance with the instructions of the attending physician.
So, treatment can last from a month to six months, after which it is necessary to maintain your body for a long time on vitamins and probiotic supplements, which will ensure a healthy state of the gastrointestinal tract.
– Treatment of intestinal colitis with medications
Conclusion
Colitis is an inflammatory bowel disease that threatens the body with more dangerous complications than cramps and diarrhea. To cope with it, you must follow the doctor's instructions.
Here are 7 simple points that we would recommend you follow:
- Take medications on time.
- Follow a diet.
- Do not take antibiotics and probiotics at the same time.
- Do not abuse analgesics.
- Don't delay going to the doctor.
- Try to stick to your daily routine.
- Do not combine traditional and traditional medicine.
Don't forget that your intestines and stomach determine your overall health and often signal that something is wrong with your body systems. Listen to yourself and try to pay attention to any worries.
Source: https://gastrocure.net/bolezni/kolit/lecheniyu-kolita-medikamentoznymi-sredstvami.html
The use of antibiotics for dysbacteriosis
When dysbiosis develops, medications from the group of antibiotics are prescribed to suppress pathogenic bacteria. Most often, drugs from the following groups are recommended for use:
- penicillins;
- tetracyclines;
- cephalosporins;
- quinolones.
Metronidazole may also be prescribed.
Since antibiotics already have a detrimental effect on the state of the microflora of the digestive tract, they are used for dysbiosis of the small intestine, accompanied by malabsorption syndrome and motility disorders.
The following drugs are most often prescribed for the treatment of dysbiosis:
- Amoxicillin. A semi-synthetic drug from the penicillin group. Gives good results when taken orally, as it is resistant to the aggressive gastric environment.
- Alpha Normix. Non-systemic broad-spectrum antibiotic. The active substance is rifaximin. Indicated for dysbiosis caused by diarrhea and infectious pathologies of the gastrointestinal tract.
- Flemoxin Solutab. Semi-synthetic drug of the penicillin group. Has a bactericidal effect.
- Levomycetin. Broad-spectrum antimicrobial agent. Prescribed for the treatment of dysbacteriosis caused by intestinal infection and pathologies of the abdominal organs. It can also be prescribed as an alternative drug if previously selected medications have not given a positive result.
With the development of dysbiosis of the large intestine, the following are prescribed:
The drugs are effective against yeast, staphylococcus and proteus, which are the main cause of colon dysbiosis. The drugs do not have a significant effect on the state of natural microflora.
Antibiotics that cause diarrhea
Penicillins
Penicillins of earlier generations (ampicillin, benzylpenicillin) more often affect the intestinal microflora. The use of modern penicillins does not lead to the development of clostridia - the main culprits of pseudomembranous colitis.
Cephalosporins
Most cephalosporins promote the growth of enterobacteria and clostridia. Cefaclor and cefradine do not affect the intestinal biocenosis.
Erythromycin
M-cells of the epithelium of the small intestine produce the hormone motilin, which affects intestinal motility, promoting the movement of food through the digestive tract. Erythromycin stimulates the production of motilin, thereby accelerating the emptying of the stomach and intestines, which is manifested by diarrhea (diarrhea).
Clavulanic acid
Clavulanic acid, which is part of many antibiotics (amoxiclav, amoxicillin/clavulanate), also stimulates intestinal motility.
Tetracycline and neomycin negatively affect the intestinal epithelium, causing a direct toxic effect.
Fluoroquinolones
Antibiotics of this group suppress the growth of normal intestinal microflora, but do not promote the growth of clostridia.
Lincomycin
If a patient has loose stools for 2 days in a row, two days after starting antibiotics and up to 2 months after stopping them, antibiotic-associated diarrhea (AAD) occurs. This condition means that the patient has experienced pathological changes in the composition of the intestinal microflora (intestinal dysbiosis). Its incidence ranges from 5 to 25% among patients treated with antibiotics.
If diarrhea occurs with symptoms of intoxication and high leukocytosis, then clostridia should be considered the cause.
Rice. 5. The bulk of the intestinal microflora is concentrated in the parietal zone of the intestine.
Those at risk for developing antibiotic-associated diarrhea are:
- children aged from 2 months. up to 2 years old and adults over 65 years old,
- patients with diseases of the stomach and intestines,
- patients who were treated with antibiotics for more than 3 days,
- use in the treatment of a large number of antibiotics,
- severe immunodeficiency.
Uncontrolled use of antibiotics contributes to the development of dysbacteriosis and increases the allergenicity of the body. The risk of developing diarrhea after antibiotics is not affected by the method of administration of antibiotics or their dosage. Cases have been described in which diarrhea developed even after a single dose of broad-spectrum antibiotics.
Antibiotics for colitis
Treatment of colitis of bacterial origin is impossible without a course of antibiotics. For nonspecific ulcerative inflammation of the colon, medications of this category are prescribed in the event of a secondary bacterial infection.
In the process of treating pathology, the following can be used:
- group of sulfonamides for mild/moderate disease;
- broad-spectrum agents for severe disease.
In order to prevent the development of dysbiosis, the patient is recommended to take probiotics. This could be Nystatin or Colibacterin. The latter contains live E. coli, which contribute to the restoration and normalization of microflora.
For colitis, the following medications may be prescribed:
- Alpha Normix. A broad-spectrum agent with a pronounced bactericidal effect, which helps reduce the pathogenic load.
- Furazolidone. A drug from the nitrofuran group. Has an antimicrobial effect.
- Levomycetin. The product is active against pathogenic microflora and also exhibits a bactericidal effect. Since numerous side symptoms may develop while taking Levomycetin, the dosage and treatment regimen should be selected individually. Intramuscular administration of the drug is possible.
Self-treatment of colitis with antibiotics is completely unacceptable. A qualified specialist must select medications and determine the dosage regimen. It is also necessary to inform the doctor about all medications taken in order to exclude the development of negative reactions due to drug interactions.
Treatment
Diet
With severe diarrhea, the first one to three days of the disease are hungry. In this case, it is necessary to consume a large amount of clean liquids (rosehip decoction, diluted unsweetened tea, water).
On the second or third day, when diarrhea subsides, it is recommended to slightly expand the table, consuming kefir (three days old) and unsweetened jelly. Then add pureed cottage cheese and go to table 4a, recommended for patients with acute enterocolitis.
During the recovery period, the diet is gradually expanded and they switch to a common table with the exception of alcohol, spices, pickles, smoked and canned foods, fatty meats, and baked goods.
It should be remembered that complete restoration of the intestinal mucosa occurs some time after all the symptoms of the disease disappear. Therefore, in the case of pseudomembranous colitis, it is necessary to adhere to dietary restrictions even after all the symptoms of the disease have disappeared.
If the disease is extremely severe, you have to resort to parenteral nutrition.
Etiotropic treatment
If severe diarrhea occurs, suspicious for pseudomembranous colitis, immediate cessation of antibiotic therapy is necessary.
Indications for etiotropic treatment of pseudomembranous colitis - that is, therapy aimed at destroying the microbe that causes the disease - are related to the severity of the disease.
According to current recommendations, asymptomatic carriage of Clostridium difficile cannot be treated. Therefore, in mild cases, when the symptoms of the disease disappear after stopping antibiotics, etiotropic therapy is not prescribed.
In severe and moderate forms, when diarrhea occurs that continues after discontinuation of antibiotic therapy, as well as in case of relapses of pseudomembranous colitis, etiotropic treatment is prescribed.
Clostridium difficile is sensitive to vancomycin and metronidazole. Moreover, metronidazole is usually prescribed as a standard. Vancomycin is a first-line etiotropic drug that is used in the presence of contraindications to metronidazole (severe liver damage, serious pathology of the nervous system, low white blood cell count, individual intolerance to the drug).
The advantage of metronidazole is the possibility of intravenous administration, which is necessary in severe cases. In addition, vancomycin is not recommended as a first-line drug, so as not to cause resistance of gram-positive microflora to it. Today, vancomycin is one of the few drugs successfully used against strains of staphylococci resistant to many antibiotics.
Correction of dysbiosis in pseudomembranous colitis
Treatment of dysbacteriosis in pseudomembranous colitis refers to etiotropic therapy. This therapy is prescribed for all forms of the disease to normalize intestinal function and prevent relapses.
Long courses (20-25 days) of bacterial preparations such as colibacterin, bifidumbacterin and bificol are indicated. In this case, the dosage should be twice as high as in the case of treatment of ordinary dysbiosis (up to 10 doses twice a day).
Therapy for dysbiosis is prescribed immediately after completing courses of antibacterial therapy, and if antimicrobial drugs were not prescribed, then immediately after stool normalization.
Pathogenetic therapy
Pathogenetic treatment is the therapy of the main syndromes of the disease. In case of pseudomembranous colitis, it is necessary to treat dehydration syndrome (dehydration of the body), correction of disturbances in protein and electrolyte metabolism, and detoxification therapy (treatment of general poisoning of the body).
In case of severe dehydration, parenteral (intravenous) administration of Ringer's, Hartmann's, and lactosol solutions is prescribed. The administration of solutions is carried out under the control of diuresis (a decrease in urine volume indicates the degree of dehydration). In some cases, it is necessary to administer up to 8 liters of rehydration solutions per day.
In severe cases of pseudomembranous colitis, significant protein losses occur, which are compensated for by intravenous administration of an albumin solution or human plasma.
If severe diarrhea has led to disruption of electrolyte metabolism, then after restoration of normal diuresis, solutions of potassium chloride are administered under the control of an ionogram.
To reduce intoxication syndrome, oral administration of cholestyramine is indicated. This drug binds to bacterial toxins and removes them from the body.
However, it should be remembered that cholestyramine sharply reduces the effect of oral antibacterial therapy, so it is prescribed either in severe cases - when metronidazole is administered intravenously, or in relatively mild cases of pseudomembranous colitis - when antibacterial therapy is not carried out.
Symptomatic therapy
Surgery
Surgical treatment of pseudomembranous colitis is carried out in the event of the development of complications such as toxic dilatation of the intestine and perforation of the intestine.
Another indication for surgical intervention is an extremely severe course of the disease. So, if intensive therapy does not produce significant positive results within two days, they turn to surgical methods. In cases where the patient’s condition deteriorates catastrophically, despite all the measures taken, wait-and-see tactics are unacceptable, since death with this course of the disease can occur very quickly.
What antibiotics should I take for colitis?
Unfortunately, a large number of people prefer to independently diagnose and treat it rather than contact a specialist. This can lead to a large number of serious complications.
If you experience pain in the intestinal area, then you should immediately contact a gastroenterologist, who will prescribe a full examination, and if colitis occurs, prescribe you to take appropriate medications and diet to treat the disease. Not every type of colitis requires antibiotics, however, in severe forms of the disease there is no escape from this. What medications can be prescribed in conjunction with antibiotics? How to take them?
Diet for pseudomembranous colitis
Suspicion of pseudomembranous colitis requires immediate withdrawal of antibiotics and subsequent prescription of drugs that inhibit Clostridium difficile. The drug of choice is metronidazole, which in some cases is replaced by vancomycin. The principle of treatment in this case is to suppress the intestinal microflora as completely as possible and subsequent restoration of the microbiome characteristic of a healthy body.
It is very important to follow a proper diet during treatment for MVP. The principles of nutrition for colitis are as follows:
- Complete hunger for the first two to three days. During this period, large amounts of fluid should be consumed, and according to the doctor’s decision, the patient can be transferred to parenteral nutrition.
- When the diarrhea subsides, the use of kefir (two or three days old) and low-fat pureed cottage cheese are allowed.
- The patient is transferred to table 4a according to Pevzner, indicated as a diet for patients with diseases of the large intestine.
- After recovery, they switch to a common table, while flour, smoked, fatty foods and alcohol remain prohibited.
To prevent pseudomembranous colitis, you should take care of your own health, maintain your immune system and use antibiotics only under the supervision of a doctor.
Metronidazole for colitis
Metronidazole is an antiprotozoal and antimicrobial drug derived from 5-hydroimidazole. The effect is that the biochemical reduction of the 5-nitro group of metronidazole is carried out through intracellular transport proteins of the anaerobic microorganism.
The drug is not sensitive to aerobic microorganisms and facultative anaerobes, however, in the presence of a mixed type of microflora, it can act synergistically with an antibiotic that is effective against the usual type of aerobes.
It has its own contraindications, including diarrhea and loss of appetite, nausea, vomiting, intestinal colic, constipation, and a “metallic” taste in the mouth. Metronidazole is prescribed to patients with colitis, since after the use of antibiotics there are various kinds of complications or undesirable consequences of treatment.
The medication is prescribed only by the attending physician in accordance with the clinical picture of the patient, but often taking 500 mg 2 times a day for 3-5 days.
How to take Fthalazol for colitis?
Phthalazole is a sulfonamide drug that is slowly absorbed from the gastrointestinal tract. The underlying mass, after oral administration, will linger in the intestinal cavity, after which the active molecular parts will begin to break off. Greater effectiveness in the treatment of colitis is due to the fact that a high concentration of sulfonamide is created in the intestinal cavity together with the activity of the drug in relation to the intestinal flora.
Before prescribing Fthalazol together with antibiotics, the doctor determines the patient’s sensitivity level. What are the recommendations for taking Phthalazol for colitis:
- Adults: the first few days, 1-2 g every 4 hours, and the next 3 days, half the dose.
- For children, 1.1 g/kg per day is prescribed on day 1. The drug is given in equal doses at intervals of 4 hours and at night. The subsequent dose will be 0.2-0.5 g with a break of 6-8 hours.
Alpha Normix for colitis
Alpha Normix is an antibiotic that has a broad spectrum antibacterial effect. It is a bactericidal drug prescribed for colitis. It binds to the beta subunits of bacterial enzymes and can inhibit the synthesis of RNA and bacterial proteins. Due to this, bactericidal properties are manifested in relation to the sensitivity indicator of bacteria.
Thanks to the antibacterial spectrum of Alpha Normix for colitis, it is possible to reduce pathogenic intestinal bacterial loads that cause some pathological conditions. This drug may reduce:
- Ammonia formation caused by bacteria.
- Increased level of proliferation.
- The presence of bacteria in the colon cavity.
- Antigenic stimulation.
- Risk of infectious complications.
Alpha Normix is taken orally. For adults, 1 tablet every 8 hours. Treatment does not exceed 7 days and should be determined by the patient’s clinical picture. The frequency and dose may be changed by your doctor.
Levomycetin for colitis
The drug is an antibiotic that is effective against a wide range of gram-positive and gram-negative microorganisms. It has a pronounced bacteriostatic effect, and at high concentrations it exhibits a bactericidal effect against some strains. After oral administration, the antibiotic is quickly absorbed into the gastrointestinal tract.
Levomycetin is available in two forms: tablets and powder for injection dilution. Tablets are taken half an hour before meals, 250-500 mg for adults. For children, the recommended dose is 125 mg 4 times a day.
The antibiotic powder is diluted with 2-3 mg of water for injection intramuscularly. The duration of treatment with Levomycetin for colitis is determined only by a doctor.
Furazolidone for colitis
Furazolidone is an antibacterial drug of the nitrofuran group, a synthetic derivative of 5-nitrofurfural, which has a pronounced antimicrobial interaction against gram-negative aerobic microorganisms. They are to a small extent sensitive to the effects of antibiotics on gram-positive aerobic microorganisms.
The pharmacological effect of Furazolidone in colitis directly depends on what dose was used, and if small doses are used, then it simply turns out to be bacteriostatic.
The drug is taken orally. The tablet is swallowed whole, it does not need to be chewed or crushed, and is washed down with plenty of water. The drug is taken after eating. The duration of treatment for colitis with Furazolidone and the dose should be prescribed only by a doctor.
Whatever your symptoms of the disease, all antibiotics for colitis must be prescribed strictly by a specialist.
Diarrhea and colitis after antibiotics
When treated with antibiotics, the number of microbes sensitive to them decreases and the growth of normal intestinal microflora is inhibited. The number of antibiotic-resistant strains is increasing. Opportunistic bacteria multiply rapidly and begin to acquire properties that damage the macroorganism.
Clostridia, staphylococci, Proteus, enterococci, Pseudomonas aeruginosa, Klebsiella and yeast-like fungi are the most well-known representatives of pathogenic intestinal flora. In most cases of diarrhea that occurs after antibiotics, the leading place is occupied by clostridia (Clostridium difficile). The frequency of their damage is:
- from 15 to 30% of cases with antibiotic-associated diarrhea (AAD);
- from 50 to 75% of cases with antibiotic-associated colitis;
- up to 90% of cases with pseudomembranous colitis.
Rice. 2. Photo of Clostridium difficile under a microscope.
Rice. 3. The photo shows a colony of Clostridium difficile.
The cause of diarrhea (diarrhea) and colitis is a violation of the intestinal microbiocenosis (intestinal dysbiosis). The growth of pathogenic bacteria leads to damage to the intestinal wall and increased secretion of electrolytes and water.
Intestinal microflora is involved in the utilization of fiber. As a result of this process, short-chain fatty acids are formed - a source of energy for the intestinal mucosa.
With an insufficient amount of fiber in the human diet, the trophism (nutrition) of intestinal tissues is disrupted, which leads to increased permeability of the intestinal barrier to toxins and pathogenic microbial flora.
Enzymes produced by intestinal microflora take part in the process of breaking down bile acids. After being released into the gastrointestinal tract, secondary bile acids are reabsorbed, and a small amount of them (5 - 15%) is excreted in the feces, participating in the formation and movement of feces and preventing their dehydration.
If there are too many bacteria in the intestines, then bile acids begin to break down prematurely, which leads to secretory diarrhea (diarrhea) and steatorrhea (excretion of increased amounts of fat).
All of the above factors form:
- Antibiotic-associated diarrhea is the most common complication of antibacterial treatment in adults. The incidence of this complication ranges from 5 to 25% in people taking antibiotics;
- The development of colitis is somewhat less common;
- A rare but serious disease that develops after antibiotics is pseudomembranous colitis.
Rice. 4. The photo shows a normal intestinal wall (histological specimen).
What antibiotics should I take for colitis?
Unfortunately, a large number of people prefer to independently diagnose and treat it rather than contact a specialist. This can lead to a large number of serious complications.
If you experience pain in the intestinal area, then you should immediately contact a gastroenterologist, who will prescribe a full examination, and if colitis occurs, prescribe you to take appropriate medications and diet to treat the disease. Not every type of colitis requires antibiotics, however, in severe forms of the disease there is no escape from this. What medications can be prescribed in conjunction with antibiotics? How to take them?
Metronidazole for colitis
Metronidazole is an antiprotozoal and antimicrobial drug derived from 5-hydroimidazole. The effect is that the biochemical reduction of the 5-nitro group of metronidazole is carried out through intracellular transport proteins of the anaerobic microorganism.
The drug is not sensitive to aerobic microorganisms and facultative anaerobes, however, in the presence of a mixed type of microflora, it can act synergistically with an antibiotic that is effective against the usual type of aerobes.
It has its own contraindications, including diarrhea and loss of appetite, nausea, vomiting, intestinal colic, constipation, and a “metallic” taste in the mouth. Metronidazole is prescribed to patients with colitis, since after the use of antibiotics there are various kinds of complications or undesirable consequences of treatment.
The medication is prescribed only by the attending physician in accordance with the clinical picture of the patient, but often taking 500 mg 2 times a day for 3-5 days.
How to take Fthalazol for colitis?
Phthalazole is a sulfonamide drug that is slowly absorbed from the gastrointestinal tract. The underlying mass, after oral administration, will linger in the intestinal cavity, after which the active molecular parts will begin to break off. Greater effectiveness in the treatment of colitis is due to the fact that a high concentration of sulfonamide is created in the intestinal cavity together with the activity of the drug in relation to the intestinal flora.
Before prescribing Fthalazol together with antibiotics, the doctor determines the patient’s sensitivity level. What are the recommendations for taking Phthalazol for colitis:
- Adults: the first few days, 1-2 g every 4 hours, and the next 3 days, half the dose.
- For children, 1.1 g/kg per day is prescribed on day 1. The drug is given in equal doses at intervals of 4 hours and at night. The subsequent dose will be 0.2-0.5 g with a break of 6-8 hours.
Alpha Normix for colitis
Alpha Normix is an antibiotic that has a broad spectrum antibacterial effect. It is a bactericidal drug prescribed for colitis. It binds to the beta subunits of bacterial enzymes and can inhibit the synthesis of RNA and bacterial proteins. Due to this, bactericidal properties are manifested in relation to the sensitivity indicator of bacteria.
Thanks to the antibacterial spectrum of Alpha Normix for colitis, it is possible to reduce pathogenic intestinal bacterial loads that cause some pathological conditions. This drug may reduce:
- Ammonia formation caused by bacteria.
- Increased level of proliferation.
- The presence of bacteria in the colon cavity.
- Antigenic stimulation.
- Risk of infectious complications.
Alpha Normix is taken orally. For adults, 1 tablet every 8 hours. Treatment does not exceed 7 days and should be determined by the patient’s clinical picture. The frequency and dose may be changed by your doctor.
Levomycetin for colitis
The drug is an antibiotic that is effective against a wide range of gram-positive and gram-negative microorganisms. It has a pronounced bacteriostatic effect, and at high concentrations it exhibits a bactericidal effect against some strains. After oral administration, the antibiotic is quickly absorbed into the gastrointestinal tract.
Levomycetin is available in two forms: tablets and powder for injection dilution. Tablets are taken half an hour before meals, 250-500 mg for adults. For children, the recommended dose is 125 mg 4 times a day.
The antibiotic powder is diluted with 2-3 mg of water for injection intramuscularly. The duration of treatment with Levomycetin for colitis is determined only by a doctor.
Furazolidone for colitis
Furazolidone is an antibacterial drug of the nitrofuran group, a synthetic derivative of 5-nitrofurfural, which has a pronounced antimicrobial interaction against gram-negative aerobic microorganisms. They are to a small extent sensitive to the effects of antibiotics on gram-positive aerobic microorganisms.
The pharmacological effect of Furazolidone in colitis directly depends on what dose was used, and if small doses are used, then it simply turns out to be bacteriostatic.
The drug is taken orally. The tablet is swallowed whole, it does not need to be chewed or crushed, and is washed down with plenty of water. The drug is taken after eating. The duration of treatment for colitis with Furazolidone and the dose should be prescribed only by a doctor.
Whatever your symptoms of the disease, all antibiotics for colitis must be prescribed strictly by a specialist.
Description of the causative agent of the disease
Pseudomembranous colitis and its symptoms were first described by the American surgeon John Finey back in 1893, when he operated on a seriously ill woman who developed severe diarrhea after the operation, which led to her death two weeks later. When opening the colon, fibrous membranes were discovered, which gave the name to the disease. Typically, before doctors began using antibiotics when treating patients, cases of pseudomembranous colitis were quite rare.
To date, the causative agent of this disease, its symptoms and necessary treatment have been well studied, and it is a mobile microorganism of the anaerobic type, whose toxins provoke the described syndrome. The key toxins in this case are enterotoxin A and cytotoxin B. and, although both of them are actively involved in the process of colitis, it is the first of them that plays the main role at the early stage of the disease.
The bacteria Clostridium difficile lives in the intestines of many animals, as well as in the human intestines, making up about one hundredth of all microorganisms living there. It is curious that virulent strains of this infection are most often found in children, who are least likely to develop pseudomembranous colitis. The reason is the fact that in the epithelium of their intestines there are no receptors that could be affected by Clostridium difficile, while children have protective antibodies acquired from the mother.
The peculiarity of this type of microbes is their resistance to environmental conditions, including elevated temperatures, which makes it a significant problem that they are spread throughout the hospital on the clothes and hands of staff (or visitors). Sometimes this even leads to local outbreaks of the disease within a single medical facility. This also explains the fact that about 10% of all patients with pseudomembranous colitis were not treated with antibiotics (which is usually included in the classic symptoms).
Vaccination against rotavirus infection - live vaccine
Both the doctor and the patient should remember that the likelihood of developing the disease in question is not affected by either the dose or the method of using the antibiotic. Moreover, even a single dose can serve as a sufficient reason for the activation of Clostridium difficile.