Description
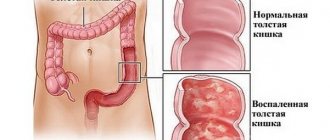
Chronic colitis is a common disease of the large intestine, which is characterized by chronic inflammatory damage to the mucous, submucosal and muscular membranes of the colon, with a severe course of the disease with degeneration of its own nerve fibers, as well as dysfunction of the intestine. The dysfunction includes a motor and secretory component. Chronic colitis is often combined with inflammation in the small intestine or stomach. There are the following types of chronic colitis: 1. Infectious (often after an episode of dysentery or salmonellosis). 2. Pseudomembranous chronic colitis develops after taking antibiotics. 3. Ischemic – with circulatory disorders. 4. Radial. 5. Medicinal. 6. Eosinophilic. 7. Lymphocytic. 8. Collagen. The pathological process in chronic colitis can be localized on one side of the intestine, for example, right-sided colitis, proctosigmoiditis, or it can be widespread. In the latter case, colitis is called total. Chronic colitis was identified as a separate nosological form by V.P. Obraztsov (1895), but in the USA and some other countries it is still not recognized as an independent disease. These positions are currently being actively reviewed.
Diagnosis of the disease
If symptoms are present, it is necessary to diagnose the disease. It is performed by a therapist or gastroenterologist. All data and symptoms must be presented. Enterites are divided into several types.
Etiological classification (by causes) of colitis:
- Infectious (consequences of intestinal infection);
- Nutritional (poor nutrition);
- Allergenic (if you are allergic to food);
- Intoxication (result of poisoning);
- Radiation (receiving radiation);
- Ulcerative (consequences of an ulcer of the mucous membrane).
When diagnosing a disease, a doctor must confidently make a diagnosis. There are diseases with symptoms similar to chronic colitis:
- Bowel cancer;
- Any disease of the digestive organs;
- Appendix;
- Enteritis.
For a reliable analysis, a comprehensive study is carried out. The medical history needs to be analyzed. Using the following methods, the area and damage to the intestine are identified, the severity is determined, and treatment is prescribed.
- A general and biochemical blood test is carried out to analyze the condition of the body organs;
- Scatological examination of stool is necessary to study the level of amino acids, ammonia and fiber;
- Examination of an x-ray of the colon;
- Colonoscopy is a method for identifying the source of infection and atrophic changes in the intestine;
- Irrigoscopy - using this method, changes in relief in the intestinal mucosa are detected;
- Ultrasound of internal organs and study of their structure (distal colitis).
Causes
Chronic colitis is a polyetiological disease. A combination of several factors is often necessary for the development of the disease. A predisposing factor for the occurrence of chronic colitis is a violation of diet, unbalanced nutrition, improper diet, alcohol abuse, hypo- and vitamin deficiency. A. The most common etiological factor is previously suffered infectious diseases of the intestinal group - for example, dysentery (shigellosis), salmonellosis, yersiniosis. A special form of chronic colitis is the so-called post-dysenteric colitis, but this diagnosis is considered legitimate only within 3 years after an episode of dysentery . B. In addition to bacteria, the inflammatory process can be caused by protozoa or fungi. Particular importance is given to Giardia and Balantidia. B. When intestinal dysbiosis is diagnosed in a patient, the saprophytic flora that normally inhabits the intestines may also become active. D. The role of intoxication in the development of chronic colitis - both exogenous (poisoning) and endogenous - in liver or kidney failure has been determined. D. Damage to the mucous membrane from radiation exposure. Radiation colitis can occur after therapy for malignant neoplasms. E. Drug-induced colitis develops after taking certain medications. Most often, chronic colitis occurs while taking NSAIDs, salicylates, and antibiotics. G. Allergy. An allergic component is present in the mechanism of development of chronic colitis. H. Enzyme metabolism disorders. The greatest clinical significance is lactose deficiency, which contributes to impaired hydrolysis, and this in turn leads to irritation of the mucous membrane. I. Poor circulation in the colon leads to the development of ischemic colitis. K. The presence of intercurrent diseases contributes to the development of chronic colitis - cholecystitis, pancreatitis, gastric ulcer and duodenal ulcer.
Chronic colitis on x-ray
Causes of the disease
The following factors influence the appearance of atrophic colitis in a person:
- hereditary predisposition;
- frequent stress or nervous breakdowns;
- non-compliance with the diet and constant consumption of junk food, as well as non-compliance with the diet prescribed for the treatment of other pathologies of the gastrointestinal tract;
- poisoning with toxic chemical compounds;
- long-term use of antibiotics or laxatives;
- infectious diseases;
- allergic reactions to certain types of products;
- diseases of the stomach and liver, leading to clinical transformations of the gastrointestinal tract;
- intoxication of the body due to alcohol poisoning;
- use of enemas and rectal suppositories;
- lack of physical activity.
Symptoms
Chronic colitis is characterized by dull, aching pain in different parts of the abdomen. It happens that the pain is cramping in nature, sometimes the pain is diffuse without clear localization. A distinctive feature is the intensification of pain after eating, physical activity, cleansing enemas, and subsidence after the passage of gas, bowel movements, the use of a warm heating pad, antispasmodics. There is an alternation of constipation and diarrhea, rumbling, flatulence (bloating), a feeling of incomplete bowel movement, the urge to defecate - tenesmus. Flatulence occurs due to concomitant dysbiosis and digestive disorders. The frequency of bowel movements reaches 5-6 times a day; impurities of mucus or blood in the form of streaks may be found in the stool. Due to inflammation in the rectum and sigmoid colon, pain can radiate to the anus. The course of this disease is chronic with periodic exacerbations. When palpating the abdomen, pain is detected along the course of the large intestine, alternation of its spasmodic and dilated areas, and sometimes a “splashing symptom” over the corresponding section. Among the clinical cases of chronic colitis, the most common are proctitis and sigmoiditis, which develop after suffering from dysentery, against the background of abuse of cleansing enemas, laxatives. The disease is manifested by pain in the left iliac region and in the anus, painful urge to defecate, and flatulence. Constipation in combination with tenesmus is often observed; the stool is light, sometimes like sheep feces, contains a lot of visible mucus, and often an admixture of blood and pus. On palpation, tenderness of the sigmoid colon, its spastic contraction or rumbling (with diarrhea) is noted. In some cases, an additional loop of the sigmoid colon is detected - dolichosigma (congenital malformation), which is the cause of chronic colitis. Examination of the anal area and digital examination of the rectum make it possible to assess the condition of its sphincter and identify frequently occurring concomitant pathologies that develop against the background of chronic proctitis (hemorrhoids, anal fissures, paraproctitis, rectal prolapse, etc.). Sigmoidoscopy is of great diagnostic importance, which allows you to assess the condition of the mucous membrane and identify the presence of ulcerative defects. For diagnostic purposes, an X-ray contrast examination of the intestine is performed, which reveals spastically narrowed intestines, or atony, and impaired peristalsis. Due to inflammation and infiltration of the intestinal wall, its relief changes. A general blood test reveals the presence of anemia (especially in the ulcerative nature of chronic colitis), leukocytosis, neutrophilia, and an increase in ESR. Associated symptoms: Pain in the intestines. Constipation. Constipation in the elderly. Change in appetite. Intestinal tenesmus. Leukocytosis. Flatulence. Malaise. Neutrophilia. Diarrhea (diarrhea). Irritability. Nausea. Increase in ESR.
Symptoms of intestinal inflammation
With any type of disease, and even when the inflammatory process begins, the body gives signs, the main thing is to recognize them.
Signs of chronic colon disease:
- Complete absence of stool for a week;
- Heaviness in the abdomen after and before meals, an external sign of an enlarged abdomen;
- Severe, frequent pain in the abdominal area, a pronounced symptom of the disease;
- Changes in stool, presence of blood and discharge;
- Frequent and false urge to go to the toilet “for the most part”, resulting in the release of mucus;
- Stool immediately after eating, early in the morning after waking up or before bedtime;
- Diarrhea with complications in the form of complete dehydration of the body;
- Bad breath, consequences of food stagnation in the stomach and intestines of a person;
- Constant rumbling in the stomach;
- Weakness and severe fatigue of the body, the immune system is weakened;
- Frequent belching with odor;
- Rapid weight loss;
- Pain in muscles and joints;
- Dolichosigma (constant constipation).
Causes of the disease:
- Bad habits;
- Infection;
- Long-term use of antibiotics, laxatives;
- Food and drug allergies;
- Metabolic disorders of the body;
- Inactive lifestyle.
Treatment
Patients with chronic colitis are advised to strictly adhere to a diet; during periods of exacerbation, No. 4a is prescribed, which includes steamed meat and fish dishes, stale white bread, steamed omelettes, low-fat weak meat and fish broths, pureed porridge in water, soft-boiled eggs, jelly, decoctions and jelly from blueberries, bird cherry, pear, quince, rose hips, tea, coffee and cocoa in water. As the exacerbation subsides, diet No. 4b is prescribed; dry biscuits, cookies, soups with boiled cereals, noodles and vegetables, a casserole of boiled vegetables, porridge with milk, mild cheese, fresh sour cream, baked apples, jam, and butter are added to the diet. During the period of remission, they switch to the 4b diet, which includes less mechanically gentle processing of food: all dishes are given unprocessed, lean ham, soaked herring, raw vegetables and fruits, and juices are added. Dill, parsley, jellied fish, tongue and black caviar are also allowed. If the clinical picture is dominated by stool retention, then foods containing an increased amount of dietary fiber (vegetables, fruits, grain products, especially wheat bran) are indicated. Bran must be poured with boiling water for 20-30 minutes, then drained and added to porridge, soup, jelly, or consumed in its pure form with water. The dose of bran is from 1 to 9 tablespoons per day. After eliminating constipation, you should continue to take them in quantities that ensure independent bowel movement once every 1-2 days. It is better to eat bread with a high bran content. Astringent, adsorbent drugs are indicated when diarrhea syndrome predominates; white clay 1 g is prescribed; calcium carbonate 0.5 g, dermatol 0.3 g in the form of a shaker before meals 3 times a day). If there is no effect, which is usually associated with concomitant dysbacteriosis, antibacterial drugs are prescribed for 7-10 days (enteroseptol, intestopan 1 tablet 3 times a day, nevigramon 0.5 g 4 times a day, nitroxoline 0.05 g 4 times per day or Biseptol-480, 2 tablets 2 times a day). In case of increased gas formation, activated carbon is prescribed 0.25-0.5 g 3-4 times a day, infusion of peppermint leaf, chamomile flowers. For patients with atonic variants of impaired intestinal motor function, it is advisable to prescribe Raglan (cerucal) 0.01 g 3 times a day; for spastic forms of impaired motor function - anticholinergic and antispasmodic drugs (no-spa 0.04 g 4 times a day, papaverine hydrochloride 0.04 g 3-4 times a day, platiphylline hydrotartrate 0.005 g 3 times a day, metacin 0.002 g 2 times a day). For watery diarrhea of various origins, imodium 0.002 g 2 times a day can be used as a symptomatic remedy. In order to increase the body's reactivity, aloe extract (1 ml/day, 10-15 injections) and pelloidin (orally 40-50 ml 2 times a day 1-2 hours before meals) are prescribed under the skin. Physiotherapy plays an important role in the complex therapy of chronic colitis. Electrophoresis with analgesics, calcium chloride and zinc sulfate is recommended. Diadynamic currents and amplipulse therapy are indicated for patients with hypomotor variants of colitis. For proctosigmoiditis, microenemas with anti-inflammatory properties are prescribed (chamomile, tannin, protargolov), for proctitis - suppositories (Anestezol, Neoanuzol, etc.). After discharge from the hospital, it is recommended to take probiotics - bificol or colibacterin, 5 doses 3 times a day for 1 month. , decoctions and infusions of medicinal plants. For example, for colitis with a predominance of constipation, the following herbs are used: a) chamomile, buckthorn bark, parsley; B) calendula, oregano, senna leaf. When diarrhea predominates: A) alder fruits, mint, rose hips; B) sage, St. John's wort, nettle, bird cherry; C) flax seed, blueberries, cinquefoil, dill. The components of each collection should be mixed in equal quantities, pour 2 tablespoons of the mixture into 250 ml of boiling water, leave for 20 minutes (preferably in a thermos). Strain and take in the morning on an empty stomach and at night before bed. Each of the fees is accepted for a month, sequentially. Courses can be repeated 2 times a year. The ability to work of patients with moderate and severe forms of chronic colitis, especially those accompanied by diarrhea, is limited. They are not shown types of work associated with the inability to maintain a diet or frequent business trips. Sanatorium-resort treatment is indicated in specialized balneological sanatoriums (Borjomi, Jermuk, Druskininkai, Essentuki, Zheleznovodsk, Pyatigorsk, Truskavets). Psychotherapeutic methods of treatment play an important role in therapy; group and individual psychotherapy are recommended.
Symptoms of the disease
Basically, the clinical picture depends on the area and location of inflammation, as well as the severity of erosive colitis. Since this disease is characterized by inflammatory processes in the rectum, the first signs of colitis will be:
- the presence of diarrhea (diarrhea), sometimes with pus and mucus;
- stomach ache;
- constant weakness, loss of weight and appetite;
- nausea, heaviness, vomiting;
- unpleasant taste in the mouth, belching.
Sometimes the process alternates between periods of exacerbation of symptoms and remission. As the condition worsens, people complain of:
- joint pain;
- the appearance of ulcers in the area of the oral mucosa;
- redness and swelling of skin areas;
- inflammatory processes of the eyes.
In the most severe cases, the temperature rises, the heartbeat accelerates, and blood appears during bowel movements. Factors that aggravate the condition are the presence of an infectious disease or stress.
Acute colitis
In almost all cases, intestinal inflammation is accompanied by problems with the stomach and small intestine. During acute colitis, symptoms manifest themselves in a sharp form and are often accompanied by pain.
In acute colitis, there is an increase in bowel movements up to 5-6 times a day and a mild aching pain in the stomach. The stool is usually mushy, possibly with a small amount of mucus, blood, or pus.
If you ignore the symptoms and do not treat the disease, there is a serious threat of its transition from acute to chronic, sometimes even with serious complications.
Chronic colitis
Often, erosive colitis does not make itself felt, and the onset of the process occurs unnoticed with sluggish symptoms, sometimes with acute outbreaks.
Some of the factors that aggravate the condition may be:
- incorrect or unobserved diets;
- physical and mental fatigue;
- presence of viral infections;
- stress;
- diseases of other internal organs.
Remember that for chronic colitis, treatment will not completely relieve you of the disease, but will only stop the progression and can prolong remission.
Clinics for treatment with the best prices
Price
Total: 644in 35 cities
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| K+31 on Lobachevsky | +7(499) 999..show Recording +7(499) 999-31-31+7(800) 777-31-31 | Moscow (metro Prospekt Vernadskogo) | rating: 4.4 | 84340ք |
| K+31 in Moscow City | +7(499) 999..show Recording +7(499) 999-31-31+7(800) 777-31-31 | Moscow (Mezhdunarodnaya metro station) | rating: 4.4 | 40390ք |
| K+31 Petrovsky Gate | +7(499) 116..show Recording +7(499) 116-77-31+7(499) 999-31-31 | Moscow (m. Trubnaya) | rating: 4.4 | 76550ք |
| Blagodatnaya Clinic on Yuri Gagarin Avenue | ..show Record +7 | St. Petersburg (metro station Elektrosila) | — | 7300ք (90%*) |
| St. Andrew's Hospitals in Korolev | +7(495) 518..show Appointment +7(495) 518-92-70+7(495) 518-92-72+7(495) 518-92-80+7(495) 518-92-81 | Korolev | rating: 4.4 | 9230ք (90%*) |
| Clinic of functional disorders on Gabrichevsky | +7(495) 363..show Appointment +7(495) 363-07-54+7(499) 654-08-00 | Moscow (metro station Shchukinskaya) | rating: 4.6 | 12505ք (90%*) |
| Medicine-Plus on Volgogradsky Prospekt | +7(495) 911..show Appointment +7(495) 911-93-00+7(495) 676-10-07+7(925) 793-45-41 | Moscow (metro station Proletarskaya) | rating: 4.7 | 14500ք (90%*) |
| Clinic No. 1 in Lyublino | +7(499) 519..show Appointment +7(499) 519-35-40+7(495) 641-06-06+7(495) 770-60-60 | Moscow (metro station Lyublino) | rating: 4.8 | 17570ք (90%*) |
| Best Clinic on Novocheryomushkinskaya | +7(499) 519..show Appointment +7(499) 519-33-09+7(499) 490-89-29 | Moscow (m. Profsoyuznaya) | rating: 4.7 | 17643ք (90%*) |
| Family doctor on 1st Miusskaya | +7(499) 969..show Appointment +7(499) 969-25-74+7(495) 126-99-31+7(926) 800-07-19 | Moscow (metro station Novoslobodskaya) | rating: 4.6 | 18830ք (90%*) |
| * — the clinic does not provide 100% of the selected services. More details by clicking on the price. | ||||
Causes of development of chronic colitis
- Acute intestinal diseases suffered in the past - dysentery, salmonellosis, foodborne toxic infections, typhoid fever, yersiniosis, etc. Particularly important is given to past dysentery and yersiniosis, which can take a chronic course. Many gastroenterologists propose to distinguish post-dysenteric colitis. According to A.I. Nogaller (1989), the diagnosis of post-dysenteric colitis can only be valid during the first three years after acute dysentery. In the future, in the absence of bacterial carriage, the development of chronic colitis is based on various other etiological and pathogenetic factors, in particular, dysbacteriosis, sensitization to automicroflora, etc.
Causes of chronic colitis
[9], [10], [11], [12], [13], [14], [15]
Symptoms of spastic colitis
Impaired intestinal motility is accompanied by painful cramps, bloating, and gas formation.
The pain often occurs at night, in the morning or after eating. Spastic colitis also manifests itself as alternating loose stools and constipation.
Chronic spastic colitis develops due to a lack of fiber in the diet; frequent suppression of the urge to defecate can also trigger the disorder.
With this form of the disease, the patient suffers from insomnia, headaches, and fatigue. The process of bowel movement can occur in 2-3 stages, both predominantly dry and dense. Treatment in this case is long and requires compliance with certain rules.
Constipation is one of the manifestations of spastic colitis.
In case of illness, nutrition plays an important role, with which you can reduce the manifestation of unpleasant symptoms.
For systematic constipation, it is recommended to eat more fruits and vegetables, which contain fiber and bran. You should also drink enough water - at least 2 liters per day.
Some foods can cause constipation, so it is important to monitor your body’s reaction to food (if, after eating certain foods, problems with bowel movements begin, discomfort appears, etc., it is better to stop eating such food).
The main symptoms of spastic constipation are sharp abdominal cramps, bloating, rumbling and increased gas production. In this case, defecation occurs once every few days.
Spastic colitis in children
Spastic colitis in children often occurs as a complication of infectious diseases of the gastrointestinal tract (intestinal, rotavirus infection, etc.). The disease causes high fever, diarrhea (at the beginning there may be constipation), pain, mucous or blood in the stool (depending on the infection), weakness.
Vivid signs of colitis in children appear after a few days (on average after 3 days), and colitis often occurs in combination with gastritis or enteritis. In advanced cases, the child may become severely dehydrated.
Treatment requires the use of enterosorbents, antibiotics, and drugs to restore water and electrolyte balance. Self-medication in this case is unacceptable.
With chronic spastic colitis, children experience dull abdominal pain, stool disturbances, bloating, fatigue, insomnia, low hemoglobin, and weight loss. The disease progresses in waves, with acute attacks followed by long-term remissions.
A prolonged course of colitis can cause intestinal obstruction, anemia, adhesions in the intestines, and inflammation of the peritoneum.
Frequent diarrhea and constipation can cause anal fissures, intestinal prolapse, and changes in the mucous membrane.
During treatment, special attention should be paid to the child’s nutrition - food should be gentle on the intestines and heat-treated. Spicy, sour, salty, and fried foods should be completely excluded from the children's menu.
The child should be in a calm environment and not be subjected to nervous and physical stress. It is recommended to take mineral waters to normalize digestion, and resort treatment during periods of remission.
Endogenous causes
- Constant pain in the stomach. This sign of the disease brings a lot of discomfort to the patient. The pain is aching or pulling. Only in rare cases can gastric discomfort be relieved by taking antispasmodics. In order to alleviate his condition, the patient can drink No-shpa, Spazmalgon, Nurofen and Analgin. However, before you relieve discomfort arising from intestinal discomfort, you should consult a doctor. As a rule, discomfort increases after a meal. In some cases, it weakens, but as the disease progresses, the pain returns.
- Dyspeptic disorder. A person diagnosed with this pathology may complain of lack of appetite. This disorder also manifests itself in the form of nausea, belching, heartburn, and a feeling of bitterness in the mouth.
- Loss of body weight. This is also a manifestation of dyspeptic disorder. This symptom is a direct consequence of lack of appetite.
- Flatulence. Almost every person who is faced with this pathology experiences bloating. Moreover, flatulence occurs regardless of food intake. The patient's stomach will be bloated, even if he has not eaten at all. The manifestation of this symptom is the result of impaired digestive functioning. The patient may also experience diarrhea or constipation. Often these gastrointestinal disorders replace each other.
Taking medications
The next type of medications, glucocorticosteroids, is prescribed in particularly exceptional cases, as they have a powerful effect and cause side effects. The most common medications in this group include Prednisolone and Dexamethasone.
- Viruses and bacteria. There are a lot of them. The main ones include: rota viruses, campylobacter, noravirus, salmonella, etc.
- Long-term use of antibiotics in the treatment of prostatitis, as well as other organs associated with the digestive and urinary systems. During the use of drugs, the balance of the microflora of the gastrointestinal tract is disrupted.
Traveler's diarrhea occurs more often in young tourists compared to tourists in older age groups. Obviously, this is due to the more risky behavior of young people in terms of the risk of infection and different eating habits between young people and older people. There were no significant differences in the incidence of traveler's diarrhea between men and women.
Diagnosis of spastic colitis
With spastic colitis, a variety of symptoms are observed.
Characteristic signs of this disease are abdominal cramps (or aching pain), most often pain occurs from the left iliac region, as well as stool disorders (loose stools and constipation). During examination, a specialist can determine intestinal pathology (expansion or contraction) during palpation.
If spastic colitis is suspected, an endoscopic examination is prescribed - examination of the rectal mucosa using a sigmoidoscope or a special probe, which reveals inflammatory processes, atrophy, intestinal dystrophy, mucous plaque (pronounced signs of the disease).
In the acute stage, the mucosa is loose, covered with erosion and pinpoint hemorrhages.
With intestinal atrophy, the mucous membrane is pale, covered with a thin network of vessels, dry (as there is no mucus), and intestinal tone is reduced.
To exclude other pathologies, an ultrasound scan, a general analysis of blood, urine, feces, and examination of stool in the laboratory to identify gastrointestinal pathologies may be prescribed.
[7], [8], [9], [10], [11], [12], [13]
Complications of erosive colitis
This disease can develop gradually over a long time. The complications associated with it are general or local.
Common complications manifest themselves in organs such as:
- liver;
- joints;
- leather;
- oral cavity (stomatitis).
Local ones include :
- megacolon;
- heavy blood loss;
- malignant tumors in the colon area;
- perforation.
If putrefactive processes occur, this threatens to infect the entire body. In addition, during them, stool has a disgusting, rotten smell. Fermentation processes and the formation of gases may occur, which swell the intestines and cause pain in the heart area.
Treatment of spastic colitis
The principle of treating spastic colitis is based on normalizing stool and reducing unpleasant symptoms.
During the period of exacerbation, antiseptic drugs are prescribed, which improve well-being in a short time, however, the recommended course of treatment should not be exceeded, since these drugs can disrupt the intestinal microflora. To reduce pain, antispasmodics (No-spa, Decitel) are prescribed; in the hospital, the doctor prescribes cholinergics or adrenergic blockers, but such drugs have severe side effects, so they should be taken only under the supervision of a specialist.
When colitis occurs, a large amount of mucous secretion forms on the walls; to reduce the irritating effect, drugs with an enveloping effect (calcium carbonate) can be prescribed.
In case of increased gas formation, enterosorbents are prescribed (enterosgel, activated carbon), acedin-pepsin is prescribed to reduce high acidity, and enzyme preparations are also prescribed to improve digestive function.
If the microflora is disturbed, you should take a course of prebiotics or probiotics (only after antiseptic drugs).
To improve general well-being, multivitamins are prescribed, usually intramuscularly.
For constipation, it is better to use oil-based laxatives or herbs that do not cause irritation to the mucous membrane. Vaseline oil (1 tablespoon per day), olive oil (1/4 cup per day), and castor oil (1 tablespoon per day) show good effectiveness.
If frequent nervous overstrain, stress, etc. are observed, a course of sedatives, soothing infusions, and mild sleeping pills is recommended.
Folk remedies for spastic colitis
Treatment with folk remedies primarily involves taking herbal infusions and enemas.
For enemas, it is recommended to prepare an infusion of calendula and chamomile (1 tablespoon of a mixture of herbs, brew 200 ml of boiling water, strain after cooling). During the procedure, it is necessary to hold the medicinal infusion inside for a few minutes and repeat the procedure 2 times a day. The course of treatment is 1 – 3 weeks, depending on the severity.
For pain and increased gas formation, anise seeds help well, the infusion of which should be replaced with regular tea (1 tsp per 200 ml of water).
For constipation, traditional medicine recommends taking raw onion juice before meals - 1 tsp. 3 times a day.
For nervous tension, tea with mint or lemon balm (3 times a day) effectively helps.
For spastic colitis, traditional medicine recommends making microenemas with honey - dissolving 50-100 g of honey in warm boiled water.
[14], [15], [16], [17], [18]
Nutrition for spastic colitis
From the first days of treatment, the patient should follow a special diet.
The diet should be varied and include foods with a lot of fiber (not fresh gray wheat bread, vegetables, cereals).
You need to eat small portions up to 6 times a day.
During periods of exacerbation of the disease, adult patients are recommended to fast for the first two days, then start the morning with a glass of water, eat oatmeal for lunch (if you are worried about loose stools, it is better to prepare liquid rice porridge), and vegetable soup for dinner.
The next day, you can add boiled meat, fish, and eggs to your diet.
You should exclude foods that irritate the intestines (legumes, nuts, mushrooms, poultry or fish skin, meat with tendons).
During acute periods of the disease, it is better to eat fruits and vegetables stewed; as acute symptoms subside, you can add raw foods to the diet; at first, it is better to peel any fruits and vegetables.
Diet for spastic colitis
Diet is of primary importance in normalizing the functioning of the digestive system.
If you have loose stools, it is better to include in your diet liquid well-cooked porridges (rice, corn), jelly, boiled puree soups, stewed grated vegetables and fruits, baked or boiled meat, and fish.
For frequent constipation, it is better to eat raw vegetables and fruits, prunes, freshly squeezed juices from vegetables and fruits, baked goods with bran, boiled or baked pumpkin, and beets.
[19], [20], [21]
Prevention
To prevent the development of a disease such as atrophic colitis, certain rules should be followed:
- stop drinking alcohol and smoking;
- use medications only as prescribed by a doctor;
- follow the principles of healthy eating;
- be careful when working with toxic substances and pesticides;
- if a pathology occurs that can lead to the appearance of atrophic colitis, it is recommended to immediately consult a doctor and, if necessary, resort to treatment in a hospital;
- to live an active lifestyle;
- undergo a medical examination regularly for preventive purposes.
Video on the topic:
References: https://www.mosmedic.com/hronicheskij-kolit-kishechnika-neyazvennoj-etiologii.html https://yandex.ru/health/turbo/articles?id=4413 https://www.nrmed.ru /rus/dlya-vzroslykh/proktologiya/kolit-kishechnika/ https://www.kleo.ru/items/zdorovie/kolit-kishechnika-simptomi.shtml https://www.rossimed-clinic.ru/stati-pro- gastroenterologiyu/kolit-kishechnika/ Notes from the author of the article, based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/13/2020
Prognosis of spastic colitis
With spastic colitis with frequent constipation, bloody diarrhea, intestinal obstruction may occur, and in some cases surgery may be required.
In most cases, the prognosis is favorable; therapy requires an integrated approach (medication, diet, and in some cases a consultation with a neuropsychiatrist may be necessary).
Spastic colitis can occur in acute or chronic form. The disease is caused by a functional disorder of the gastrointestinal tract, the main factors provoking the disease are stress, frequent overload of the body (both physical and nervous), and poor nutrition.
Source
Forms of colitis and causes of their occurrence
There are different forms of colitis:
- Spastic occurs as a result of suffering severe stress and nervous strain. The symptoms of spastic colitis are highly treatable, and the pathology itself does not cause any particular complications.
- Infectious - the result of infection of the intestines with various bacteria, including salmonella, pathogenic fungi, gonococci and other viruses.
- Parasitic – a consequence of the presence of helminths in the human body. These are mainly flagellated parasites - Giardia.
- Intoxication is the result of exposure to harmful poisons (mercury, arsenic, lead salt) on the body.
- Drug-induced illness occurs through long-term use of medications, namely laxatives or antibiotics.
- Concomitant is a consequence of irritation by products that are not completely digested and get on the mucous membrane of the colon. It occurs due to improper functioning of the pancreas and stomach.
In addition, the causes of erosive colitis may be:
- mechanical effects (when a person abuses enemas due to frequent constipation);
- acute allergic reactions;
- serious food poisoning;
- alcohol abuse;
- poor nutrition.
Also in medicine, there are a number of unsafe factors that influence the development of the disease. These include:
- Genetic inheritance. Often people who have erosive colitis have relatives with a similar diagnosis.
- Environmental factors, namely air pollution and sanitary conditions.
- Taking anti-inflammatory non-steroidal drugs.
Treatment for adults
Non-infectious gastroenteritis and unspecified colitis should be treated taking into account the state of the digestive tract, since with this pathology almost the entire gastrointestinal system is involved in the inflammatory process.
When the cause of the disease is intoxication, gastric lavage is performed immediately, which helps prevent the absorption of toxic substances into the bloodstream.
When the cause of the disease is helminth infestation, an appropriate course of treatment is prescribed. In the initial phase of the disease, it is recommended to take enterosorbents. Smecta and activated carbon are prescribed. Drinking plenty of fluids is necessary. It is recommended to take medicinal mineral water and a decoction of medicinal plants. A therapeutic diet is prescribed, which must be followed for 10 days, and for another week after the symptoms disappear. If necessary, antibiotics are prescribed, the choice of which is made by the doctor based on the degree of the inflammatory process.
Enveloping drugs are also prescribed, which help restore damaged mucous membranes of the gastrointestinal tract. A saline solution is injected inside to prevent intoxication.
Vitamin therapy is carried out to strengthen the immune system and replenish the body's deficiency, which appears as a result of frequent vomiting and diarrhea.
Eubiotics are prescribed to normalize the microflora of the digestive tract.
Physiotherapy is also used for treatment, which includes:
- electrophoresis;
- mud applications;
- magnetic therapy;
- ultraviolet irradiation.
Drugs
Treatment of ulcerative colitis begins with the use of drugs that relieve intestinal inflammation and heal small cracks and wounds.
Preference is given to the following anti-inflammatory drugs: Medicines containing 5-acetylsalicylic acid - Mesacol, Kansalazine.
Sulfasalazine tablets and suspension with the active ingredient mesalazine relieve inflammation in ulcerative colitis well. The drug is prescribed for the treatment of exacerbations and as a prophylaxis. The daily dose and duration of administration are determined by the doctor.
All dosage forms of Sulfasalazine are contraindicated in case of severe liver/kidney diseases, bleeding disorders, or stomach or intestinal ulcers. During treatment, the following may occur: nausea, loss of appetite, flatulence, skin rash, headache.
Corticosteroids – Prednisolone, Budesonide. Hormonal drugs can relieve inflammation in any part of the intestine, but they have a number of contraindications and can cause a variety of side effects (night sweats, facial hair growth, insomnia, high blood pressure). Such medications are prescribed only in cases of severe or moderate colitis and for a period of 1–2 months.
Immunosuppressants – Cyclosporine-A, Azathioprine, Methotrexate, Infliximab, Azathioprine. They can also reduce inflammation, but do not act directly, but by suppressing the body's immune response. Immunosuppressants are not prescribed to children, pregnant women, or during lactation. During treatment, these medications may cause fatigue, headache, blurred vision, and nausea and vomiting. In addition to anti-inflammatory drugs, medications are used to help relieve symptoms.
Depending on the severity of the pathology, the attending physician prescribes one or more of the following medications:
- Antidiarrheals – Loperamide, Imodium. Medicines help restore normal stools, prevent intoxication and severe dehydration of the body. The use of antidiarrheal drugs is only possible after consultation with a doctor, because they can increase the chances of developing megacolon.
- Painkillers – Acetaminophen, Tylenol, Panadol. They help ease the act of defecation and relieve pain in the lower abdomen. For ulcerative colitis, it is strictly forbidden to use non-steroidal anti-inflammatory drugs, such as Ibuprofen, Aspirin.
- Vitamins and iron preparations - Totema, Ferrum-Lek, Alphabet Classic, Vitrum. Prescribed after stopping bleeding to replenish hemoglobin and prevent the development of iron deficiency anemia.
- Broad spectrum antibiotics - Cifran, Ciprofloxacin, Ceftriaxone. Prescribed to reduce body temperature and fight infection. The choice of the best medicine, dosage and duration of its use remains with the doctor.
Prognosis and prevention
The prognosis for chronic colitis is favorable, complications are rare, but if they do develop, the prognosis directly depends on the timeliness of treatment and the severity of intestinal damage.
To maintain stable remission, the following is recommended::
- eat properly and regularly, do not starve or overeat;
- engage in physical education and sports, do exercises, walk a lot;
- maintain a plentiful drinking regime - drink at least 1.5-2 liters per day;
- do not tolerate the urge to defecate, empty your bowels in a timely manner;
- control the quality of food and drink.
Prevention also includes timely consultation with a doctor when the first signs of trouble appear on the part of the gastrointestinal tract, and adequate treatment of infectious and inflammatory processes of any other localization.
Diagnostics
Diagnosis of chronic non-infectious (non-ulcerative) colitis:
Complaints from patients with chronic non-infectious (non-ulcerative) colitis:
- pain in the abdomen (in the lateral and lower abdomen, including at night, in the morning 6-8 hours after eating, and subsiding after defecation and/or passing of gas);
- stool disorders (alternating constipation and diarrhea);
- when diarrhea predominates (immediately after eating or in the morning) - watery stools with mucus;
- with a predominance of constipation, the stool is fragmentary, less often ribbon-like;
- incomplete bowel movement;
- tenesmus (false urge to defecate);
- bloating;
- excessive release of gases;
- nausea;
- belching;
- unpleasant taste in the mouth.
Objective research data:
- pale facial skin;
- coated tongue (white, gray;
- pain in the projection of the colon.
Instrumental studies of the intestine with a biopsy of the colon mucosa for the purpose of diagnosing chronic non-infectious (non-ulcerative) colitis:
- sigmoidoscopy (up to 20-25 cm from the anus): hyperemia, edema, bleeding and less often detected: erosion, mucus, atrophy or no changes are found;
- colonoscopy (up to 20-25 cm from the anus): hyperemia, edema, bleeding, and less often they reveal: erosion, mucus, atrophy (during colonoscopy, atrophy of the colon mucosa) or no changes are found.
Histological study of biopsy material of the colon mucosa for the purpose of:
- confirmation of chronic non-infectious (non-ulcerative) colitis with verification of the specific and severity of this colitis;
- exclusion of cancer, ulcerative colitis, Crohn's disease of the colon.
X-ray examinations of the colon to identify chronic non-infectious (non-ulcerative) colitis:
- irrigoscopy (narrowing of the lumen of the colon, detection of multiple haustrations, changes in the relief of the mucous membrane, changes in colon motility);
- CRT of the colon.
Laboratory tests of stool:
- bacteriological: stool analysis for dysbiosis (dysbacteriosis) of the large intestine;
- stool analysis for coprogram, eggs of worms and protozoa;
- stool occult blood test;
- other studies to exclude colitis or enterocolitis of other etiologies.
Laboratory blood tests for:
- toxocariasis;
- ascariasis;
- other helminthiases;
- intestinal giardiasis;
- intestinal candidiasis.
Differential diagnosis when a gastroenterologist excludes the following diseases:
- irritable bowel syndrome;
- nonspecific ulcerative colitis;
- Crohn's disease;
- ischemic colitis;
- pseudomembranous colitis;
- diverticular disease of the colon with diverticulitis;
- colon cancer;
- endometriosis;
- other diseases.
Treatment methods
Treatment is aimed at eliminating etiological factors and certain links in pathogenesis, relieving symptoms, reducing inflammation and preventing relapses.
Drug therapy
Treatment of pathology involves prescribing the following drugs:
- broad-spectrum antibiotics;
- intestinal antiseptics for the sanitation of the intestinal tract as a whole;
- antispasmodic drugs to eliminate spasms;
- painkillers and antipyretics;
- hormonal agents;
- sedatives for the psychogenic nature of intestinal pathologies.
, laxatives (for constipation), probiotic complexes, and vitamins are required
In the treatment of chronic colitis, sitz baths with antiseptic solutions, microenemas based on chamomile, sage, string, suppositories with anesthesin, belladonna, calendula, and sea buckthorn help. Resort therapy will help ensure stable remission.
Surgery
The need for surgery arises when complications arise , adhesions, acute intestinal obstruction, significant defects of the colon, massive bleeding and an extensive purulent-infectious process.
The main goal is to eliminate complications and prevent death with rapidly developing symptoms.
Folk remedies
Non-traditional methods of treatment include taking decoctions and tinctures, performing local procedures and sitz baths, microenemas with decoctions of medicinal herbs.
Popular means:
- Chamomile decoction with honey . 1 tbsp. l. dried flowers are poured into 500 ml of water, infused, filtered and drunk instead of tea during the day, adding a little honey. A decoction of chamomile with honey helps relieve inflammation and soothe irritated intestines.
- Decoction of oak bark . Oak bark, alder cones and birch buds are mixed, 2 tbsp. l. raw materials, pour 1 liter of boiling water and bring to low heat for 30 minutes. Drink 100 ml 4 times a day after meals, and also do microenemas. The product helps with bleeding, has an antiseptic and protective effect.
- Propolis tincture . For microenemas, take 300 ml of water and 1 tbsp. l. water tincture of propolis; for internal use, you can use alcohol or water tincture in the proportion of 200 ml of water per 1 tbsp. l. water and 1 tsp. alcoholic. Propolis is considered a natural antiseptic, it heals well, and helps relieve symptoms during exacerbation.
Doctors do not deny the effectiveness of traditional treatment methods, but they must correspond to the clinical picture and severity of the disease.
Diet
Chronic colitis does not require special dietary adjustments or adherence to strict therapeutic nutrition . It is enough to limit alcohol, salt, exclude coarse fiber and foods that irritate the stomach and intestines (citrus fruits, spices and seasonings, spicy dishes, marinades, canned food, preserves and smoked meats). Gas-forming and constipating foods (white cabbage, legumes) should be avoided.
Exclude sweet carbonated water from drinks (you need to degas it before drinking mineral water), rich natural citrus juices, thick fatty broths, alcohol, and fermented milk products. During an exacerbation, it is recommended to drink a decoction of rose hips, unsweetened dried fruit compote, and pumpkin juice.
Note! You should eat in small portions and often, the temperature of the food should be comfortable. A diet is required (at approximately the same time). Only complex therapy helps reduce the risk of relapse.
Physiotherapy
Physiotherapy for chronic colitis has a beneficial effect on the intestinal tract and enhances the effectiveness of drug therapy. Electrophoresis with antibiotics, zinc sulfate and calcium is useful.
For colitis with decreased peristalsis, manipulations with diadynamic currents and amplipulse therapy are performed. In chronic colitis, warming up is possible in the absence of high temperature and acute purulent process. For these purposes, take warm baths, perform mud wraps, paraffin therapy, and apply a heating pad.
Possible complications and consequences
If the disease is not treated, it can cause a number of complications. This mainly concerns ulcerative colitis. The consequences may be as follows:
- Perforation of the ulcer, which often results in peritonitis. In this case, the symptoms will be manifested by severe bloating and tension in the abdominal muscles, high fever, chills, a coating on the tongue, and general weakness.
- Gangrene of the colon and affected areas of the intestine. In this case, you may feel weakness, high temperature, and decreased blood pressure.
- Blood poisoning or spread of infection to other organs.
- Bleeding in the intestines (with chronic ulcerative colitis).
- The appearance of an oncological tumor is also possible.
Video - Chronic intestinal colitis: causes, symptoms, treatment of colitis.
Pathogenesis of chronic colitis
The main pathogenetic factors of chronic colitis are the following:
- Direct damage to the colon mucosa under the influence of etiological factors. This applies primarily to the influence of infection, drugs, toxic and allergic factors.
- Impaired immune system function, in particular, a decrease in the protective functions of the gastrointestinal immune system. Lymphoid tissue of the gastrointestinal tract functions as the first line of specific defense against microorganisms; Most of the body's Ig-producing cells (B lymphocytes and plasma cells) are found in L. propria of the intestine. The presence of local immunity, optimal synthesis of immunoglobulin A and lysozyme by the intestinal wall is a reliable protection against infection and prevents the development of an infectious-inflammatory process in the intestine. With chronic enteritis and colitis, the production of immunoglobulins (primarily IgA) and lysozyme by the intestinal wall is reduced, which contributes to the development of chronic colitis.
Pathogenesis of chronic colitis
Treatment of pathology
Drugs used to treat colitis:
- Antimicrobial agents - used in the treatment of infectious colitis, courses of antibiotics (Tsifran, Rifaximin), antiseptics (Enterofuril) are prescribed;
- Antispasmodics and anticholinergics - to relieve pain symptoms (No-spa, Drotaverine hydrochloride, Papaverine, Metacin, Atropine);
- Anthelmintic drugs – for the treatment of helminthic infestations;
- Enterosorbents – for the correction of microflora (Enterosgel, Polypefan, Polysorb, activated carbon);
- Prebiotics and probiotics - for the restoration of beneficial lacto- and bifidobacteria (Linex, Bifidumbacterin, Colibacterin, Normobakt, Bifikol);
- Anti-diarrhea medications (Loperamide, Imodium, Tanalbin, bismuth nitrate, oak bark infusion);
- Local remedies for the treatment of inflammation of the lower intestines - microenemas with chamomile, tannin, protargol, calendula, suppositories with belladonna, anesthesin, papaverine;
- Enzymes for the treatment of enzyme deficiency (Festal, Creon, Pancreatin);
- Anti-constipation medications – laxatives (sena alexandria preparations, Guttalax, Sorbitol);
- Immunomodulators.
With the aim of strengthening the body and its rehabilitation, physiotherapeutic methods are used: mud therapy, massage, acupuncture, as well as treatment with mineral waters at balneological resorts.
Treatment of ulcerative colitis stands alone among the treatment regimens used. This is a long-term, multifaceted therapy, carried out exclusively in a hospital, using complex drugs with numerous side effects:
- Biotherapy agents – Infliximab, Adalimumab.
- Preparations with acetylsalicylic acid - Pentas, Mezavant, Mesacol, Salofalk.
- Corticosteroids – Prednisolone, Methylprednisolone, Hydrocortisone.
- Immunosuppressants – Azathioprine, Methotrexate, Cyclosporine.
Diagnostic methods
Modern recommendations prescribe the following diagnostic measures necessary to confirm the diagnosis:
when collecting a history of the disease, it is necessary to pay special attention to the time of onset of the first symptoms, the connection of the pathology with drug intolerance, as well as trips to countries with unfavorable epidemiological conditions for intestinal infections; an objective examination reveals a lack of body weight, edema, as well as extraintestinal manifestations of UC; It is imperative to conduct a general and biochemical analysis of blood, urine and a coagulogram and identify anemia, thrombocytosis, leukouitosis, and hypoalbuminemia characteristic of UC; to exclude the infectious nature of the process, microscopic and bacteriological examination of stool is performed; if chronic colitis is suspected (ICD 10 code K51), stool should be examined for C. difficile toxin, especially with recent antibiotic therapy and hospital treatment; To exclude perforation of the large intestine due to immune inflammation, a plain X-ray of the abdominal cavity is performed; endoscopic examination of the colon mucosa - colonoscopy, sigmoidoscopy - is required for the initial diagnosis of ulcerative colitis, as well as for monitoring treatment; biopsy is performed from at least four different parts of the intestine
Microscopic signs of the disease include deformation of the crypts, a decrease in the number of goblet cells, crypt abscesses, and histiocytic infiltration of the lamina propria of the mucous membrane.
Use the interactive constructor to get a ready-made patient management protocol based on the latest clinical recommendations of the Russian Ministry of Health.
Directions of therapy
Treatment of ulcerative colitis (ICD 10 code K51) involves an integrated approach: prescription of drug therapy, diet correction and, if indicated, surgical intervention.
Pharmacological agents are used to induce and maintain remission. The first group includes rectal and systemic preparations of mesalazine and glucocorticosteroids.
In severe forms of the disease, it is advisable to prescribe a combination of GCS and azathioprine. Steroid withdrawal is carried out with a gradual dose reduction.
Biological therapy (infliximab, vedolizumab) is used as an adjunct to treatment.
If conservative therapy is ineffective, the possibility of surgical treatment should be considered.
Direct indications are intestinal bleeding, toxic megacolon, and perforation of the colon.
In addition, if patients have UC, their risk of developing colorectal cancer increases significantly.
Currently, the gold standard for surgical intervention for chronic colitis is considered to be colproctectomy with ileoanal pouch anastomosis, and the procedure can be performed in two or three stages.
Causes of colitis
As a result of numerous studies, the main causes of colitis have been established:
- side effects of pharmaceutical drugs that provoke the disorder
- acid-base balance (antibiotics, laxatives, NSAIDs, contraceptives, aminoglycosides);
- long-term exposure to toxic substances (mercury, phosphorus, arsenic);
- food and drug allergies;
- congenital functional deficiency;
- food poisoning, intestinal infections;
- violation of diet, lack of fiber and passion for fast food,
- the effect of alcohol;
- decreased immunity combined with psycho-emotional shocks;
- irritation of the intestines by coprolites resulting from chronic constipation.
In many cases, several causes occur simultaneously, and then the patient is diagnosed with combined colitis.
Classification and code according to ICD-10
What is atrophic colitis? This pathology involves damage to the intestinal mucosa, accompanied by its gradual destruction. In the international classification of diseases of the tenth revision, this disease is coded K52 (other non-infectious gastroenteritis and colitis).
The main classification suggests dividing this pathology depending on the course:
- acute atrophic colitis – characterized by rapid development and pronounced symptoms; atrophy of the mucous layer of the organ occurs.
- chronic atrophic colitis - exacerbations of the disease are replaced by remissions; When the disease becomes chronic, destructive changes are observed not only in the mucous membrane, but also in the ligamentous-muscular apparatus of the intestine.
As the disease progresses, atrophic colitis goes through several stages:
- Stage 1 (subatrophic colitis) – the lesion affects only the superficial layer of the intestine; At this stage, non-drug treatment (diet) is possible.
- Stage 2 – characterized by the severity of clinical symptoms and deterioration of the general condition.
- Stage 3 (complicated) – dystrophic changes in intestinal tissue are observed, which are irreversible; treatment is often surgical.
Symptoms of chronic colitis
Chronic colitis is characterized by pain localized mainly in the lower abdomen, in the flank area (in the lateral sections of the abdomen), i.e.
in the projection of the large intestine, less often - around the navel. The pain can be of a varied nature; it can be dull, aching, sometimes paroxysmal, spastic, or bursting. A characteristic feature of the pain is that it decreases after passing gas, defecation, after applying heat to the abdominal area, and also after taking antispasmodic drugs. Increased pain is observed when taking coarse vegetable fiber (cabbage, apples, cucumbers and other vegetables and fruits), milk, fatty, fried foods, alcohol, champagne, carbonated drinks. Symptoms of chronic colitis
Non-infectious colitis in a child
Treatment of non-infectious gastroenteritis in children does not require special intervention, with the exception of the toxic form. Non-infectious gastroenteritis in children manifests itself with quite severe symptoms. The child complains of pain in the navel area, which quickly spreads throughout the entire abdominal cavity. The pain intensifies after eating and stops abruptly. Abdominal bloating, colic, and loose stools are observed.
Traces of mucus are recorded in the stool. The child experiences vomiting and nausea. As a result of frequent vomiting and diarrhea, a baby may develop dehydration, which is manifested by dry mouth, lethargy, a strong feeling of thirst, pale and dry skin, the appearance of a gray or brown coating on the tongue, weakness and depression, and decreased appetite.
The disease in children develops as a result of severe stress, frequent infectious diseases, due to which immunity is reduced, poor nutrition, the presence of helminths, violation of basic hygiene rules, the presence of an allergic reaction to food, overeating and consumption of low-quality food or improperly processed foods.
To select the correct treatment tactics, an examination is necessary. A pediatrician examines a sick child to identify symptoms typical of the pathology. The presence of muscle noise of intestinal peristalsis, muscle weakness, the presence of plaque on the tongue, swelling of the pharynx, and muffled heart rate tones are determined. To clarify the nature of the disease, confirm or exclude infection, the following is prescribed:
- Blood test, urine test, copogram;
- Bacteriological examination of stool with an antibiogram;
- Serological studies;
- Hematocrit
If necessary, instrumental examinations are carried out:
- Ultrasound and fegds;
- Intragastric pH-metry.
Treatment of the child begins with gastric lavage if the disease is caused by toxicity. The doctor recommends drinking plenty of fluids and dieting, from which heavy foods should be excluded.
The child is given boiled water if he has symptoms of dehydration, and citroglucosolan or rehydron is added to the water. If the problem occurs in a baby, you should postpone feeding for a couple of hours and at this time give the baby a large amount of water.
The following are prescribed as treatment:
- Digestive enzymes and probiotics;
- Absorbing agents such as activated carbon, polypheran, polysorb;
- Temperature-reducing agents, as well as antibiotics (medications if necessary).
The dosage of drugs is chosen by the doctor based on the severity of the pathology and the weight category of the child. If a baby is fed artificial formula, he is prescribed rehydration drugs in certain quantities. In this case, feeding must be shifted by an hour. The correct diet plays a decisive role in therapeutic therapy.
Required:
Eliminate fermented milk products from the baby’s diet (for 1 – 2 weeks);
In the first days, only unsweetened vegetable and fruit purees should be included in the child’s menu. Gradually, the diet is expanded, adding lean chicken meat, chicken broth, cookies, fish, and eggs to the menu. It is allowed to return to the usual regimen after 7 days from the start of the diet.