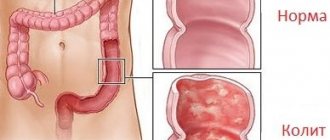
Chronic colitis is an inflammatory process affecting the large intestine. It occurs over a long period of time and in waves, causing intestinal dysfunction. The result of the process is inflammatory and dystrophic changes in the mucous membrane.
According to statistics, chronic colitis is observed in at least 50% of patients with diseases of the gastrointestinal tract. The disease is most common in North America and Europe, and the term “chronic colitis” is not used there.
Most often, men over 40 and women aged 20 to 60 consult a doctor with chronic colitis.
Types of chronic colitis
There are several classifications of chronic colitis.
By location:
- proctitis - an inflammatory process in the rectum;
- transversitis - damage to the transverse colon;
- typhlitis - the inflammatory process affects the appendix and cecum;
- sigmoiditis – the sigmoid colon is affected;
- pancolitis – a total inflammatory process develops.
Due to development:
- infectious;
- parasitic;
- nutritional;
- ischemic;
- medicinal;
- allergic;
- mechanical;
- radiation;
- intoxication;
- mixed;
- cryptogenic.
Depending on the violation of the structure of the intestinal mucosa:
- atrophic;
- ulcerative;
- catarrhal;
- erosive;
- mixed.
Depending on the presence of motor dysfunction:
- with dyspepsia;
- with motor dysfunction.
Symptoms
Since the chronic course of the disease involves alternating periods of exacerbation and resolution of symptoms, patients most often seek help from a doctor precisely at the moments of acute manifestation of symptoms. During remission, they are expressed to a weak degree or are completely absent. Thus, the symptoms of chronic colitis are:
- soreness, the localization of which spreads along the lateral parts of the abdomen. The pain can range from severe cramping to aching, and, as a rule, does not spread to other internal organs;
- diarrhea followed by constipation, or vice versa;
- rumbling in the intestines - can cause discomfort because it is constant;
- frequent belching, often with an unpleasant odor;
- change in the size of the abdomen;
- a large amount of emitted gases;
- lack of feeling of complete bowel movement, which often leads to discomfort, and this, in turn, causes frequent mood swings and irritability of the patient;
- false urge to pass feces. Emptying occurs every few days;
- constant nausea and malaise;
- the appearance of an unpleasant taste in the mouth;
- weakness of the body;
- severe fatigue occurs even when performing low-intensity physical activity;
- sleep disorders, manifested in the form of insomnia or a change in rest mode, when a person sleeps or is drowsy during the day and is awake at night;
- pale skin;
- increased hair loss and brittle nails;
- change in taste preferences.
Signs of nonspecific ulcerative colitis:
- the appearance of blood or purulent fluid in the stool;
- diarrhea prevails over constipation;
- pain in the lower abdomen is often mild and may resemble tingling or colic. In cases where spasms intensify, this may indicate damage to the deep intestinal tissues;
- bloating in the lower abdomen;
- increased body temperature;
- decreased or complete absence of appetite, which leads to weight loss;
- Inflammation of the vascular, mucous and iris membranes of the eyes appears. But such a sign is detected extremely rarely;
- muscle weakness;
- joint pain.
During an exacerbation of symptoms in ulcerative colitis, changes in the intestinal mucosa may occur. Among them:
- swelling;
- bleeding, which can be noticed by blood in the stool or a change in its color (in this case it will turn black);
- formation of small ulcers;
- the appearance of neoplasms similar to polyps. They appear only during inflammation.
Symptoms of chronic spastic colitis:
- the occurrence of painful spasms that intensify at night or during a long period of refusal to eat;
- bloating;
- increased gas formation;
- alternating constipation and diarrhea;
- insomnia, as a result of which a person is constantly tired;
- headache attacks of varying intensity;
- Complete bowel movement can be accomplished the second or third time. The process of excreting feces occurs once every few days;
- constant rumbling in the stomach.
In order to reduce symptoms, it is necessary to constantly adhere to the diet, but it is important to watch out for the fact that certain foods can cause constipation.
Causes of chronic colitis
Most often, the disease occurs as a result of damage to the colon mucosa by the following pathogenic microorganisms:
- bacteria – shigella, salmonella, yersinia, clostridium, campylobacter, staphylococcus, proteus;
- protozoa - lamblia, amoeba, balantidia;
- viruses – rotaviruses, enteroviruses, adenoviruses;
- mushrooms;
- helminths.
Other causes of chronic colitis include:
- activation of opportunistic microorganisms. Microorganisms can live on the intestinal mucosa, which, when the immune system is disrupted, begin to actively multiply, causing unpleasant symptoms;
- chronic diseases of the genitourinary system (renal failure);
- diseases of the digestive system (pancreatitis, gastritis, hemorrhoids);
- intestinal abnormalities;
- long-term exposure to ionizing radiation on the body;
- gross violations of the diet, consumption of large amounts of dyes, preservatives, hot seasonings and spices;
- endocrine diseases (diabetes mellitus, Addison's disease, thyroiditis);
- poisoning with alcohol-containing drinks, salts of heavy metals, alkalis, pesticides;
- long-term food allergies;
- use of medications that can negatively affect the mucous membrane of the colon (non-steroidal anti-inflammatory drugs, salicylates, laxatives).
In most cases, chronic colitis occurs due to a combination of different factors that enhance each other’s effects. Often the cause of colitis is infection in combination with poor diet and self-medication.
The prognosis is favorable in case of correct and timely treatment. If the patient follows all the doctor’s recommendations and eats properly, long periods of remission are possible.
Sometimes it is not possible to find out the root cause of the disease. In this case, cryptogenic colitis is diagnosed.
Factors that influence the development of the disease include:
- poor nutrition;
- obesity;
- severe chronic diseases;
- disruption of the innervation of the intestinal wall;
- immunodeficiency states;
- industrial or household contact with toxic substances;
- alcoholism;
- a history of acute infectious diseases of the digestive system;
- adhesions and polyps in the intestines, making it difficult to move contents through the colon;
- decreased blood supply as a result of weakened arterial blood flow (ischemia of the intestinal mucosa);
- uncontrolled use of herbal or chemical laxatives;
- abuse of enemas.
Reasons for appearance
Chronic colitis occurs as a result of numerous provoking factors, among which the following reasons can be identified:
- violation of secretory function;
- dysbacteriosis;
- concomitant diseases of the digestive system;
- obesity;
- enzyme deficiency;
- long-term intoxication, food poisoning;
- impaired intestinal motility;
- infectious-inflammatory process;
- prolonged constipation.
Chronic colitis can also be caused by injury or damage to the intestinal mucosa. Violation of tissue integrity occurs during medical research, surgery or after an enema.
In women, pathological processes develop against the background of long-term and strict diets, as a result of poor nutrition. In children, the disease occurs due to a food allergic reaction.
Symptoms of chronic colitis
The disease can be indicated by both local and general symptoms of chronic colitis. They depend on the stage of the disease. During the period of remission, signs of the disease are absent or become so unexpressed that the patient does not pay attention to them. With exacerbation of colitis, they intensify.
Stool disorders
With right-sided colitis and involvement of the lower small intestine, diarrhea is usually observed. The frequency of urges depends on the severity of the disease and can range from 4 to 15 times a day.
With left-sided colitis, when spasm of the distal colon, sigmoid or rectum occurs, the patient may experience constipation. Due to stagnation of feces, small amounts of feces with blood may be released several times a day.
The urge to evacuate (including false ones) may occur after a change in body position, in the morning, during stress or after eating.
Stool with chronic colitis has an unpleasant sour odor. It may contain large amounts of carbon dioxide, mucus and pus. With concomitant pancreatitis, undigested pieces of food enter the stool.
In some cases, patients with chronic colitis experience intestinal crises. They are characterized by the presence of several series of urges to defecate. At the beginning of the process, feces of normal consistency are released, and later they become liquid, mixed with mucus.
The process of their release is accompanied by severe cramping pain in the abdomen, which subsides after the stool leaves the intestines.
Pain
Patients with chronic colitis experience aching pain in the abdomen, sometimes giving way to sharp, cramping pain. The pain syndrome intensifies after eating fried, fatty and spicy foods, fermented milk products, carbonated drinks or alcohol. After defecation or passing gas, the pain decreases.
Painful sensations can be observed before defecation, in some cases they continue for two hours after it.
Other local symptoms of chronic colitis include:
- nausea with periodic recurring episodes of vomiting;
- flatulence;
- feeling of incomplete bowel movement;
- unpleasant taste in the mouth;
- frequent belching;
- weight loss;
- mucus in stool.
Chronic colitis is also accompanied by general symptoms, which include:
- rapid fatigue even with minor physical exertion;
- sleep disorders (a person may experience drowsiness during the daytime and suffer from insomnia at night);
- decreased performance;
- general deterioration of health;
- irritability and apathy.
Acute intestinal colitis, symptoms
A disease called intestinal colitis is accompanied by a number of symptoms. The pain is cutting in nature and often intensifies with movement. Acute colitis develops after infection or after intoxication of the body.
The following symptoms of proctological disease are distinguished:
- pain syndrome:
Throughout the day, the patient experiences severe pain in the stomach. Unpleasant sensations intensify with any physical activity and even with coughing or sneezing.
- temperature increase;
An inflammatory process develops in the body during colitis, as a result of which in most cases the patient’s temperature rises to 39°C.
- gastrointestinal disorders;
A common disease is bowel movement disorder. The patient suffers from frequent urge to go to the toilet. Diarrhea is accompanied by an increase in blood pressure, the mucous membrane is irritated. With constipation, anal fissures form in the anus.
The patient feels cramping pain in the intestines and the abdomen is bloated. Feces stagnate in the body and fecal stones form. Feces increase in size and lead to intoxication of the body. Frequent urge to go to the toilet sometimes does not lead to bowel movement, during which the walls of the anus are injured.
- impurities in feces;
Impurities of blood, mucus and even pus are found in the stool. The blood is dark brown in color. This symptom indicates an inflammatory process.
- flatulence and heaviness in the abdomen;
After eating, the patient is bothered by flatulence and bloating. Gas formation brings discomfort and disrupts the usual way of life. My stomach is constantly growling. Regardless of food intake, severe discomfort is felt in the stomach area.
- lack of appetite;
Due to problems associated with digestion, the patient has no appetite throughout the day.
- nausea and vomiting;
Nausea is observed after eating. Sometimes vomiting begins, in which impurities of mucus and blood appear.
- cardiac system disorders;
All body systems are interconnected, so in some cases there is an increase in blood pressure, dizziness, and tachycardia.
Signs of intestinal colitis in women are similar to pathological processes in the urinary and reproductive systems. Patients often confuse colitis with problems of the uterus and appendages. If abdominal pain intensifies during sexual intercourse, or vaginal discharge appears, then we are talking about gynecological problems.
In acute intestinal colitis, the symptoms vary in nature and intensity. In the early stages, pain appears extremely rarely and does not cause discomfort to the patient. In advanced stages, the pain does not stop throughout the day and does not disappear even after taking painkillers.
If any signs appear, you should contact a medical specialist, namely a proctologist. The private proctology clinic “Proctologist 81” employs highly qualified specialists and doctors of the highest category. For each patient they select an individual treatment method. Diagnosis of the body is carried out using modern technologies and the latest equipment.
Diagnostics
A gastroenterologist diagnoses the disease; initially, he performs palpation, identifying pain along the colon.
In most cases, chronic colitis occurs due to a combination of different factors that enhance each other’s effects. Often the cause of colitis is infection in combination with poor diet and self-medication.
Laboratory research methods include:
- General blood analysis. In this case, an increased number of leukocytes and an acceleration of ESR can be detected (in the stage of exacerbation of chronic colitis).
- Stool examinations. It may contain leukocytes, red blood cells, pus, blood, mucus, ammonia, and parasite eggs.
Instrumental research methods for chronic colitis:
- Irrigoscopy. This is an x-ray examination that is performed with the colon filled with oxygen and barium sulfate. Allows you to evaluate the relief of the mucous membrane and shape.
- Sigmoidoscopy. Using a special device (sigmoidoscope), a visual examination of the mucous membrane of the rectum and distal parts of the sigmoid is carried out. Allows you to detect ulcers, erosions, redness of the mucous membrane, pus, mucus deposits, swelling.
- Ultrasound examination of the abdominal organs. Helps clarify the presence of thickening of the intestinal walls, identify neoplasms and evaluate the effectiveness of therapy.
Differential diagnosis of chronic colitis is carried out with the following pathologies:
- dyskinesia of the large intestine;
- enteritis;
- pancreatitis;
- neoplasms in the intestines.
Treatment of chronic colitis
To treat the disease, medications that belong to the following pharmacological groups are used:
- Antimicrobial agents. They are used in the acute period of a disease caused by pathogenic bacteria.
- Sorbents. Used to relieve intoxication and diarrhea.
- Drugs that inhibit intestinal motility. They are used if chronic colitis is accompanied by diarrhea.
- Laxatives. Used for constipation. Preference is given to drugs that increase the volume of feces and soften them.
- Carminatives. Indicated for flatulence.
- Enzyme preparations. Improves the digestion process.
- Prokinetics. Normalizes contraction of the muscles of the esophagus and stomach.
- Antispasmodics. Reduce pain.
Treatment of chronic colitis should be comprehensive. During the period of exacerbation of the disease, the patient is prescribed bed rest. This makes it possible to reduce energy costs and reduce the amount of food consumed, which allows you to relieve the intestines. In severe forms of the disease, fasting for 24 hours is prescribed. During this period, you can only drink water (1.5–2 liters per day) or tea without sugar in small portions.
Diet for chronic colitis plays an important role. It is determined depending on the predominance of putrefactive or fermentative dyspepsia. Preference should be given to dishes that do not cause intestinal irritation and increase intestinal peristalsis. These include:
- rice or oatmeal cooked in water;
- broth from lean meats (veal, turkey);
- steam cutlets or meatballs;
- vegetable broth soups;
- cottage cheese with minimal fat content;
- boiled fish or meat;
- jelly;
- crackers;
- vegetable purees;
- baked apples.
When exacerbating chronic colitis, exclude from the patient’s diet:
- fatty meats and fish;
- legumes;
- whole milk;
- raw vegetables and fruits;
- carbonated drinks;
- alcohol.
During remission of chronic colitis, you also need to monitor your diet - do not overeat, exclude spicy and fatty foods, smoked meats and pickles from your diet.
In some cases, patients with chronic colitis experience intestinal crises. They are characterized by the presence of several series of urges to defecate.
If you have dyskinetic constipation, it is recommended to eat foods rich in fiber, fresh fruits and vegetables, and prunes. It is effective to carry out fasting days. Depending on the functional state of the intestines, you can drink mineral water.
Preventive measures
In order to prevent the development of chronic colitis, the following recommendations must be followed:
- Eat properly.
- Treat infectious diseases in a timely manner (before they become chronic).
- Stop smoking and drinking alcohol.
- Do not abuse medications.
- Use protective equipment when in contact with toxic substances.
If symptoms of the disease are detected, you should consult a gastroenterologist.
Video from YouTube on the topic of the article: