More about the disease
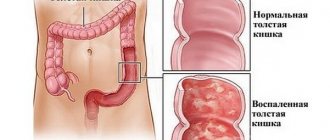
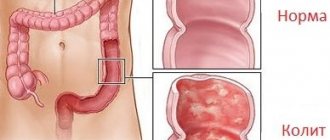
Left-sided colitis is caused by an unusual reaction of the body's immune system, leading to inflammation of the large intestine. This inflammation leads to small ulcers in the lining of the colon. Left-sided colitis is a chronic disease for which there is currently no cure.
In this form of ulcerative colitis, inflammation extends from the rectum to the splenic flexure. Splenic flexure is the name given to the flexure in the colon, next to the spleen. It is located on the left side of the abdomen.
Inflammation of the intestinal mucosa leads to significant disturbances in the functioning of the digestive system. This disease affects men over 40 years of age and women over 20. But not all patients receive timely treatment. Experts believe that manifestations of left-sided colitis occur in more than half of people with problems with the gastrointestinal tract.
Left-sided colitis is accompanied by inflammatory processes of the rectum, which, in turn, spread upward to the splenic flexure of the colon. This leads to proctosigmoiditis and false diarrhea, accompanied by bleeding. These symptoms clearly indicate impaired colon function, treatment of which is a priority. In addition, forms of colitis can flow into others, and left-sided can develop from a peptic ulcer.
Damage to the left side is noted in 60% of patients. Left-sided colitis is diagnosed with inflammation of the descending colon, sigmoid and rectum. Rectosigmoiditis accounts for the bulk of inflammation. It is associated with constipation and increased secretion of mucous secretions from the rectal walls.
It is the irritation of the rectum by mucus that leads to the phenomenon of tenesmus. The patient feels the urge to defecate, but goes to the toilet with the same mucus with small lumps of feces mixed with strands of blood and pus.
Causes of colitis
This or that type of colitis can occur for various reasons. The most common ones are:
- Use of antibiotics in treatment. Some antibiotics interact with natural bacteria in the stomach that are involved in the digestive process. The natural balance of bacteria can be disrupted by antibiotics. Some strains begin to grow rapidly, leading to inflammation of the intestinal mucosa.
- Hereditary factor. Heredity is one of the causes of the disease. According to studies, the parents of many patients suffering from colitis also had this disease.
- Stress. Scientists have not noted a direct connection between stress and the occurrence of colitis. However, emotional overload can become an indirect factor in the onset of the disease.
- Autoimmune causes. According to scientists, the immune system of some people can actually influence the development of the disease. When a person gets sick, the defense mechanisms in his body begin to fight bacteria. However, in some people, the immune system struggles lead to inflammation of the digestive system. As a result, the body fights with itself, destroying its own tissues. Colitis can be one of the consequences of such a struggle.
Classification of colitis
The disease is classified according to several criteria:
- By the nature of the course: Acute. It occurs together with other diseases: gastritis, ulcers, so the symptoms are similar to those of other gastrointestinal inflammations.
- Chronic is a pathology that returns periodically and occurs without pronounced symptoms, but it is dangerous because it slowly destroys the structure of the intestinal wall, so after its treatment a long recovery period will be required.
- By type of disease: Spastic – one of the forms of chronic colitis. It is characterized by such a sign as a violation of intestinal motor activity. As a result of problems with peristalsis, the patient suffers from constipation, pain and cramps.
- Infectious – develops as a result of the activity of pathogenic microorganisms, accompanied by symptoms of viral or bacterial infection, for example, an increase in body temperature.
- Toxic - can appear during poisoning with various foods or chemicals, as well as during long-term treatment with certain pharmaceuticals. If the patient does not pay attention to the symptoms of the disease and continues therapy, or does not review the composition of the daily menu, then the disease will develop into one of the chronic forms, for example, spastic colitis.
- Nutritional – due to unbalanced nutrition.
- Ulcerative – in most cases the result of chronic. Nonspecific ulcerative colitis, characterized by diffuse lesions of the epithelium of the large intestine, is also possible. Methods for its treatment are described here.
- Ischemic is a form of the disease that mainly affects older people. Its occurrence is associated with senile disruption of the blood supply to the gastrointestinal tract.
Symptoms of intestinal colitis: general signs
General symptoms of colitis are present with the manifestation of any type of pathology. Only additional symptoms differ in different forms of the disease. The female body is more sensitive to pain than the male body.
General symptoms:
- pain in the abdominal area (the intensity of this symptom may vary, but it is common and mandatory for all forms and stages of colitis);
- disruption of the bowel movement process (impaired intestinal motility leads to diarrhea or constipation; in some forms of colitis, these conditions alternate);
- bloating (all types of the disease are characterized by rumbling in the abdomen, excessive gas formation and flatulence);
- general weakness of the body (the combination of different manifestations of pathology causes a deterioration in the woman’s general condition, rapid fatigue, a tendency to frequent headaches and insomnia);
- painful or false urge to defecate (pain syndrome occurs in the abdominal area and the urge to defecate, the woman constantly feels incomplete bowel movement, a symptom characteristic not only of constipation, but also of diarrhea);
- the appearance of blood or mucus in the stool (a symptom characteristic of all forms of the disease).
Signs of acute intestinal colitis
An attack of acute colitis always occurs suddenly. Its obligatory sign is a sharp and intense painful spasm. Additional symptoms depend on the individual characteristics of the woman’s body and the level of immunity. If there are no serious problems with the functioning of the digestive tract, then the intensity of the pain will decrease.
Features:
- pain after stress or eating fatty, fried, spicy foods;
- the presence of blood or green streaks in the stool;
- feces are excreted in minimal quantities;
- false urge to defecate and a feeling of incomplete bowel movement;
- increased body temperature, chills, fever.
Chronic intestinal colitis, its symptoms
A distinctive feature of chronic colitis is the presence of remission. Attacks occur several times a year with varying intensity. The severity of the pain syndrome depends not only on the individual characteristics of the woman’s body, but also on the correctness of the chosen treatment tactics.
If the patient follows the doctor’s instructions, the symptoms of chronic colitis will cause minor discomfort.
Distinctive features:
- some time before the attack, general weakness of the body appears;
- pain syndrome develops from the lower abdomen;
- prevalence of constipation;
- regular feeling of thirst;
- pain occurs after a violation of the diet;
- rashes on the skin (as a result of metabolic disorders).
Spastic intestinal colitis, its symptoms
Spastic colitis or irritable bowel syndrome is always accompanied by spasms in the digestive system. The pain may be accompanied by a fever. The woman develops chills, increased sweating, and general weakness of the body. If there are additional pathologies of the digestive tract, the pain intensity will be maximum.
Distinctive features:
- abdominal cramps after eating or a stressful situation;
- mucus impurities in feces (rarely blood);
- pronounced flatulence;
- instability of the bowel movement process.
Signs of ulcerative colitis of the intestine
A distinctive feature of the ulcerative form of colitis is the occurrence of pain not only in the area of the digestive organs, but also in the joints. As a result of metabolic disorders, rashes appear on the skin. A parallel symptom is itching of the mucous membranes. The danger of this form of pathology is the increased risk of blood clots. The inflammatory process can spread to the gallbladder.
Distinctive features:
- fecal incontinence;
- false urge to defecate is replaced by constipation;
- there is mucus and putrefactive inclusions in the stool;
- excessive sweating and chills;
- signs of intoxication of the body;
- defecation is accompanied by pain.
Symptoms of nonspecific ulcerative colitis of the intestine
Nonspecific ulcerative colitis develops in two variants - with severe pain symptoms or in a sluggish form. In most cases, women experience diarrhea, but in the presence of inflammation of the sigmoid colon, the symptom gives way to constipation. According to some signs, this type of colitis may resemble hemorrhoids. An attack is always accompanied by pale skin and general weakness of the body.
Distinctive features:
- bowel movements up to 25 times a day;
- impurities of pus, mucus and blood appear in the stool;
- the attack is accompanied by pallor of the skin;
- tendency to fecal incontinence;
- increase in body temperature.
Enterocolitis, its main symptoms
Enterocolitis in most cases is provoked by the progression of an infectious process in the digestive system. The symptoms of the disease resemble food poisoning. An additional manifestation of enterocolitis can be gastritis. The intensity of pain symptoms depends on the individual characteristics of the female body.
Distinctive features:
- nausea and uncontrollable vomiting;
- intense diarrhea;
- streaks of blood in stool;
- pain in the abdominal area;
- increased body temperature;
- general intoxication of the body.
Symptoms of ischemic colitis
Ischemic colitis occurs against the background of intestinal obstruction. The pain syndrome reaches its maximum levels. The clinical manifestation of the disease depends on the degree of occlusion of the mesenteric artery. The danger of the pathology lies in the risk of painful shock.
This condition is accompanied by loss of consciousness and disturbances in psychomotor reactions.
Distinctive features:
- spasmodic pain appears immediately after eating;
- obligatory symptoms are nausea, vomiting and flatulence;
- with painful shock, blood pressure decreases, pallor of the skin and signs of tachycardia appear.
Causes of colitis
There is no exact cause of left-sided colitis, but there are many hypotheses as to why it occurs. Some researchers believe that ulcerative colitis is an autoimmune disorder that targets the digestive system.
Doctors know that there are many different risk factors for left-sided colitis:
- history of inflammation and antibiotic use;
- a family history of ulcerative colitis or other digestive disorders;
- living in a developed country;
- living further from the equator.
These risk factors are not causes of ulcerative colitis, but do mean that people with these factors are more likely to develop the condition.
Acute left-sided colitis often occurs as a result of intestinal damage: salmonella, viruses, pathogenic fungi. The causes may also be various poisonings and intoxications of the body.
The development of left-sided colitis can be caused by:
- unhealthy diet;
- long-term use of antibiotics;
- chronic constipation;
- previous stomach diseases;
- congenital insufficiency of intestinal function;
Risk factors for colitis:
- decreased immunity;
- lack of plant foods in the diet;
- alcoholism;
- frequent consumption of spicy foods;
- stress.
Symptoms of left-sided colitis
The symptoms of left-sided colitis are very similar to the various types of inflammatory colitis. Chronic diarrhea is the most common symptom of left-sided colitis. Many people also complain of feeling a constant need to go to the toilet. This sensation is called tenesmus and is caused by irritation and inflammation in the rectum.
Other symptoms of ulcerative colitis include:
- weight loss;
- dehydration caused by diarrhea;
- fever;
- stomach ache;
- rectal spasms;
- constipation.
There may be blood in the stool, which is a sign of damage to the colon.
The most common symptoms of left-sided colitis:
- rumbling in the stomach;
- bloating;
- pain on palpation;
- diarrhea;
- lack of appetite;
- general malaise, decreased ability to work.
Types of colitis (by etymology)
Infectious
The colon contains a huge number of bacteria, the presence of which does not cause discomfort or any symptoms. However, if pathogenic bacteria enter the human body, the large and small intestines become infected. This is how food poisoning occurs. The most common pathogenic bacteria include: Campylobacter, Shigella, Salmonella and E. coli. These bacteria often lead to dehydration and cause diarrhea accompanied by bleeding. Intestinal infection can also occur when parasites, such as Giardia, living in contaminated water, enter the body.
One type of the disease is called pseudomembranous colitis. The disease can occur in patients who have recently taken antibiotics for a long time that alter the normal intestinal flora. Violation of the flora leads to the active growth of clostridium bacteria, which produce toxins that lead to diarrhea.
Infectious colitis may be accompanied by fever.
Radiation
Occurs in a person suffering from radiation sickness.
Ischemic
Atherosclerosis leads to narrowing of the arteries that supply blood to the colon. When blood flow becomes insufficient or restricted, the blood vessels become inflamed. This leads to colitis. To get rid of the disease, you need to establish the cause of the circulatory disorder. The cause may be hernias, intestinal volvulus, infections, diabetes mellitus or excess fat deposits. In addition, ischemic colitis occurs as a result of anemia, mechanical injury, dehydration and a drop in blood pressure. Symptoms of this type of disease include bloody stools, severe pain in the colon, and fever.
Chemical
The disease occurs as a result of the accumulation of chemicals in the colon. Chemical colitis can be caused by antibiotics. That is why taking this group of drugs should be carried out under the strict supervision of a doctor.
Microscopic
The disease mainly occurs in older women. A symptom of microscopic colitis is non-bloody, watery stool. This type of disease consists of:
- lymphocytic colitis;
- collagen colitis.
Inflammatory bowel diseases
There are 2 types of inflammatory bowel diseases:
- Crohn's disease. Can affect any part of the digestive tract. In this case, the affected areas alternate with healthy ones;
- Ulcerative colitis. Refers to autoimmune diseases. This means that the patient’s immune system “attacks” the large intestine, which leads to inflammation. The disease begins in the rectum and then can spread further.
Features of colitis in children
In acute colitis, the course of the disease and treatment measures in children are the same as in adults. Chronic colitis in children, as a rule, is the outcome of acute intestinal infections, most often dysentery. Less common causes of chronic colitis are amoebiasis, giardiasis balantidiasis, helminthic infestations, and mushroom poisoning. Dysbacteriosis and disorders of the nervous and humoral regulation of the intestine are of great importance in the development of the disease.
Causes
A certain role is assigned to the reduction of local immunity of the colon mucosa and autoimmune processes. The main causes of colitis in children are irrational use of antibiotics, unbalanced nutrition (predominance of carbohydrates in food, deficiency of proteins and vitamins), food allergies in children, physical and neuropsychic stress, and diseases of other organs.
When the disease lasts up to 2-3 years, as a rule, segmental colitis is observed, affecting mainly the distal parts of the colon, which is facilitated by such anomalies of its development as dolichosigma, megacolon. With a longer process, pancolitis develops.
Symptoms
Symptoms depend both on the phase of the disease and the location of the pathological process. During exacerbation, abdominal pain is noted, often paroxysmal, localized around the navel or along the colon in the right (with typhlitis) or left (with sigmoiditis) iliac region. The pain intensifies before defecation, with flatulence, physical activity, and excessive consumption of fresh fruits, vegetables, and milk.
The equivalent of pain in young children is the symptom of “slipping” (loose stool after eating), caused by an increase in the gastroileocecal reflex. Rumbling in the intestines, flatulence, and increased release of gases are noted. Characterized by constipation, which can be replaced by diarrhea. The stool becomes more frequent and becomes pasty or liquid.
Nausea, belching, and less commonly heartburn and vomiting are observed, in most cases due to involvement of the upper digestive tract in the process. On palpation, the large intestine is painful, spasmodic in places. In the stage of incomplete clinical remission, children have no complaints, but pain on palpation and stool disorders persist. In the stage of clinical remission, children feel healthy, but examination reveals changes in the colon.
Colitis caused by clostridia, which usually develops after taking broad-spectrum antibiotics (pseudomembranous colitis), is somewhat unique. Characterized by sudden, paroxysmal abdominal pain without clear localization, diarrhea or constipation. The feces are fragmented, shrouded in mucus, and contain almost no remains of undigested food. The course of the disease is undulating. exacerbations are usually associated with ingestion of food containing allergens.
Treatment of colitis in children
In case of exacerbation of chronic colitis, hospitalization is indicated. Bed rest is prescribed until spontaneous pain disappears. Diet No. 4 is used, for diseases of allergic origin - diet T (hypoallergic) with the exclusion of dairy products, eggs, and limitation of flour products; with concomitant damage to the small intestine and the development of malabsorption syndrome, a gluten-free diet that excludes flour products, semolina and oatmeal porridges, sausages, sausages, strong meat broths and sauces can be effective.
The ratio of fats and carbohydrates in the diet of children with chronic colitis approaches the physiological norm; the amount of proteins can be increased by 10-15%. Fats included in the recommended diet should contain fatty acids with a medium-length carbon chain (lean meats, fish, vegetable oil, eggs). When prescribing drug treatment for colitis in children, drugs used in adults are mainly used, but antibiotics and sulfonamides are rarely used.
The most effective in childhood are bacterial preparations that normalize intestinal microflora (colibacterin, bifidumbacterin, bificol), and specific bacteriophages.
Children are often given local treatment (microenemas with sea buckthorn, rose hip, eucalyptus oil, Shostakovsky balm, etc.). Physiotherapeutic treatment is widely used (in case of exacerbation - warming compresses, warm heating pads on the stomach, electrophoresis of novocaine, calcium chloride, during remission - mud therapy, diathermy, ozokerite paraffin), abdominal massage, exercise therapy. Sanatorium-resort treatment is carried out no earlier than after 3-6 months. after discharge from the hospital.
Diagnosis of left-sided colitis
Correct diagnosis of left-sided colitis is the most important step in treatment. Doctors order an endoscopy to get an image of the colon, which will help doctors look for signs of inflammation, such as redness, swelling and other visual changes.
Diagnosis of intestinal inflammation consists of determining the stage of the process, localization of the disease and the degree of damage to the mucosa. It is necessary to distinguish the symptoms of colitis from signs of Crohn's disease, gynecological, urological, and cardiac diseases.
The following will help to establish an accurate diagnosis:
- external examination, palpation;
- general blood test, urine test, as well as blood biochemistry, stool examination for dysbacteriosis, worm eggs, calprotectin;
- plain radiography;
- radiography with barium sulfate;
- intestinal endoscopy with collection of material for histology;
- Ultrasound, MRI, .
Differential diagnosis
This is only possible using instrumental examination methods. Used:
- sigmoidoscopy – examination of the rectum;
- endoscopy – examination of the entire large intestine using an endoscopic device with a video camera and the ability to broadcast the image to a monitor;
- irrigoscopy - x-ray examination of the intestine after preliminary administration of a contrast mixture, most often barium sulfate;
- angiography or visualization of intestinal vessels if ischemia is suspected;
- fecal analysis for helminth eggs;
- bacterial culture of stool, during which infectious agents are detected and their sensitivity to antibiotics is determined;
- examination of other parts of the digestive canal if inflammation is suspected of spreading from there.
Be sure to read:
Duodenitis (inflammation of the duodenum): symptoms and treatment methods
Studies make it possible to determine the condition of the mucous membrane - simple thickening due to chronic inflammation or the presence of ulcers of different sizes. With a long course of the disease, studies are prescribed to determine metabolic disorders: blood tests for various ingredients, determination of the concentration of minerals and vitamins, hormones.
Treatment
Treatment of colitis is aimed at eliminating the causes that lead to the pathology. The course of treatment includes:
- for acute colitis, antibiotics are prescribed (selected individually for each patient);
- preparations for removing toxins (activated carbon, white carbon, etc.);
- antispasmodics - for severe pain (no-spa, revalgin);
- for diarrhea - loperamide, oak bark infusion, etc.;
- for constipation, laxative;
- probiotics - for dysbacteriosis (Linex or the Russian analogue of Linex, only cheaper, normobact);
- physiotherapy (electrophoresis, acupuncture);
Treatment for left-sided colitis will depend on several factors: the severity of symptoms and how the person responds to medications.
Medicines are currently the first line of treatment for colitis. Depending on the diagnosis and severity of symptoms, doctors prescribe one or more medications to treat left-sided colitis.
One of the most common and effective drugs is 5-aminosalicylic acid (5-ASA). It can be taken orally, with an enema, or topically. 5-ASA reduces colon inflammation. Recent studies have noted that topical 5-ASA may be more effective than other methods. These treatments induce remission in 72% of cases. The researchers also noted that a combination of oral and topical treatments helped reduce symptoms.
While 5-ASA helps in most cases, some people do not respond to this drug. In these cases, doctors prescribe corticosteroids to control the inflammation. Corticosteroids are often used together with 5-ASA for better effect.
In cases where both 5-ASA and corticosteroids do not help, doctors may recommend immunosuppressants. These drugs target immune system proteins that cause inflammation in inflammatory colitis.
Severe cases of colitis may require hospitalization. At the clinic, the person receives intravenous medications and steroids to reduce symptoms. In rare cases, doctors may recommend removing part of the colon. This is usually associated with severe damage, inflammation or bleeding in the affected area.
Antibacterial agents for colitis
Colitis of an infectious nature is treated with antibacterial medications. The doctor treats intestinal inflammation with drugs:
- group of nitrofurans – Enterofuril, Furazolidone;
- group of sulfonamides – Phthalazol;
- rifampicin group – Alpha Normix;
- group of fluoroquinolones – Tsifran;
- group of polymyxins – Polymyxin-v sulfate, Polymyxin-m sulfate;
- broad spectrum antibiotics - Tetracycline, Levomycetin, Oletetrin, Streptomycin, Neomycin, Monomycin.
Before using antibiotics, an analysis of the sensitivity of the flora to drugs is carried out to prescribe the most effective remedy. Take in the dosage indicated by the prescription, strictly observing the time intervals.
Anthelmintics for colitis
If colitis is caused by parasitic worms, anthelmintic drugs are prescribed. Methods and means of treatment depend on the type of parasite.
The following can cure helminthiasis in colitis:
- Nemozol;
- Vermox;
- Albendazole;
- Dekaris;
- Praziquantel;
- Pirantel.
Tablets and suspensions for worms are highly toxic. Treat helminthiasis carefully, following the dosage and doctor's instructions.
Antispasmodics for colitis
Antispasmodic drugs are intended to treat colitis with painful spastic pain. They will relieve pain by relaxing tight muscles.
Spasms are treated with medications:
- No-Shpa;
- Spasmol;
- Duspatalin;
- Dicetel;
- Buscopan;
- Papaverine;
- Papazol.
In addition to pharmaceutical drugs, folk methods will help relieve pain from illness. Decoctions of mint, chamomile, oregano, and calamus will relieve pain, relieve spasms, and soothe irritated mucous membranes. Brew a teaspoon of dry herb with 200 ml of boiling water, leave for 30 minutes. Take 50 ml between meals 4 times a day. The course of treatment is from 2 weeks to a month.
Diarrhea remedies
Diarrhea threatens with dehydration and impaired water-electrolyte metabolism. You can stop diarrhea with Smecta, Enterosgel, Imodium. To replenish moisture, drink more water, weak tea, compote, or rosehip decoction.
Herbal decoctions will be effective for colitis with diarrhea:
- infructescences of gray alder, rhizomes of snake knotweed;
- oak bark, cinquefoil rhizome.
Take a teaspoon of dry ingredients mixed in equal parts, pour in 300 ml of boiling water and simmer for 15 minutes in a water bath. Cool, filter, take 2 tablespoons 20 minutes before meals.
Remedies for bloating and gas formation
Excess intestinal gases cause great inconvenience to those suffering from colitis. The solution to the problem is simple - you need to prepare a decoction according to the recipe:
- chamomile flowers, oregano herb, caraway fruits;
- calendula flowers, chamomile flowers, peppermint leaves, valerian root.
Brew a teaspoon of the mixture in equal parts of dry plants with 300 ml of boiling water, leave for 30 minutes. Take 100 ml of decoction an hour after meals three times a day.
Surgical intervention
Indications for surgical treatment are the ineffectiveness of diet and conservative therapy, the development of complications (massive bleeding, perforation of the colon, if a malignant neoplasm is suspected, etc.).
Resection of the large intestine followed by the creation of an ileorectal anastomosis (connection of the free end of the ileum to the anal canal) is the most common surgical technique for treating ulcerative colitis. In some cases, a section of the affected intestine limited within healthy tissues is removed (segmental resection).
Complications of left-sided colitis
Left-sided colitis can cause complications, including toxic megacolon and anemia.
Toxic megacolon is a common complication of inflammatory bowel disease and causes dilatation of the large intestine. Symptoms include abdominal pain, fever, dehydration and malnutrition. Toxic megacolon can cause damage to the colon. The condition is usually treated with medications, intravenous fluids, and sometimes surgery.
Anemia can be another complication of left-sided colitis. Loss of blood from an inflamed intestine can lead to anemia. Treatment uses iron supplements or blood transfusions.
Additional methods of treating the disease
Many people use diet and lifestyle changes to reduce the symptoms of left-sided colitis. More research is needed to find natural methods that are effective for ulcerative colitis symptoms. For example, probiotics may reduce the symptoms of colitis but should not be considered a stand-alone treatment. There is also evidence that people with colitis may benefit from acupuncture.
Other natural supplements and foods that may help with ulcerative colitis:
- Omega-3 fatty acids;
- probiotics;
- turmeric;
- folates and foods rich in folic acid.
Nutrition for pathology
The diet is based on the specifics of the disease: exacerbation or remission of the disease, whether constipation or diarrhea predominates, whether there is a food allergy.
For diarrhea during an exacerbation, a chemically and mechanically gentle diet No. 4b is prescribed. The diet includes: quince, pear, strong tea, pureed porridge, slimy soups, blueberries, bird cherry - i.e. foods that reduce intestinal motility. Fruits and vegetables are consumed boiled and pureed.
Excluded from the diet: milk - for flatulence, radishes, cabbage (coarse plant fiber), legumes, rye bread (gas-forming products).
If left-sided colitis is accompanied by constipation, diet No. 15 is prescribed, and the diet in this case is based on products containing coarse plant fiber and promoting more complete bowel emptying (brown bread, raw vegetables, fruits). Also, the diet should be based on a large amount of B vitamins.
The final stage of digestion occurs in the large intestine. The absorption of water, the formation of feces, and the production of vitamins B, PP, E, and K occur primarily in the long colon. Colitis, or inflammation of the large intestine, manifests itself with specific symptoms and can be treated in adults and children. Intestinal colitis disrupts the natural processes of digestion, worsens well-being, and limits life opportunities.
A diet high in fiber and low in refined carbohydrates can relieve inflammation in the colon.
During the period of exacerbation or acute course of colitis, the menu consists of boiled or steamed dishes. Food should not have coarse particles that can irritate the intestinal mucosa, so soups and cereals are blended with a blender or rubbed through a sieve.
List of prohibited foods for colitis:
- rye and fresh bread;
- baked goods;
- pasta;
- rich broths;
- fatty meats, fish and poultry;
- milk;
- caviar;
- eggs, hard-boiled or fried;
- pearl barley porridge and soup;
- legumes;
- raw fruits;
- honey;
- sweets;
- fruit juices, which increase gas formation in the intestines;
- alcohol;
- carbonated drinks.
During the period of remission, nutrition should be balanced and healthy. You need to eat in small portions (5-6 times a day), and it is also important to drink enough liquid.
It is recommended to exclude from the diet spicy and fatty foods, whole milk, as well as foods that contain coarse plant fiber and promote gas formation - white cabbage, legumes, black and whole grain bread, grapes and others. Drinking alcoholic beverages is strictly prohibited.
When preparing food, preference should be given to baking, boiling or steaming dishes.
For colitis, which is accompanied by constipation, the menu must include beets, carrots, dried fruits, apricots, kiwis, and consuming 1 tablespoon of any vegetable oil in the morning on an empty stomach will also help loosen stools.
Traditional methods of treatment
Treatment of colitis with folk remedies depends on the type of disease. It is impossible to completely cure the disease in adults with herbs, especially the acute type. Before starting treatment with folk remedies, you should definitely consult your doctor. He will tell you whether it makes sense to carry out such therapy in a specific clinical case.
This disease is treated in adults using herbal remedies. Valerian root, fennel seeds, chamomile flowers, mint leaves in a ratio of 1:1:6:2. Sage, mint, St. John's wort, caraway fruits, chamomile - all 1:1. Oregano, shepherd's purse, knotweed, motherwort, St. John's wort, yarrow, nettle in equal proportions. These fees have an anti-inflammatory effect and are used in the treatment of chronic types of illness in adults.
Dial 2 tbsp. l. collection pour 1 liter. boiling water and leave for 10-12 hours. You need to drink a third of a glass 4 times a day. The course of treatment is 3 months with a break of two weeks. After the break, apply the next charge. Soda is often used in folk medicine. Treatment with soda will help restore the natural intestinal microflora. for this 0.5 tsp. dissolve soda in 0.5 tbsp. warm water and drink in the morning.
Antimicrobials
Medicines in this group are prescribed for the treatment of functional intestinal dyspepsia.
- Phthalazole
Available in tablet and powder form.
The main component in the composition is phthalylsulfothaisol, auxiliary components are calcium stearate and potato starch.
The peculiarity of the drug is that it is practically not absorbed into the blood, but acts directly in the organs of the digestive system. Phthalazole has a pronounced antimicrobial and anti-inflammatory effect, and also restores the functionality of the intestines, relieving inflammation.
This medicine is approved for the treatment of adults and children over 2 years of age:
- The children's daily dosage is 0.2 g per 1 kg of weight. This amount is divided into 3 parts and taken every 8 hours;
- adult patients can take 1-2 g of Phthalazole every 4-6 hours.
Contraindications for use: diseases of the thyroid gland, liver and circulatory system.
- Sulfasalazine
Available in the form of round tablets, light brown in color.
The main active ingredient, sulfasalazine, has a pronounced anti-inflammatory effect, therefore it is often prescribed both for exacerbation of the chronic form of the disease and for colitis in remission.
The dosage of Sulfasalazine depends on the age of the patient:
- for children 5-7 years old – 0.5-1 tablet 3-6 times a day;
- after 7 years – 1 tablet with the same frequency;
- adults can take 1 tablet 4 times a day on the first day of therapy, on the second - 2 tablets, on the 3rd day and beyond - 3-4 tablets 4 times a day.
Contraindications: diseases of the circulatory system, pathologies of the liver and kidneys and individual intolerance to the ingredients of the drug.
Before using these medications, you should consult your doctor.
Prevention
To avoid complications and serious health problems, timely treatment is necessary, as well as preventive measures:
- maintaining a healthy lifestyle;
- use of personal household items;
- strict compliance with prescribed nutrition, adherence to diet;
- timely consumption of food (breakfast cannot be ignored);
- compliance with basic hygiene rules (washing hands);
- avoiding the intake of raw water and thoroughly washing vegetables and fruits before consumption;
- visits to doctors, regular medical examinations by a dentist, family doctor, gastroenterologist.
Disease prognosis
With a mild course without complications, the prognosis is favorable. About 80% of patients taking 5-acetylsalicylates as maintenance therapy do not report relapses or complications of the disease throughout the year. Patients usually experience relapses once every five years; in 4% there are no exacerbations for 15 years. Surgical treatment is resorted to in 20% of cases. The probability of developing a malignant tumor in patients with ulcerative colitis ranges from 3-10% of cases.
Sources: https://www.kolit.su/vidy/levostoronnij-kolit-kishechnika medicalinsider.ru/news/chto-takoe-levostoronnijj-kolit/ https://kcson-sp.ru/levostoronniy-kolit-kishechnika-simptomy -i-lechenie-u-vzroslyh.html zhkt.guru/kolit-2/vidy-4/levostoronniy https://bolvkishkah.com/kolit/levostoronnij-kolit.html https://ru.oldmedic.com/what- is-left-sided-ulcerative-colitis-6350 https://lechenie.gastrit-i-yazva.ru/yazva/hronicheskij-levostoronnij-kolit-kishechnika This material is exclusively subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/19/2020