What is ulcerative colitis?
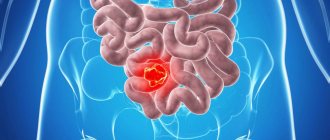
Ulcerative colitis is based on a chronic, recurrent inflammatory process that affects the mucous membrane of the large intestine. A feature of the pathology is the formation of numerous deep ulcers on the mucosa in individual segments or along the entire internal surface of the colon (Fig. 1). The location of the lesion determines the course of the disease.
Figure 1. Ulcerative colitis. The photograph shows white ulcers on the intestinal mucosa. Source: selvanegra
The pathological process usually begins in the rectal area, and in 20-30% of cases is limited to it.
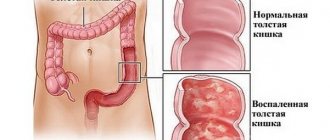
In half of the cases, inflammation spreads to the sigmoid, descending colon and transverse colon, and in the rest it covers the entire large intestine. What does the human large intestine consist of?
The large intestine is about two meters long. This is where the final absorption of nutrients from food and the formation of feces occurs. The large intestine is divided into 5 sections: the cecum (it is connected to the ileum of the small intestine) and the appendix, the colon (it is divided into 4 parts - ascending, transverse, descending and sigmoid), rectum and anus, ending in the anus (Fig. .2).
Figure 2. Structure of the large intestine. Source: CC0 Public Domain
Ulcerative colitis most often affects young men under 40 years of age, but the trend in recent years is an increase in the number of cases among children and the elderly. The geographical features of the prevalence of the pathology are interesting: in Australia, the USA and Canada there are 100-150 cases per 100 thousand population, while in Europe this figure does not exceed 15. Residents of African and Asian countries practically do not suffer from ulcerative colitis. In Moscow and the Moscow region, the number of diseases per 100 thousand population is fixed at 22-23 cases per 100 thousand population.
Mechanism of development of UC
In most cases, the development of UC begins in the rectal area. The inflammatory process gradually spreads to the entire surface of the mucous membranes of the large intestine. The disease is accompanied by two main stages, which periodically replace each other - the exacerbation phase and remission.
Forms of ulcerative colitis
Ulcerative colitis is divided into several types depending on the location of the pathological process and the characteristics of the course of the disease. According to the mechanism of development, UC can be continuous, recurrent and acute. In the first case, the symptoms of the pathology constantly bother the patient, in the second, exacerbation occurs periodically. Acute UC is a period of sudden onset of symptoms.
Forms of UC depending on location:
- distal type (inflammation affects the sigmoid and rectum, pain during the development of pathology is localized in the left iliac region);
- left-sided type (the inflammatory process is localized in the colon);
- pancolitis (pathological process affects all parts of the rectum);
- total form (the disease is accompanied by massive blood loss, the most dangerous form of UC);
- proctitis (pathology affects only the rectum).
Causes
Despite the long history of studying the causes of the disease, they are still not fully understood, and determining the etiology of ulcerative colitis is considered one of the most difficult problems of gastroenterology. There are several theories of the pathogenesis of the disease, which are based on factors of different nature:
- Genetic. As a result of long-term clinical studies, it was found that people who have one of their parents also suffered from this disease are more likely to suffer from ulcerative colitis. The genetic theory is based on the assumption that certain genes are mutated.
- Infectious. The inflammatory process in the large intestine can be caused by certain types of pathogenic microflora. In addition, ulcerative colitis may result from an excessive immune reaction to antigens of certain non-pathogenic bacteria present in the intestines.
- Autoimmune. According to some researchers, the cause of ulcerative colitis is the destruction of epithelial cells of the large intestine as a result of the formation of antibodies against self-antigens.
Predisposing factors for the occurrence of ulcerative colitis:
- unhealthy diet with excess animal protein and lack of dietary fiber;
- nervous tension;
- various viral infections;
- lack of vitamin D in the body;
- sedentary lifestyle, smoking, alcohol abuse.
Food allergies, for example, intolerance to nuts, milk, honey and other products, can also play a role in the occurrence of pathology.
Causes of development of nonspecific ulcerative colitis
The etiology of UC remains unknown, but medical practice identifies several factors that significantly increase the risk of developing this disease. Research has proven that a special risk group includes patients whose relatives have been diagnosed with pathologies of this type. UC can be transmitted at the genetic level and is a hereditary disease.
Other causes of UC:
- infectious factor (the pathological process is provoked by the active reproduction and activity of harmful microorganisms);
- progression of inflammatory processes (UC can be provoked by any disease of the digestive system in the absence of adequate therapy);
- autoimmune factor (impaired functioning of the immune system causes massive destruction of cells, the consequences can be inflammatory processes in the large intestine);
- stressful situations and serious errors in nutrition (factors are not direct causes of UC, but can increase the risk of development and progression of the pathology).
Classification
To determine the correct treatment tactics for ulcerative colitis, it is necessary to correctly classify the disease.
Classification is carried out on various grounds. Table 1. Classification of ulcerative colitis.
| Type of colitis | Characteristic |
| Proctitis (distal colitis) | Inflammation within 18 mm of the anal canal, affecting only the rectum |
| Left-sided colitis | Affects the area from the sigmoid colon to the left flexure of the rectum |
| Total (pacolite) | Includes subtotal colitis with inflammation of the left flexure of the colon |
The severity of the disease is divided into severe, moderate and mild, depending on the severity of symptoms during the exacerbation period, the presence of complications, and response to drug therapy.
With super-severe or extremely severe ulcerative colitis, diarrhea is observed more than 10-15 times a day, hemoglobin is noticeably reduced, and body temperature rises above 38 ° C.
Ulcerative colitis is also classified according to the presence of intestinal complications and extraintestinal manifestations, activity and some special indices. According to the nature of the course, acute and chronic colitis are distinguished.
Manifestations of the acute stage of ulcerative colitis are extremely painful: frequent bowel movements, admixtures of pus and blood in the stool, fever, nausea, weakness, severe abdominal pain. The serious condition can be aggravated by peritonitis (due to perforation of the intestine) and heavy bleeding.
Chronic ulcerative colitis
If colitis lasts more than six months, it is considered chronic. There are 2 types of chronic ulcerative colitis:
- Chronic with continuous course - the disease occurs without periods of remission. This form of colitis is characterized by functional disorders of the intestines, the appearance of lymphatic infiltrates in the mucosa and changes in metabolic processes.
- Chronic relapsing - periods of exacerbation are replaced by long-term remission. At the same time, during remissions the symptoms disappear, and during the period of exacerbation they return. During the active phase, the body temperature rises and blood is found in the stool.
More about the disease
Non-ulcerative intestinal colitis can develop due to all the same reasons as any other colitis. This pathology is assigned a code range from K50 to K52. The disease in question refers to non-infectious enteritis and colitis.
Chronic non-ulcerative colitis is a chronic inflammatory disease of the colon, characterized by the development of inflammatory-dystrophic, and with long-term existence, atrophic changes in the mucous membrane, as well as dysfunction of the large intestine.
The pathological process can involve both the entire colon (total colitis) and mainly its various sections (right-sided colitis, left-sided colitis, proctosigmoiditis, transversitis). Often chronic colitis is combined with chronic enteritis.
The incidence of nonspecific ulcerative colitis is about 50-80 cases per 100 thousand population. At the same time, 3-15 new cases of the disease are detected annually for every 100 thousand inhabitants. Women are more prone to developing this pathology than men; in them, UC occurs 30% more often.
Nonspecific ulcerative colitis is characterized by primary detection in two age groups: young people (15-25 years old) and older people (55-65 years old). But besides this, the disease can occur at any other age. Unlike Crohn's disease, ulcerative colitis affects only the mucous membrane of the large colon and rectum.
What is the danger of ulcerative colitis
Ulcerative colitis is associated with serious complications, some of which can be fatal.
In the worst case, fecal peritonitis develops, i.e. acute inflammation of the peritoneum due to contamination of the abdominal cavity with fecal microflora.
Signs of peritonitis are severe abdominal pain, nausea, vomiting, prolonged constipation, pale skin. It is difficult for the patient to move, his facial features become sharper.
Peritonitis requires urgent surgical intervention. After confirming the diagnosis using ultrasound or fluoroscopy, the abdominal cavity is opened, its sanitation is performed and the defect in the colon wall is sutured.
Important! The success of treating peritonitis directly depends on the time of seeking medical help. If you have severe abdominal pain, you should immediately call an ambulance and do not try to solve the problem with painkillers.
Complications
Other dangerous complications of ulcerative colitis:
- severe bleeding from the colon, development of anemia and shock due to significant blood loss;
- the appearance of malignant neoplasms at the site of ulceration (malignancy);
- damage to the inflamed mucosa by pathogenic intestinal microflora;
- purulent inflammation of nearby tissues.
Most complications of ulcerative colitis can only be treated with surgery. The decision about surgery is made by the attending physician based on a comprehensive examination.
Symptoms of Ulcerative Colitis
Ulcerative colitis is characterized by three leading syndromes caused by the inflammatory process in the colon (Fig. 3):
- problems with stool: diarrhea, visiting the toilet up to 20 times a day;
- impurities of blood and mucus in the stool;
- severe cutting, pulling pain in the abdomen and rectal area without excretion of feces.
Figure 3. Main symptoms of ulcerative colitis.
Photo: verywell Sometimes, at the beginning of the disease, ulcerative colitis is manifested by constipation, periodic abdominal pain and minor traces of blood in the stool. Such symptoms do not cause anxiety in a person, and he is in no hurry to see a doctor, mistaking the ailment for a common intestinal disorder.
The severity of symptoms depends on the severity and form of the disease. In the acute phase, local symptoms include high fever, weakness, aching muscles and joints, weight loss, lack of appetite; (in approximately 1% of cases) ulcerative colitis is accompanied by ophthalmological manifestations - conjunctivitis, anterior uveitis, episcleritis.
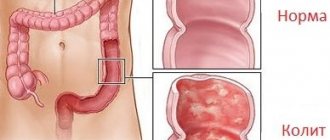
What does it look like
Nonspecific ulcerative colitis is detected by ulcerative lesions of the mucous membrane of the colon and rectum.
The prevalence, localization and exact picture of ulcerative lesions can be seen in the photo. In the left-sided type of the disease, damage to the mucous membrane of the descending and sigmoid areas is observed. With the total type, the inflammatory process is widespread throughout the intestine.
With proctitis, you can see how the inflammation spreads to the anus, localizing in the rectal area.
Diagnostics
In diagnosing ulcerative colitis, it is important to distinguish it from other inflammatory diseases with similar symptoms. The diagnostic complex includes a number of mandatory activities, including various laboratory and instrumental studies.
Which doctor should I contact?
The first stage of the examination is a conversation with a gastroenterologist. Taking an anamnesis includes determining the hereditary predisposition to the disease, determining the nature of the complaints, the color of the blood contained in the stool, its quantity, localization of pain, etc.
During the examination, the condition of the mucous membrane of the eyes is determined and the abdomen is palpated. This procedure can identify areas of increased sensitivity and possible enlargement of the colon.
Laboratory research
Laboratory tests include:
- General blood analysis. Particular attention is paid to the level of hemoglobin, the number of leukocytes and red blood cells.
- A biochemical blood test that allows you to identify the inflammatory process (reactive protein), the level of gamma globulins to assess the amount of antibodies.
- An immunoassay to determine the immune response to antibodies.
- Analysis of stool for bacteria, mucus and blood.
To determine the nature of the inflammatory process and its localization, the following is prescribed:
- Endoscopy of the large intestine. The procedure requires physiological and psychological preparation of the patient, as it is accompanied by discomfort and unpleasant sensations. Endoscopy can detect swelling and redness of the mucosa, its structure and bleeding, the presence of blood or pus in the large intestine. The sigmoid colon is examined using rectosigmoidoscopy.
- Colonoscopy is an examination of the large intestine to assess the extent of the pathological process and exclude other diseases, in particular malignant tumors.
- X-ray - to identify possible complications, for example, perforation of the intestinal wall, as well as to assess the condition of the mucosa, the presence of erosions and pseudopolyps.
- Irrigography is a study using contrast to clarify the diagnosis.
Based on the results of a comprehensive study, the doctor prescribes an individual treatment regimen. In severe cases, the patient can only be helped by emergency surgery.
Diagnosis of UC
To confirm nonspecific ulcerative colitis, it is necessary to conduct a series of examinations of the patient. A gastroenterologist diagnoses the disease. A general and biochemical blood test is mandatory. According to this study, the level of leukocytes, hemoglobin and other vital substances is determined. Next, the patient should undergo an endoscopic examination (this technique has the highest degree of effectiveness for UC).
Endoscopic diagnosis of UC
Endoscopy of UC is carried out in several ways. All procedures involve some preparatory steps. The patient should not eat food for twelve hours before the examination. To improve the quality of the procedure, it is recommended to do several enemas (cleaning the intestines of feces will allow you to get a clearer image). The purpose of endoscopic diagnosis of UC is to determine the degree of damage to the mucous membranes, identifying bleeding, pus and pseudopolyps.
Types of endoscopic diagnostics:
- colonoscopy (the study is aimed at all parts of the large intestine);
- Rectosigmoidoscopy (method for studying the condition of the sigmoid and rectum).
Additional methods for diagnosing nonspecific ulcerative colitis are X-ray examination with contrast, CT and MRI. An x-ray is necessary to rule out or confirm intestinal perforation. CT and MRI scans allow the doctor to visually examine the digestive organs. These techniques are prescribed at the discretion of the specialist.
Laboratory and serological markers
Laboratory and serological tests are a mandatory step in diagnosing the disease. Based on certain deviations in the research data, the doctor determines the presence of an inflammatory process and draws up a general clinical picture of the patient’s condition. Tests may be repeated at different stages of therapy to monitor the trend towards recovery.
Necessary tests:
- histological studies;
- coprogram;
- general and biochemical blood test;
- molecular genetic research;
- immunological blood test;
- bacterial culture and C-reactive protein;
- fecal calprotectin test.
Ulcerative colitis activity indices
For clinical practice, it is necessary to describe the activity indices of ulcerative colitis. The mild form is bloody stool up to four times a day. Moderate type - stool up to six times a day. In severe cases, stool occurs more than six times a day, and the patient's condition is worsened by tachycardia and fever. Acute colitis (fulminant type) develops with symptoms of anemia, stool occurs more than ten times a day.
Treatment
Difficulties in the treatment of ulcerative colitis are associated with the unclear etiology of the disease, therefore the main goal of therapeutic measures is to relieve symptoms, achieve stable remission, prevent relapses, improve the quality of life and alleviate the physical and psychological condition of a person.
The treatment regimen is developed strictly individually depending on the phase and nature of the disease, the condition of the colon, duration of the disease, severity of symptoms, response to previous treatment, allergic status, risk of complications and a number of other factors.
The therapy complex includes:
- drug treatment;
- strict adherence to the diet;
- psychological support;
- surgical treatment for complications and lack of effect from other methods.
Medications
Drug therapy includes four main groups of drugs:
- glucocorticosteroids;
- non-steroidal anti-inflammatory drugs based on 5-aminosalicylic acid;
- immunosuppressants;
- genetically engineered biological products (GEBP).
In addition, symptomatic medications are prescribed: antidiarrheals, painkillers, drugs to replenish iron in the body, vitamins B and C and some others.
The form and duration of taking each type of medicine is selected strictly individually.
Important! Ulcerative colitis is a dangerous inflammatory disease; self-medication is absolutely unacceptable. Uncontrolled use of medications can lead to serious complications and significantly worsen the situation.
Diet
Diet plays a decisive role in the treatment of ulcerative colitis. In the acute phase, with pronounced symptoms, complete fasting with permission to drink only clean water may be recommended. The ban on food intake is tolerated by patients without problems, since during an exacerbation they lose their appetite for natural reasons. In especially severe cases, parenteral nutrition (intravenous administration of a solution with nutrients) is prescribed.
The diet for ulcerative colitis is aimed at normalizing the condition of the intestinal mucosa and stopping diarrhea. The most irritating to the mucous membrane are spicy, sour foods, marinated dishes, large amounts of fiber and roughage, and any alcoholic drinks.
For intestinal inflammation, foods high in protein of animal and plant origin are recommended. The amount of protein in the daily diet is calculated based on the norm of 1.5-2 grams per kilogram of weight. The main sources of protein are lean meat, boiled and baked fish, eggs, and legumes. It is not recommended to fry foods, as dishes prepared in this way severely irritate the mucous membranes of the stomach and colon.
Recommendation During the period of exacerbation, many people develop intolerance to milk, so it is advisable to exclude dairy products and dishes based on them.
The optimal menu for ulcerative colitis corresponds to dietary table No. 4. The diet includes soups based on fish broth or lean meat, steamed minced meat dishes, porridge with water, pureed apples, boiled eggs, butter (no more than 5 grams per day), green tea, rosehip decoction and some other dishes and drinks.
Important! Any violation of the diet for ulcerative colitis threatens to worsen the disease!
Folk remedies
Folk remedies cannot be the main ones; they are only a way to alleviate the patient’s condition, but not a replacement for therapy. However, after consulting a doctor, to relieve symptoms of colitis, you can take decoctions of medicinal plants that have an anti-inflammatory effect and normalize stool. For example, to relieve symptoms of inflammation, a decoction of chamomile, an infusion of willow bark, and licorice root syrup are widely used, and to stop diarrhea, infusions and decoctions of oak bark, St. John's wort, quince fruits and seeds, and pomegranate peels are widely used.
Surgery
Surgical treatment is indicated if there is no effect from a strict diet and medications. Emergency surgery is indicated for suspected massive bleeding, peritonitis and the development of other complications.
During the operation, a resection of the large intestine is usually performed and the free end of the ileum is connected to the anal canal. If the situation allows, resection is performed partially while preserving intact areas of the colon. Surgical treatment is indicated in approximately 20% of patients.
Forecast
The prognosis for ulcerative colitis depends on the severity of the course, the presence of complications and concomitant diseases. With a mild form of the pathology and supportive anti-inflammatory therapy, more than 80% of patients do not experience relapses within a year. The risk of developing malignant neoplasms is limited to 3-10%.
Diet
Diet for ulcerative colitis is an important part of treatment. Experts recommend that patients adhere to the requirements of a specially formulated diet constantly, in order to avoid relapses and exacerbation of the disease. The basic principles of the diet are that all dishes should be steamed or baked. The frequency of meals should be 6 times a day, taking into account that the last meal will be no later than 19.00. All food consumed must be warm. The diet should include foods high in calories; the diet for ulcerative colitis of the intestine should be hypercaloric - up to 3000 calories per day (if the patient does not have a problem with excess weight). It is necessary to consume foods with a high content of proteins, vitamins and microelements. It is recommended to eat a lot of fruits, berries, slimy porridges, boiled eggs, lean meat and fish. It is useful to include beef liver, cheese, and seafood in the diet.
You should exclude from your diet foods that can cause chemical and mechanical irritation of the colon mucosa, as well as foods that activate colon peristalsis. The consumption of carbonated drinks, drinks containing caffeine, also strong tea, cocoa, chocolate, alcohol, fermented milk products, mushrooms, fatty meats (pork, goose, duck) is prohibited. The use of kiwi, dried apricots and plums, and raw vegetables is not recommended.
The list of prohibited foods includes chips, popcorn, crackers, nuts, seeds, any kind of spices, salty and spicy foods, ketchup, mustard, legumes, and corn.
Prevention
The main method of preventing any problems with the gastrointestinal tract is the habit of a healthy lifestyle. Knowing about the hereditary predisposition to ulcerative colitis, it is necessary to eat properly, avoiding foods that irritate the intestines. You should completely give up alcohol and cigarettes, monitor your weight, normalize your work and rest schedule, play sports, and avoid stress and emotional stress.
It is necessary to carefully monitor the condition of the body, do not ignore any gastrointestinal ailments and undergo regular examinations.