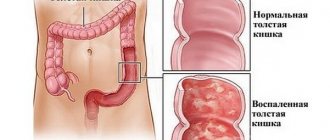
Ischemic colitis is an inflammatory process in the large intestine that occurs during a transient disruption of the blood supply to its wall. Usually develops after the age of 60 years. The diagnosis is confirmed by computed tomography, irrigoscopy and colonoscopy. It is treated predominantly conservatively. Surgical intervention is indicated for significant spread of the process and necrosis of a large area of the intestinal wall.
Symptoms
Variants of the course of the disease:
- Acute colitis. It appears suddenly against the background of complete well-being. Accompanied by vivid clinical symptoms and rapid deterioration of the condition.
- Chronic colitis. Symptoms are moderate or erased. The patient's condition worsens gradually.
Gastrointestinal symptoms
Local symptoms come to the fore in chronic colitis:
- Pain in the umbilical region, right or left in the iliac region. Pain syndrome occurs 1-1.5 hours after eating or physical activity and disappears spontaneously after 2-3 hours.
- Unstable stool: constipation alternates with diarrhea. Loose stools with a lot of mucus and streaks of blood predominate.
- False urge to have a bowel movement.
- Bloating and flatulence.
- Recurrent bleeding from the anus.
The intensity of symptoms depends on the extent of the process. If the pathological focus is limited to a small segment of the intestine, the manifestations of the disease will be weak and erased. With significant circulatory impairment, signs of colitis increase.
Manifestations of the disease depend on the stage of its development:
- With a reversible disruption of blood flow in the intestines, pain occurs periodically and almost always subside on its own. Blood in the stool and bleeding occur a few days after the onset of the disease. Reversible ischemic colitis is possible with a short-term disruption of blood flow or against the background of the development of collaterals (bypass blood vessels).
- With irreversible disruption of the blood supply, symptoms progressively increase. The pain intensifies, the stool becomes liquid with an admixture of blood. The general condition worsens, signs of intoxication of the body appear. This option is possible with significant disruption of blood flow, intestinal necrosis and the absence of collaterals.
Extraintestinal (general) symptoms
A change in general condition is characteristic of acute colitis with irreversible disruption of blood flow. The following symptoms occur:
- increased body temperature;
- chills;
- nausea;
- vomiting that does not bring relief;
- confusion.
Signs of general intoxication increase along with an increase in the area of necrosis (death of tissue) of the intestine.
With chronic ischemic colitis, other symptoms may appear:
- general weakness, weakness;
- decreased performance, memory impairment;
- anemia – a decrease in hemoglobin and red blood cells in the blood, leading to oxygen starvation of tissues;
- signs of a lack of certain vitamins when their absorption is impaired (dry skin, brittle nails and hair, muscle weakness, muscle cramps, etc.).
Clinical picture of the disease
The inflammatory process manifests itself in the form of general symptoms characteristic of this pathology. There are varying intensity of symptoms depending on the form of the disease.
Among the common signs:
- frequent bowel movements;
- increased gas formation;
- rare urination;
- fever;
- vomit;
- dehydration;
- dry mouth and skin;
- general weakness;
- symptoms of peritonitis, one of which is diarrhea accompanied by dark blood clots.
It should be noted that the most striking symptom is sharp pain in the left side of the abdomen, which is observed in all patients with ischemic colitis. It is characteristic that pain is felt simultaneously in different parts of the body. Most often this is the left hypochondrium, lower abdomen, left iliac artery.
In rare cases, pain is observed around the navel, in the pit of the stomach. Sometimes pain appears under the shoulder blade, in the back of the head, in the neck, and in the lumbosacral region.
The nature of the pain is also quite varied. These are attacks, contractions, aching, increasing, dull, cutting pain. There is also constant pain, intensifying from time to time.
Causes of pain
There are many factors that provoke pain. This:
- Load associated with digestive processes.
- A large amount of food consumed at one time. The type of food can also be a provocateur: cold, spicy or very sweet dishes, dairy products, difficult-to-digest fiber.
- Irregular bowel movements.
- Exceeding the permissible physical activity in adults.
- Disturbances in the functioning of the gastrointestinal tract.
- Weight loss caused by reluctance to eat due to fear of renewed pain, which can provoke hunger pains.
Patients can eliminate most of the factors of pain and symptoms of ischemic colitis on their own by following a diet and proper diet, dosing physical activity.
Causes of the disease
The main cause of ischemic colitis is a decrease in blood flow to a certain area of the colon. The following conditions can cause ischemia:
- atherosclerosis of the aorta and arteries of the large intestine;
- occlusion of the vessels of the large intestine as a result of trauma, thrombosis;
- shock of any origin;
- stroke;
- massive bleeding;
- intestinal infection with severe dehydration;
- abdominal aortic aneurysm;
- congestive heart failure;
- systemic vasculitis;
- severe anemia;
- blocking of the intestinal lumen with a hernia or tumor;
- complications after surgery on the abdominal organs.
Variants of the course of the disease:
- Occlusive ischemia. When the lumen of the vessel is completely blocked (occluded), acute ischemic colitis develops. The area of damage to the colon will depend on the diameter of the vessel and the duration of occlusion, and the possibility of developing collateral blood flow. In case of incomplete overlap, chronic colitis is formed.
- Nonocclusive ischemia. Occurs when blood pressure decreases in the vessels supplying the intestines. A chronic form of pathology usually develops.
Characteristics of colitis
Colitis is an inflammatory disease that affects the mucous membrane of the large intestine . Its development is provoked by pathogenic microorganisms penetrating the body - staphylococci, streptococci. The disease also occurs due to various intoxications.
Typically, the development of such a disease is influenced by several factors.
Colitis can occur in acute or chronic form.
Note! Most often, this pathology is diagnosed in women aged 20 to 60 years and men aged 40 to 60 years.
Diagnostics
- General examination and palpation. There is soreness and tension in the muscles of the anterior abdominal wall around the navel or in the iliac regions.
- Digital rectal examination. Upon examination, blood is visible in the rectum.
- Colonoscopy. Endoscopic examination of the large intestine can identify foci of hemorrhage in the wall of the organ. Additional information is provided by a biopsy - tissue sampling for histological examination.
- Irrigography. X-ray contrast examination of the colon determines filling defects in areas of ischemia (impaired blood flow). This is not a permanent symptom and disappears quickly, so barium enema should be performed at the first signs of ischemic colitis. If time is lost, the filling defect is not detected. Necrotic ulcers and strictures may be visible.
- CT scan. Allows you to exclude other causes of abdominal pain and identify signs of circulatory disorders in the intestines.
- Angiography. Used to assess the level of vascular obstruction.
Differential diagnosis is carried out with the following conditions:
- ulcerative colitis;
- Crohn's disease;
- diverticulitis;
- intestinal obstruction;
- colon cancer.
The final diagnosis is made after colonoscopy with biopsy, irrigography, and computed tomography.
How is ischemic colitis diagnosed?
Ischemic colitis can be difficult to diagnose. It can easily be mistaken for inflammatory bowel disease, a group of diseases that includes Crohn's disease and ulcerative colitis. Ischemia can be suspected by the presence of abdominal pain in the left side of the abdomen, often accompanied by diarrhea, nausea, vomiting, and rectal bleeding. There may also be blood in the stool instead of bleeding.
Particular attention should be paid to age (over 60 years), although the disease also occurs in younger people.
Further diagnostics are necessary in order to:
- determine the location of intestinal damage;
- find out the extent of the lesion;
- provide medical assistance in a timely manner;
- promptly prevent the development of possible complications.
Diagnosis of ischemic colitis consists of several stages: medical history, physical examination, laboratory and instrumental diagnostic methods.
Anamnesis collection.
The proctologist studies the medical history (symptoms, chronic diseases - very important, previous operations) and prescribes several diagnostic tests. When collecting anamnesis, it is necessary to pay attention to the localization of pain, the connection with physical activity and food intake, as well as the presence of blood in the stool.
Physical examination.
On external examination, asthenia and low body weight are possible, but this is not necessary and does not always occur (with a long-term disease).
When palpating the abdomen
noted:
- soreness (mainly on the left, in the lower abdomen, but possibly throughout the abdomen);
- bloating is usually moderate;
- splashing noise.
During auscultation of the abdomen
There is a systolic murmur over the abdominal aorta, which is one of the main and reliable signs of ischemic colitis. It should be taken into account that systolic murmur is absent when the vessel is narrowed or occluded, so its absence does not exclude intestinal ischemia.
Further laboratory and instrumental diagnostic tests may include the following:
- Abdominal ultrasound or CT scan
, which provides images of blood vessels (using contrast and Doppler). - A mesenteric angiogram
is an imaging test that uses x-rays to see the arteries and determine the location of the blockage. - Complete blood test
to check white blood cell levels. If a high white blood cell count is detected, this may indicate acute IR. - Tissue biopsy
followed by histopathological examination is necessary to exclude a malignant process. - Colonoscopy
, which allows you to examine the condition of the rectal mucosa, the presence of narrowing of the lumen and at the same time perform a biopsy.
Principles of treatment
Therapy for ischemic colitis begins with diet and medication. The operation is rarely performed and is indicated only in the presence of conditions that threaten the patient’s life.
Diet
General principles of nutrition for ischemic colitis:
- Frequent and small meals. 5-6 meals with decreasing portion sizes are recommended. Dinner should be 2-3 hours before bedtime.
- Steamed and boiled food. Fried foods are not recommended until complete recovery or stable remission.
- Drinking regime. You need to drink up to 1.5-2 liters of clean water per day, unless there are contraindications (severe heart and kidney diseases).
The list of products is presented in the table.
| Recommended Products | Not Recommended Products |
|
|
With a widespread process, the patient is transferred to parenteral nutrition.
Drug therapy
Depending on the specific clinical situation, the following medications are prescribed:
- Electrolyte solutions. Replenish fluid loss during bleeding and diarrhea.
- Drugs that normalize blood flow. They speed up the work of the heart muscle and lungs, increase the flow of oxygen into the intestines.
- Antibacterial drugs. Indicated for necrosis of the intestinal wall. Suppress the growth of pathogenic microorganisms, prevent the development of peritonitis (inflammation of the peritoneum).
- Vitamins. Prescribed during the rehabilitation period to improve the general condition and normalize the functioning of internal organs.
- Probiotics. Indicated after a course of antibacterial therapy to restore intestinal microflora.
Surgical therapy
Indications for surgery:
- extensive intestinal necrosis due to impaired blood supply;
- perforation of the intestinal wall;
- progressive bleeding;
- peritonitis;
- sepsis;
- intestinal obstruction;
- colon tumor.
An intestinal resection is performed - excision of a part of an organ affected by necrosis. The volume of the operation depends on the extent of the process. The ends of the intestinal tube are compared and sutured. The abdominal cavity is inspected and the pus is removed. In case of extensive damage, when it is not possible to match the ends of the intestine, a stoma is formed - an opening on the front wall of the abdomen for the removal of feces.
Complications and prognosis for life
Without treatment, ischemic colitis leads to the development of complications:
- intestinal perforation;
- peritonitis;
- sepsis;
- narrowing of the intestines;
- intestinal obstruction.
If complications develop, surgical treatment is indicated.
The prognosis is favorable with timely diagnosis of the pathology. After prescribed therapy, stable remission of the disease can be achieved. Relapse occurs in 5% of cases. In advanced situations, the development of peritonitis and sepsis can lead to death.
Prevention
Since the exact cause of ischemic colitis cannot always be determined, it is difficult to talk about its prevention. You can reduce the risk of developing the disease if you follow the recommendations:
- give up bad habits: smoking, drinking alcohol;
- promptly treat diseases of the large intestine and cardiovascular system;
- monitor your weight, blood pressure, and cholesterol levels in your blood.
When the first signs of the disease appear, you need to consult a doctor - therapist, gastroenterologist, or surgeon. It is important to remember that pain and bleeding occur with various pathologies, and only after examination can an accurate diagnosis be made. Delay is dangerous to health and life.
In continuation of the topic, be sure to read:
- Rectal fissure: causes, symptoms and treatment of pathology
- Causes of bloating and increased gas formation, treatment methods
- Rectal cancer: symptoms, stages, treatment and prognosis for life
- More about hemorrhoids: causes, symptoms and treatment methods
- Details about bowel cancer: stages, symptoms, treatment and prognosis
- Irritable bowel syndrome: symptoms and treatments
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- Sigmoiditis (inflammation of the sigmoid colon): symptoms and treatment methods
- Diseases of the large intestine: symptoms and signs of the disease, treatment
- Nonspecific ulcerative colitis: causes, symptoms and treatment methods