More about the disease
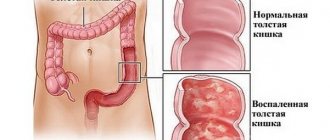
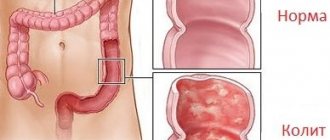
One of the common diseases of the colon is colitis. The disease causes inflammatory-dystrophic changes in this organ. In newborns, the pathology also affects the small intestine, so they are diagnosed with enterocolitis. Regardless of the type, colitis causes problems with stool, abdominal pain and malaise. The disease is most often provoked by intestinal infections, but there are other reasons for its development.
Due to the anatomical and physiological characteristics of the digestive system of young children, the inflammatory process, as a rule, occurs with simultaneous involvement of the small and large intestines (enterocolitis). School-age children usually experience isolated damage to various parts of the intestine - enteritis and colitis.
Types of disease
Taking into account the morphological characteristics, colitis is divided into:
- atrophic,
- catarrhal,
- ulcerative-erosive.
According to the nature of the flow, it can be mild, moderate, or severe.
By type – monotonous, latent, progressive and recurrent.
The broadest classification divides colitis into the following types:
- primary;
- medicinal;
- nonspecific;
- parasitic (pseudomembranous);
- neurotic;
- nutritional;
- allergic;
- toxic;
- post-infectious;
- ray;
- spastic.
Acute, chronic, nonspecific ulcerative and spastic colitis are diagnosed more often in children - unlike adults.
There is another classification of this disease. Since the large intestine consists of several sections, colitis can have different localizations. Taking this criterion into account, the following are distinguished:
- typhlitis (inflammation of the cecum);
- transversitis (inflammation of the transverse colon);
- sigmoiditis (colitis of the sigmoid colon);
- pancolitis (generalized inflammatory process);
- proctosigmoiditis (colitis of the sigmoid and rectum);
- angulitis (inflammation of the transition of the transverse colon to the descending colon);
- proctitis (inflammation of the rectum);
- typhlocolitis (inflammatory process in the cecum and ascending colon).
Diagnostics
A pediatric gastroenterologist knows how to treat colitis in children and diagnose it, based on information obtained during a physical examination, laboratory and instrumental procedures.
Thus, the first stage of diagnosing pathology is aimed at:
- familiarizing the clinician with the medical history of not only the patient, but also his relatives - to identify the etiological factor that is most suitable for a particular person;
- collection and study of the child’s life history – this should include information regarding the course of the period of intrauterine development of the fetus;
- a thorough examination, involving palpation of the anterior wall of the abdominal cavity - to establish its location, which will indicate the affected part of the large intestine;
- a detailed survey of the patient or his parents is necessary to determine the intensity of clinical manifestations, which, in turn, will provide information about the severity of the inflammatory process.
The following laboratory tests are considered the most valuable:
- general and biochemical blood test;
- coprogram;
- bacterial culture of feces;
- analysis of stool for dysbacteriosis.
The last step of diagnostic manipulations is instrumental procedures, among which it is worth highlighting:
- colonoscopy and rectoscopy;
- endoscopic biopsy of the affected segment;
- X-ray of the intestine using a contrast agent;
- Ultrasound of the peritoneum;
- CT and MRI.
Examination of the large intestine - colonoscopy
Colitis in children should be differentiated from:
- celiac disease;
- intestinal dyskinesia;
- enteritis;
- cystic fibrosis;
- Crohn's disease;
- chronic inflammation of the appendix;
- diverticulitis.
Causes of pathology in children
The sources of intestinal inflammation in children are diverse. Acute colitis is most often provoked by pathogens of digestive tract infections:
- salmonella;
- retrovirus;
- rotavirus;
- Escherichia;
- Shigella
Also, an acute form of colitis develops as a result of gastritis of any nature, enteritis and gastroenteritis. Chronic is caused by dysentery, ascariasis, giardiasis, pancreatic dysfunction and poisoning with toxic substances. Risk factors for developing any form of colitis:
- long-term use of anti-inflammatory, laxative or antibacterial medications;
- severe food poisoning;
- poor nutrition;
- early introduction of complementary foods;
- intestinal damage by parasites (helminthic infestation);
- allergies of various nature;
- frequent stress, prolonged psycho-emotional shocks;
- autoimmune diseases;
- burdened heredity;
- sedentary lifestyle (in adolescence);
- bad habits of the mother during pregnancy; congenital anomalies in the structure of the intestine;
- intestinal dysfunction of unknown nature (in infants).
Symptoms
Symptoms of colitis in children in acute form manifest themselves in the form of nausea, weakness and elevated body temperature. The child complains of abdominal pain. Bowel movements occur up to 15 times a day. The stool is watery, greenish, mixed with blood. Symptoms of colitis in infants can be complicated by rectal prolapse and dehydration.
Symptoms of colitis in children in chronic form can worsen and subside depending on the phase of the disease and recovery. The dominant symptoms of colitis in a child are abdominal pain, bowel problems such as diarrhea and constipation. In some cases, there is a deterioration in the baby’s general well-being, exhaustion of the nervous system, headaches and chronic fatigue. Colitis can also cause lack of body weight, anemia and vitamin deficiency.
How to recognize?
A baby with acute colitis caused by infections is usually accompanied by signs of intoxication - the child has a high temperature, is weak, and feels nauseous. When the intestinal mucous membranes become inflamed, spasms begin, as a result of which the baby complains of abdominal pain and the urge to defecate, which may well be false.
Diarrhea can recur from 5 to 15 episodes per day . Fecal masses with inflammation in the large intestine have a watery structure, they are foamy, have an unpleasant odor, often greenish, dirty-brown, impurities of mucus are clearly visible in them, and in the hemorrhagic form, inclusions of blood.
The urge to defecate can be so frequent and strong that the development of complications in the form of rectal prolapse is possible.
But the main danger of colitis in its acute form lies not even in this, but in the possibility of dehydration. It is from this that most often death occurs in intestinal infections. The younger the child, the faster dehydration occurs . The baby's facial features become sharper, the baby is thirsty, he is very weak, the skin loses its elasticity, the lips, tongue and mucous membranes are dry. With severe loss of fluid, delirium, loss of consciousness, and convulsions are observed. Acute severe colitis is especially dangerous for infants and newborns.
You can suspect chronic colitis in a child by the characteristic alternation of periods of exacerbation and calm. Inflammation of the large intestine will manifest itself mainly as pain in the abdomen and upset stool.
It hurts mainly in the area near the navel, the pain is aching, unexpressed, and most often appears a short time after eating. Constipation may alternate with diarrhea. Fecal masses have the characteristic appearance, smell, color and consistency described above. In children prone to constipation, cracks may form in the anus.
Children with chronic forms of colitis slowly gain weight and often do not reach the age norm. They often complain of headaches, weakness, get tired quickly, and have trouble sleeping at night.
Features of the course of the disease in childhood
The clinical picture and causes of this disease in children differ significantly from adults, so the symptoms and treatment of intestinal colitis in children will be different.
Acute intestinal colitis in a child, the symptoms of which last more than two weeks, in case of ineffective treatment passes into the stage of chronic colitis. This condition is dangerous due to complications, for example, peritonitis, the development of adhesions, chronic diarrhea and much more. Therefore, treatment of symptoms of colitis in children should begin from the first days of the disease.
Acute colitis is most dangerous for children under one year of age. Allergic colitis is more common in infants, which develops in response to a certain type of allergen - lactose, a medication, a separate strain of bacteria, etc. It is important to identify the allergen and eliminate it completely. Otherwise, colitis in infants often leads to dehydration of the body against the background of repeated vomiting and diarrhea, followed by the development of seizures and even the death of the child.
Prevention and prognosis
To prevent the development of such a disease, you should:
- monitor the adequate course of pregnancy;
- provide rational nutrition to children in accordance with their age category;
- Do not give medications to children unless absolutely necessary;
- give up bad habits – applicable for teenagers;
- regularly show the child to the pediatrician to identify in the early stages the progression of those pathologies against which colitis develops.
Complex treatment provides a favorable prognosis for the disease, which is observed in the vast majority of cases. Chronic colitis in a child can often recur without following medical recommendations.
Features of the course of various types of colitis in children
Acute colitis
In the acute form, the child suffers from severe cutting pain in the abdomen, and the body temperature can rise to febrile (38.5-39°C). The disease is accompanied by pronounced intestinal symptoms - frequent stools (3-6 times a day), liquid, foamy, it may contain remnants of undigested food, as well as bloody and mucous inclusions. Sometimes the clinical picture is complicated by nausea and vomiting.
This condition is typical for the early stage, as well as for periods when the chronic form of the disease worsens due to the influence of external and internal factors. The cause of the appearance is often infection of the digestive tract with the pathogenic bacterium Helicobacter pylori.
Acute forms also include spastic colitis, a condition in which the intestines spasm more often than in other types of the disease. In this regard, the nature of the pain changes - they become paroxysmal. Among the symptoms of the disease there is also “sheep” feces - hard, with distinct individual segments.
Chronic colitis
Even with timely and adequate treatment, the acute form in most cases becomes chronic. At the same time, the symptoms become more blurred - the pain dulls, becomes aching, vomiting and nausea stop. After eating, belching appears, and in very young children - regurgitation. Signs of increased gas formation appear: a bloated abdomen, a feeling of fullness, periodic passing of gas.
If the patient systematically undergoes courses of treatment and follows a diet under parental supervision, chronic colitis can be asymptomatic, with rare exacerbations or without them at all. In this case, the intestinal mucosa is gradually restored, although complete regeneration is impossible.
Nonspecific ulcerative colitis
The most common form of the disease, the causes of which often remain unclear. Typically, ulcerative colitis in children develops as a result of a combination of genetic predisposition and nutritional disorders. Often the picture is intensified by other gastrointestinal diseases - gastritis, stomach ulcers, duodenitis, problems with the pancreas.
The disease received its name due to the similarity of its clinical picture with peptic ulcer of the stomach and duodenum, namely: mucosal degeneration, in which in some places the affected areas transform into ulcers. Sometimes these areas cover a large area of the intestine, but in most cases they are located fragmentarily. Ulcerative colitis can occur in chronic and acute forms.
Acute form
It is characterized by pronounced manifestations of the disease: severe pain in the left side of the abdomen, increased body temperature to febrile and subfebrile levels. During periods of exacerbation, the ulcerated areas open and begin to bleed. As a result, a laboratory analysis shows the presence of blood in the stool of a sick child, and his general condition worsens: weakness, apathy appear, appetite worsens, weight loss, and joint pain are observed.
Chronic form
Unlike acute, it proceeds more mildly, since during remission the intestinal mucosa tends to partially recover, ulcerative areas are covered with a new layer of epithelium. The disease can worsen due to inappropriate use of medications, non-compliance with diet, stressful situations, and overwork. Chronic colitis can be manifested by difficulties in bowel movements - constipation, false urge to defecate, sensations of incomplete bowel movement.
The danger of this form of the disease is that when the pronounced symptoms disappear, the child’s parents may mistakenly decide that the child has fully recovered and stop following the diet and undergoing examinations.
When examining the patient, swelling of the affected areas of the intestine is detected, destruction at different depths of the mucosa, in rare cases reaching the submucosal layer. Sometimes the inflammatory process is accompanied by the formation of polypous growths.
Infectious (allergic) colitis
This type of disease occurs as a complication of acute intestinal infections (most often when the gastrointestinal tract is affected by salmonella, shigella, streptococci), helminthic infestations, and fungi. The disease is characterized by a rapid onset and development, accompanied by vomiting, diarrhea, and severe abdominal pain. Among the reasons that provoke this mucosal pathology is long-term use of antibacterial drugs, especially in children under 6 years of age.
Accurate diagnosis of infectious colitis is difficult due to the often mixed etiology of the disease - a viral or bacterial infection is usually accompanied by chronic diseases of the digestive organs. To complete the picture, a wide range of laboratory tests, as well as a number of instrumental studies, are required.
Pseudomembranous colitis
One of the most severe types of infectious colitis is pseudomembranous colitis (PMC), the development of which is provoked by the bacterium Clostridium difficile. As with damage to other pathogenic microorganisms, MVP is characterized by an increase in the number of leukocytes in the blood, diarrhea of varying severity, a state of dehydration, and other manifestations of intoxication.
Intestinal colitis in children: how to identify and treat
Colitis is an inflammatory-dystrophic pathology that develops primarily in the human large intestine. In a child under one year old, colitis can affect the tissues of not only the large intestine, but also the small intestine.
This is due to the physiological structure of the gastrointestinal tract of a young organism. Often the disease develops due to harmful bacteria and viruses entering the digestive system.
They can enter through the nose or mouth.
What does ulcerative colitis look like?
So often, children become infected while eating. The cause of the development of colitis of the large intestine can be non-compliance with personal hygiene rules. It is enough to not wash your hands once before eating to introduce an infection into the gastrointestinal tract.
In addition to the main reasons for the development of pathology, it should also be noted that colitis can exhibit characteristic symptoms due to frequent stressful situations that the child has had to endure.
This can be severe emotional shocks, worries, or a prolonged nervous state.
The next reason is a poor diet. If a child at an early age does not eat several times a day, this leads to colitis and gastritis. It is quite harmful for newborn babies to eat too solid foods.
Colitis of the colon often occurs due to a hereditary connection.
If one of the parents previously had a similar pathology, then if the child is likely to develop it even if the nutritional rules or preventive measures are followed.
In medicine, there is a separate classification of colitis of the large intestine. Belonging to a certain type is revealed during the recording of the manifested symptoms, as well as after diagnosing the cause of the disease.
Colitis forms in the rectum
Allergic type colitis can be observed quite often in children. In this case, the cause of the pathology was an allergic reaction to a drug or food product. Allergic colitis occurs due to the high sensitivity of the child’s body to certain types of intestinal microflora bacteria.
Depending on the location of the signs of the disease and the causes of its occurrence in children, catarrhal, erosive-ulcerative, atrophic and chronic types of colitis can be identified.
Quite dangerous chronic colitis can develop due to helminthic infestations in the body, infection with certain parasites, and intoxication of the digestive system.
The chronic form is very dangerous, and this type of colitis is difficult to treat.
Treatment and prevention
Drug therapy is usually prescribed for effective treatment. One of the most common groups of drugs is antibiotics. It is aimed at destroying harmful pathogens. If the symptoms of the pathology worsen, it is necessary to prescribe complex treatment using antibiotics, enzymatic preparations, and probiotics.
You will also need anesthetics to reduce pain, restorative agents that will improve tissue regeneration in the affected area, and, if necessary, antipyretic drugs. If the result of the pathology is the causative agent of the allergy, then treatment is carried out with the use of antihistamines.
Treatment using traditional medicine recipes is common. Folk remedies are also used as preventive measures. With the next exacerbation of chronic colitis, it will be necessary to treat the patient simultaneously using traditional medicine and folk remedies.
Traditional medicine includes various decoctions, herbal teas, infusions and other compositions. Among the most effective traditional medicines for colitis are honey and propolis.
Diagnosis of colitis
Immediately after contacting a specialist, the diagnostician carries out a set of measures in order to make a diagnosis as quickly as possible. To avoid making a mistake, the doctor first clarifies the complaints in detail, notes their nature and combines the symptoms. This is followed by a careful examination of the child, starting with the skin, which is usually pale, with peripheral cyanosis at the fingertips.
Due to impaired absorption of vitamins in the intestines, increased fragility of hair, nails and dry skin occurs. During the conversation, a foul odor from the mouth is noted, caused by rotting processes in the intestines, and belching may occur. During palpation of the abdomen, painful sensations can be more accurately localized; under the doctor’s fingers, rumbling in different parts of the intestine and a feeling of fluid transfusion may occur.
After a physical examination, laboratory tests are prescribed, primarily scatological examination of stool, which reveals a large amount of undigested food. A culture is done, and in case of colitis, a large number of pathogenic colonies grow in Petri dishes, which indicates intestinal dysbiosis.
The gold standard in diagnosis is sigmoidoscopy and colonoscopy. During the examination of the rectum, sigmoid colon and a complete examination of the colon, areas of inflamed mucous membrane, the presence or absence of ulcerative defects, and characteristic plaques are determined. If particularly suspicious areas are detected in the intestine, a piece of tissue is taken using special forceps for histological examination.
As an additional study, doctors prescribe radiography of the colon with contrast - irrigography, the results of which can reveal the characteristic symptoms of colitis and a clear localization of inflammation.
Treatment of colitis in children
Colitis in children three years of age and older can be treated largely through changes in diet and general routine. It is important to make the child feel better and reduce the frequency of seizures. For this purpose, a diet is prescribed that excludes dairy products and is rich in meat, fish, and eggs. Babies under one year old who are artificially fed are transferred to hypoallergenic lactose-free formulas.
If the baby is fed breast milk, everything is more complicated. Here the etiology of the disease is initially determined. Allergic colitis in an infant requires immediate transfer of the baby to artificial formula or the introduction of a strict diet for the mother.
A diet to cure colitis in older children requires, during moments of exacerbation, to completely exclude all foods that interfere with the food processing process, negatively affect the mucous membrane and increase gas formation.
“Prohibited” foods include flour delicacies, crackers and chips, salty and spicy foods, fast-food, carbonated sweet water, sauces and seasonings, preservatives, coffee, chocolate. It is also better to refuse or minimally reduce the amount of legumes, raw fruits and berries, fatty meats, yeast, rice and corn in the diet.
It is advisable to build a daily menu for colitis in a child. It should include:
- soups based on boiled meat and vegetables;
- lean meat stew);
- porridge (buckwheat, barley, rolled oats are recommended).
Flour is not completely prohibited. Allowed are hard pasta, white bread made from rye flour, and bran rolls. Drinks made from herbs, tea, and jelly will be useful.
Nutritional features depending on the type of colitis in a child
Dysfunction of the colon often causes failure of bowel movements. Depending on whether the child has constipation or diarrhea due to colon dysfunction, the list of prohibited foods changes.
If there is no bowel movement for more than 3 days:
- soups with rich broth;
- mushrooms;
- pork;
- pasta;
- semolina;
- chocolate;
- strong tea;
- canned food;
- seasonings
For diarrhea:
- milk and fermented milk products;
- baking;
- candies;
- sugar;
- legumes;
- nuts;
- fresh fruits and raw vegetables;
- high-calorie, fatty foods.
Nutrition for ulcerative and nonspecific colitis
Nonspecific ulcerative colitis in children is characterized by damage to the mucous membrane of the colon. The patient's food with this disease should be of a soft consistency so that it is quickly absorbed by the body. Solid feces of the large intestine can injure the damaged mucosa, causing inflammatory processes. The patient should be offered food, boiled or steamed, always warm. Food should be protein and fractional.
List of prohibited products:
- semi-finished products;
- smoked meats;
- legumes;
- cabbage;
- radish;
- carrot;
- fruits.
Features of the diet for spastic colitis in children
Untreated spastic colitis often becomes chronic. To prevent this from happening, it is necessary, in accordance with the child’s age, to enrich his diet with foods rich in plant fiber. All kinds of cereals and black bread will be useful. If pain occurs, doctors recommend eliminating foods with coarse fibers for a while and introducing them into the diet gradually.
It is strictly forbidden to feed the child:
- dairy products;
- fatty meat;
- oil;
- sugar.
Products during exacerbation and in remission
If there is an exacerbation of colitis, food consumption should be reduced to a minimum, especially in the first day. If a child tolerates the lack of food normally, he should be offered only half a glass of rosehip decoction 5 times a day for 24 hours. In this way, they achieve rapid functional unloading of the intestines and rid the colon mucosa of the chemical and mechanical effects of food.
Next, the therapeutic diet involves the gradual introduction of pureed protein foods (broths with poultry meat, cottage cheese). You should not offer your child cold or fried food. Fermentation processes can be prevented by eliminating sugar, cereals, and bread from the diet.
At this time the following are prohibited:
- vegetables and fruits;
- milk;
- pickles, seasonings;
- carbonated drinks;
- fatty meats and fish;
- canned food
During the remission stage, the therapeutic diet can be expanded, but the products should be as natural as possible. Vegetables and fruits are baked, peeled, and wiped before consumption. Gradually introduce pasta and milk. Over time, ground food is replaced with crushed food, increasing the load on the intestines. If the body normally perceives innovations, add raw vegetables and fruits to the diet.
Ulcerative colitis and drug treatment
The main task during the therapeutic process is to partially or completely stop inflammation and weaken the effect of pathogenic microorganisms on the intestines. For this purpose, anti-inflammatory drugs are prescribed. The complexity of the process of ulcerative colitis in children depends on the symptoms and the effectiveness of treatment.
Medication adjustment of the patient’s condition includes taking the following medications:
- Glucocorticoids (especially effective for left-sided forms of colitis);
- Antibiotics (recommended at times of relapse, including with elevated body temperature).
In the absence of expected results from treatment, as well as in emergency cases, surgery is recommended for children with UC. Most patients do not require radical surgical intervention, but, according to statistics, in approximately 20-40 percent of cases, as pathogenic processes worsen, removal of part of the intestine is required.
Drug therapy
The diet for colitis in children is supported by medicinal substances. Drug treatment consists of several points:
- oral rehydration with water-salt solutions, folk decoctions of medicinal herbs and fruits. In cases where fluid intake is difficult, it is administered parenterally as part of medicinal solutions.
- antibacterial therapy with Metronisazole, Furazolidone, Enterofuril, Phthalazole, especially in severe generalized inflammation;
- use of bacteriophages: Sextaphage, coliproteus bacteriophage;
- enterosorption with activated carbon, Polysorb, Smecta, Enterodes;
- prescription of enzyme preparations: Creon, Mezim, Pancreatin;
- restoration of intestinal microflora with probiotics, Bifiform and Linex are often used;
- For constipation that is not corrected by diet, prokinetics are recommended: Loperamide.
Physiotherapeutic methods are often used, for example: electrophoresis with solutions of potassium and magnesium electrolytes on the intestinal area. Warming compresses, paraffin therapy and acupuncture are indicated. It is useful for recovering children to engage in physical therapy.
In very severe forms that cannot be treated with medication, resection is performed - amputation of a fragment of the intestine.
Complications and prognosis of colitis in children
Acute colitis in a child can be complicated by such local manifestations as the formation of hemorrhoids, anal fissure, weakening of the sphincter, leading to gas incontinence and involuntary defecation during physical exertion, coughing, sneezing.
More severe consequences include intestinal cancer and diverticulitis, intestinal bleeding, inflammation of the gallbladder and pancreas, liver disease, and trophic ulcers. Infectious colitis often entails the spread of infection throughout the digestive tract and throughout the body, as a result of which the child may experience complications in the form of stomatitis, sore throat, bronchitis, and pneumonia.
Colitis is a serious disease, often exacerbating, difficult to treat, entailing many complications, requiring systematic examination and treatment. However, with the right approach and following all the doctor’s recommendations, inflammation becomes chronic, which may not appear for several years.
In general, the prognosis for life is conditionally favorable, but complete recovery is impossible.
If colitis is quickly diagnosed and complete therapy is carried out, then there are no complications. Following nutritional recommendations after recovery and following personal hygiene rules allows you to achieve stable clinical and laboratory remission.
Prevention of colitis
Colitis in children can be mild, or it can quickly become severe. Therefore, if alarming symptoms occur, you should contact a pediatrician or pediatric gastroenterologist for treatment and medical examination.
To prevent the development of colitis in children, it is necessary to protect them from intestinal infections, food poisoning, helminthic infestations, and dysbacteriosis.
- The most important measures to prevent colon dysfunction are:
- A varied diet based on natural food with a sufficient amount of plant fiber in proportion to the child’s age.
- No stress or excessive physical activity.
- Maintaining hygiene.
- Timely sanitation of the large intestine at the first symptoms of the disease and medical examination if necessary.
Sources: https://www.krasotaimedicina.ru/diseases/children/colitis https://vrachmedik.ru/1414-kolit-u-detej.html zhkt.ru/kishechnik/kolit/u-rebenka-kolit.html lechigemor .ru/drugie-zabolevaniya/kishechnik/359-kolita-u-rebenka.html https://vse-pro-detey.ru/kolit-u-detej/ gastritam.net/bolezni/kolit/u-rebenka.html https http://sovets.net/18494-kolit-u-detej.html This material is exclusively subjective in nature and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/19/2020
Prevention
Preventive measures are aimed at preventing relapses of the disease. It is necessary to try to prevent the child from contracting intestinal infections that can provoke an exacerbation of UC.
You should not take medications without a doctor's prescription. Experts believe that drugs from the NSAID group contribute to the development of relapse.
An indispensable condition is compliance with the diet. Children must be provided with a protective regime: they are exempt from physical education lessons, labor camps and other stress. The best option is to study at home. Vaccination is carried out only according to epidemiological indications (after consultation with an immunologist) with weakened vaccines.
After discharge from the hospital, the child is registered with a pediatric gastroenterologist. If the disease lasts more than 10 years, annual colonoscopy with biopsy is indicated for timely detection of malignant degeneration of the intestinal mucosa.