What is colitis in a child?
Colitis is reported in cases of pain in the abdominal area. In these conditions, stool is disrupted and inflammatory processes in the intestine are observed during examination. As a rule, colitis begins in childhood. In adults, the chronic form is diagnosed. Therefore, the disease is considered one of the complex problems of childhood gastroenterology. Since the anatomical structure of the stomach of a newborn and infant differs from that of an adult, the disease at an early age of the child is accompanied by disturbances in the functioning of the intestines. Focal lesions in the form of enterocolitis occur on the walls of the small and large intestines.
Types of disease
Enteroseptol
In medicine, this disease is divided into several forms. Allergic colitis is very often diagnosed , since at this age babies are very sensitive to various allergens.
Children may also suffer from pseudomembranous colitis , which develops when taking antibiotics for too long. The basis of treatment for this disease is refusal to take them.
Spastic colitis in a child develops in cases where he eats only black bread, cereals and vegetables, and also often suppresses the desire to go to the toilet “in a big way”.
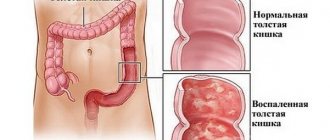
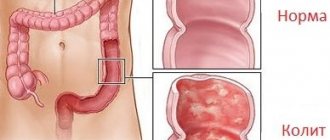
Ulcerative colitis is characterized by erosions and ulcers on the mucous membranes of the large intestine. It is this type of disease that is most often diagnosed by doctors, and not only in childhood.
Chronic colitis develops in a child if its acute form is not treated in time.
Whatever form of illness the baby suffers from, it is very important to diagnose it in time and begin treatment, the success of which depends on how accurately the recommendations of the attending physician are followed.
Treatment
Ulcerative colitis
Colitis in children three years of age and older can be treated largely through changes in diet and general routine.
It is important to make the child feel better and reduce the frequency of seizures. For this, a diet is prescribed that excludes dairy products and is rich in meat, fish, and eggs.
Babies under one year old who are artificially fed are transferred to hypoallergenic lactose-free formulas.
A diet to cure colitis in older children requires, during moments of exacerbation, to completely exclude all foods that interfere with the food processing process, negatively affect the mucous membrane and increase gas formation.
“Prohibited” foods include flour delicacies, crackers and chips, salty and spicy foods, fast-food, carbonated sweet water, sauces and seasonings, preservatives, coffee, chocolate. It is also better to refuse or minimally reduce the amount of legumes, raw fruits and berries, fatty meats, yeast, rice and corn in the diet.
It is advisable to build a daily menu for colitis in a child. It should include soups based on boiled meat and vegetables, lean meat stews), porridge (buckwheat, pearl barley, rolled oats are recommended). Flour is not completely prohibited. Allowed are hard pasta, white bread made from rye flour, and bran rolls. Drinks made from herbs, tea, and jelly will be useful.
Painkillers, laxatives or restorative drugs help relieve some of the symptoms. Antiviral and antibacterial substances, glucocorticoids, and antipyretics are also used. In very severe forms that cannot be treated with medication, resection is performed - amputation of a fragment of the intestine.
We must not forget about preventive measures, which include regular (once a year) medical examination. About drug therapy, proper nutrition, constant stable physical activity.
Diagnostics
Nonspecific ulcerative colitis of the intestine, who has had it?
A pediatric gastroenterologist knows how to treat colitis in children and diagnose it, based on information obtained during a physical examination, laboratory and instrumental procedures.
Thus, the first stage of diagnosing pathology is aimed at:
- familiarizing the clinician with the medical history of not only the patient, but also his relatives - to identify the etiological factor that is most suitable for a particular person;
- collection and study of the child’s life history – this should include information regarding the course of the period of intrauterine development of the fetus;
- a thorough examination, involving palpation of the anterior wall of the abdominal cavity - to establish its location, which will indicate the affected part of the large intestine;
- a detailed survey of the patient or his parents is necessary to determine the intensity of clinical manifestations, which, in turn, will provide information about the severity of the inflammatory process.
The following laboratory tests are considered the most valuable:
- general and biochemical blood test;
- coprogram;
- bacterial culture of feces;
- analysis of stool for dysbacteriosis.
The last step of diagnostic manipulations is instrumental procedures, among which it is worth highlighting:
- colonoscopy and rectoscopy;
- endoscopic biopsy of the affected segment;
- X-ray of the intestine using a contrast agent;
- Ultrasound of the peritoneum;
- CT and MRI.
Colitis in children should be differentiated from:
Prevention
It is almost impossible to prevent nonspecific ulcerative colitis due to the reasons that cause it are not fully understood. During the course of the disease, during the period of remission, every effort must be made to follow all the instructions of the attending physician so that it lasts longer.
To avoid relapse, it is necessary to protect the child from stress and shock, unnecessary stress, provide high-quality, proper nutrition, and protect against intestinal infections. It is better for schoolchildren to study at home. Vaccination is carried out for such children only in agreement with an immunologist. Children with an established diagnosis of UC should be registered at a dispensary and regularly undergo the necessary examinations.
We recommend: What is pseudomembranous colitis: how it manifests itself and treatment methods
Description of the disease
Chronic atonic colitis treatment
Childhood colitis is an inflammation of the colon, accompanied by intense cutting pain with functional disorders of the intestine. More than 10% of cases of colitis develop from infancy. Therefore, the main problem of pediatric gastroenterology is the diagnosis and treatment of inflammation of the colon.
Since in children in the first years of life the digestive system has some structural features, inflammation affects two sections of the intestine. This disease is called enterocolitis. In adolescence, isolated lesions of different parts of the intestine, classified as enteritis and colitis, are more common. Consequently, the inflammatory process can be limited and widespread, that is, covering several areas.
When the distal part of the intestine is affected, proctitis develops, and when the rectum and S-shaped intestine are inflamed, proctosigmonditis develops. The illness happens:
- acute and chronic;
- infectious and non-infectious;
- ulcerative and spastic.
Infectious colitis is a dysenteric disorder. Frequent exacerbations of the protracted form lead to delayed physical development and psychosocial adaptation.
Common methods of treating childhood colitis:
- Anti-inflammatory therapy using high-frequency electromagnetic fields, healing methods with electromagnetic waves of the decimeter range, therapeutic mud of various origins.
- Anesthetic therapy by prescribing electrophoresis with novocaine.
- Prescription of antispasmodics taken during sessions of high-frequency magnetic therapy, electrophoresis, applications with coolants, sitz baths.
- Specific methods, including endonasal electrophoresis with B vitamins, exposure of the intestines to direct electric current at low voltage (up to 80 V), current irradiation with a frequency of 50-100 Hz, drinking mineral waters, prescribing microenemas, colon hydrotherapy.
- Treatment with sedatives, including the effects of current pulses on the brain, electrophoresis with bromine on the neck-collar area, pine baths.
Diet therapy is one of the main techniques for relieving the disease. Young patients are assigned to table menu No. 4, in which dairy products are excluded, and the dishes are enriched with proteins from fish, meat, and eggs.
To normalize microflora, probiotics are prescribed
At the same time, antibiotics are prescribed: Sulfasalazine, Mexaform, Erythromycin, Enteroseptol. The list of medications includes analgesics, anticholinergic drugs, ganglion receptor blockers, such as Novocaine, Atropine, etc. To maintain normal intestinal microflora, the following are taken:
- enzymes;
- antihistamines;
- probiotics;
- enveloping, adsorbent and astringent agents;
- vitamins of group B, PP, A.
Traditional methods of treatment are represented by a number of recipes:
- decoction of alder cones, taken orally for 4 months;
- cleaning with microenemas with chamomile or St. John's wort for 1 month;
- microenemas at night with sea buckthorn oil in the amount of 60 g - for teenagers, 30 g - in the first years of life;
- flaxseed tinctures;
- cleaning with enemas on mumiyo with a dilution of 0.05-0.1 g of the substance - for adolescents, 0.02 g - from 3 months to 1 year.
Before using any of the above methods, you must consult your doctor.
Treatment of the disease
Treatment of this disease usually occurs over a fairly long period; in this case, an integrated approach, which involves following a diet, is very important. A small patient should exclude dairy products, meat, fish and eggs from the diet.
Next, the doctor usually prescribes the following medications:
- Antibiotics (Enteroseptol). Antibiotics are usually taken three times a day for a week.
- Enzymes (Mexase). Enzymes are taken for two weeks.
- Probiotics (Bifikol). Taking probiotics usually coincides with a course of antibiotics.
- Analgesics (Novocaine).
- Antihistamines (Zodak, Zyrtec, Suprastin).
- Vitamin complexes.
Suprastin
In addition, the course of taking medications can be combined with traditional methods of treatment . Your doctor may recommend taking flax seed tincture or doing microenemas at night with rosehip decoction.
Physiotherapeutic procedures, for example, dry heat, a heating pad, paraffin therapy and ozokerite, help well with colitis.
Diagnosis and treatment of colitis
For an infant, colitis can cause the development of other diseases, for example, peritonitis. If you do not see a doctor in time, the symptoms become more severe and it is more difficult to determine an accurate diagnosis.
The purpose of diagnostic measures is to confirm or refute the presence of colitis and determine its type. To do this, the following procedures are carried out:
- General examination and palpation of the abdomen;
- Fecal analysis (the structure, presence of blood, mucus, traces of parasites are studied);
- Blood test (the main indicators are the level of red blood cells, leukocytes and hemoglobin);
- X-ray of the intestines (prescribed only in controversial cases).
Since colitis is a very dangerous disease, especially for children under one year of age, treatment should take place exclusively in a hospital setting. For quick and effective rescue, complex therapy is prescribed, which includes the following measures:
- A course of antibiotics. The drug and dose depend on the age of the child and the stage of the disease. In addition, the antibiotic is selected after determining the exact pathogen.
- Special diet. If the baby is completely breastfed, then the mother should avoid aggressive foods and products that can cause allergies. For artificial nutrition, it is also worth choosing a mixture that is hypoallergenic and easily digestible. After six months, the baby can be given liquid low-fat soups, ground porridge, chicken broth. But it is necessary to exclude fresh vegetables and fruits for a while.
- Dysbacteriosis may develop against the background of colitis. Therefore, for prevention purposes, probiotics and sorbents are prescribed. For this age category, Laktiale and Smecta are considered the safest.
- Anti-inflammatory and painkillers of non-steroidal origin. Often used in the form of droppers. This method is considered more effective and safe.
Treatment requires calm and patience. During this period, you should not let your baby try new foods, so as not to cause an aggravation. Also, do not panic, if a child refuses food, it means that his damaged intestines are not yet ready.
For prevention purposes, doctors recommend eliminating all allergenic foods from the diet. Also, try each new food in small portions.
Particular attention should be paid to the baby’s hygiene and behavior. For example, if your child puts everything in his mouth, then you need to ensure the cleanliness of all his toys and things that surround him
You should not let your child play with keys, money, telephones and other things that are often found in public places.
Alternative medicine also has several methods in its arsenal. First of all, various decoctions based on honey and propolis are used to treat colitis. But these products can cause severe allergies. Therefore, doctors do not recommend resorting to such methods when treating children under one year of age. In such cases, you need to be careful in choosing a treatment method, because we are talking about the child’s health.
What causes colitis in newborns?
Colitis is an intestinal disease that is dystrophic-inflammatory in nature. This is a very complex disease, and for young children it is also very dangerous. Often, due to untimely or improper treatment, colitis becomes chronic and suffers with its unpleasant manifestations for a long time.
This disease is diagnosed in 15% of newborns under one year of age. Boys are at risk, this is due to their special hormonal structure. In total, there are four types of colitis; in infants, allergic colitis occurs in most cases.
Colitis has many causes, but specifically in infants under one year of age it occurs as a result of the following factors:
- Bacterial and viral damage to the intestines. This happens due to the entry of harmful organisms into the digestive organs through the mouth or nose. Very often this is observed when eating, especially when it comes to low-quality complementary foods. Children also often experience helminthiasis and other parasitic infections.
- Failure to comply with hygiene and baby care rules. This includes dirty hands and dirty food. You can get an infection even if you do not follow the rules of breast care during feeding.
- Stress and severe nervous tension. Many parents believe that at this age their child understands little. But, in fact, the baby feels and experiences everything. He is especially affected by the emotional state of the mother. Colitis can result from such childhood experiences.
- Allergic reaction to a food product. This is one of the main reasons for the development of the disease.
- Failure to follow the baby's nutritional rules. Up to one year old, children should eat soft food 5-6 times a day and possibly even at night. Products must be appropriate for the age category. Therefore, non-compliance with the regime, food that is not yet able to be digested in the children's intestines, can cause colitis and gastritis.
- Hereditary factor. He plays his role 70% of the time.
Typical case
Ulcerative colitis occurs according to a single pattern. The medical history of such patients has similar points. Let us describe the general version of the pathology using a specific example.
Medical history of a patient with ulcerative colitis:
Patient M., 9.5 years old, was admitted to the gastroenterology department with complaints of diarrhea, bleeding in feces, bloating, pain in the left abdominal wall. The attack began more than 3 weeks ago; outpatient treatment with antibacterial agents was performed, which did not produce positive results. According to his mother, the boy recently suffered from rotavirus infection.
In a hospital setting, the patient underwent colonoscopy, FGDS, and ultrasound of the abdominal cavity. Ulcers, infiltration of the membrane with leukocytes, and single polyps were found in the intestines. Histology conclusion: morphological picture of UC. The process affected the rectum area, changes were found in the sigmoid colon, in the left parts of the colon. After a course of treatment, the symptoms subsided. The patient was sent home under the dispensary observation of a local pediatrician and gastroenterologist.
This story shows that:
- in childhood, boys are more likely to get sick;
- the average age of patients is 7-10 years;
- colitis in children is not limited to the rectum;
- an attack of the disease is often associated with a viral infection.
Nonspecific ulcerative colitis in children symptoms
NON-SPECIFIC ULCERATIVE COLITIS IN CHILDREN AND ADOLESCENTS
The article examines the features of the course of nonspecific ulcerative colitis (UC) in children of different age groups, evaluates the significance and information content of generally accepted X-ray endoscopic and histological criteria for diagnosing UC, and conducts a comparative analysis of the effectiveness of therapy with aminosalicylates and prednisolone. It is noted that ulcerative colitis in children is characterized by total damage to the colon and a chronic continuous course. The most informative symptoms are diarrhea with bloody discharge, abdominal pain, and weight loss. Each age group has its own characteristics of the course of the disease, but in children under 7 years of age they are most pronounced. Despite total lesions, these patients have minimal symptoms. Diarrhea, weight loss, and blood loss may be absent. The only manifestations of UC may be abdominal pain and unstable stool. Diagnosis of ulcerative colitis should be based on clinical and anamnestic data, the results of endoscopic and histological studies. Endoscopic signs of UC were detected in 80% of patients, and histological signs - in 65%. It has been established that the age of patients, the severity of exacerbation and the dose of the drug affect the results of therapy. The developed algorithm for the treatment of ulcerative colitis in children makes it possible to effectively achieve remission of the disease and prevent the development of life-threatening complications.
Edition: Russian Pediatric Journal Year of publication: 2002 Volume: 3 pp. Additional information: 2002.-N 2.-P.16-18
Symptoms
The main symptom of UC is loose, foul-smelling stools with a frequency of up to 20 times a day.
Manifestations of the disease depend on the form and course, the severity of colitis, and the age of the children. The most characteristic symptoms of UC are diarrhea, blood in the stool, and abdominal pain.
The onset of the disease can be gradual or acute, sudden. Almost every second child develops UC gradually. In most cases, the stool is loose and foul-smelling, with the presence of mucus, blood (sometimes also pus). The frequency of stool varies - from 4 to 20 or more times per day, depending on the severity.
With a mild degree of colitis, there are streaks of blood in the stool; with severe colitis, there is a significant admixture of blood; the stool may look like a liquid bloody mass. Bloody diarrhea is accompanied by pain in the lower abdomen (more on the left) or in the navel area. Characterized by tenesmus (painful act of defecation), increased bowel movements at night.
The pain can spread throughout the entire abdomen. They can be cramp-like in nature, precede bowel movements or accompany them. Some children experience pain when eating.
Sometimes UC begins with the appearance of loose, loose stools, and blood and mucus are found in the stool after 2-3 months. With severe ulcerative colitis, body temperature rises within 38 ° C, and symptoms of intoxication appear. Sometimes a child is mistakenly diagnosed with dysentery. Exacerbations of the disease are regarded as chronic dysentery, and UC is diagnosed late.
Children with UC experience decreased appetite, severe weakness, bloating, anemia, and weight loss. On examination, rumbling is noted, and a painful, spasmodic sigmoid colon is palpable. The liver is enlarged in almost all children, and sometimes there is an enlargement of the spleen. In rare cases, constipation occurs with this disease. As the illness continues, abdominal pain occurs less frequently. Persistent pain syndrome is observed in complicated UC.
Symptoms and treatment of intestinal inflammation in a child
Inflammatory bowel disease refers to inflammation of the mucous membrane in the intestines. Almost all parents of small children face this problem. What are the symptoms of this pathology and how to relieve inflammation - read below.
Intestinal inflammation in a child can be chronic and is characterized by immune inflammation of the intestinal walls.
Among childhood pathologies of the digestive system, intestinal inflammation is in first place. It is believed that the most severe gastrointestinal diseases are Crohn's disease and ulcerative colitis. Children are susceptible to ulcerative colitis more often than adults. Moreover, the reasons for the appearance of this disease are still not entirely clear. Most often, intestinal inflammation is associated with dietary errors and viral infections.
Symptoms of intestinal inflammation in a child
For nonspecific ulcerative colitis. Already at the age of three to five months, a child may develop symptoms of this disease. The main one is the inclusion of blood in the baby’s stool with the subsequent occurrence of diarrhea. In adult children, diarrhea may occur immediately. The chronic form of ulcerative colitis is characterized by frequent loose stools and painful cramps;
For Crohn's disease. Inflammation of the intestines in Crohn's disease is manifested by ulcerative formations on the intestinal walls. Ulcers can develop into fistulas. The first period of the disease is characterized by narrowing of the intestines. The child suffers from frequent bowel movements—up to ten times a day—and abdominal pain after eating. During the last period of the disease, blood appears in the stool;
Treatment of intestinal inflammation in children
Intestinal inflammation in children should be treated in the direction of restoring the structure of the mucous membrane of the intestinal walls. Treatment must be comprehensive. This includes diet therapy and the use of medications.
The child's meals should be frequent and small. Foods that irritate the intestinal mucosa - chewing gum, chocolate, coffee, fatty and spicy foods - should be excluded from the children's diet. Young children are given soy-based formulas.
When intestinal inflammation occurs, medicinal drugs are used - such as Sulfosalazine, Pentas, Salofalk, which contain 5-aminosalicylic acid, which helps reduce inflammatory processes.
There are cases when the inflammation is so severe that surgery is required. To avoid this, you need to contact a specialist with your child at the first symptoms of Crohn’s disease or ulcerative colitis.
MOST INTERESTING NEWS
Forecast
With timely detection and the prescription of the necessary course of procedures, complete rehabilitation of acute childhood colitis is possible. The permanent form of the disease in this case goes into a long stage of remission.
Modern therapeutic methods show effectiveness in 85% of cases of cure of patients with mild and moderate ulcerative colitis up to complete remission.
Colitis is an inflammatory disease of the large intestine that affects the epithelial layer of the mucous membrane. In the case of a prolonged pathological process, dystrophy of the intestinal mucosa occurs with its thinning.
Why does colitis occur and how does it progress?
There is no exact answer to why colitis occurs in children due to the characteristics of each child’s body and social differences. When favorable conditions arise, colitis develops, sometimes due to a combination of factors and the appearance of an infectious agent.
Various provoking factors can contribute to the development of colitis:
- hereditary predisposition;
- stress and emotional excitability;
- food poisoning;
- long-term drug treatment;
- immunity deficiency;
- autoimmune diseases;
- helminthic infestations;
- defect of the digestive system or underdevelopment;
- past infectious diseases.
In infants, colitis occurs with inflammation of the small intestine due to anatomical features. In older children, colitis is an isolated inflammation of the large intestine. Symptoms in children are severe from the first days of the disease. Colitis most often develops in children after suffering from an intestinal disease.
The main causative agents of colitis:
- staphylococci;
- coli;
- streptococcus;
- Mycobacterium tuberculosis;
- viruses.
Classification of colitis
Colitis can be classified according to dystrophic changes in the intestines:
- atrophic;
- catarrhal;
- erosive-ulcerative.
Inflammation can occur isolated in one place or in several, therefore colitis is distinguished:
- Typhlitis. Inflammation of a limited nature of the cecum.
- Typhlocolitis. Inflammation of the large and ascending intestines.
- Transversit. Colitis, characterized by inflammation of the transverse colon.
- Sigmoiditis. Inflammation of the sigmoid intestine.
- Angulite. Inflammation of the area of the intestine located between the descending and transverse colon.
- Proctitis. Inflammation of the rectum.
- Simple sigmoiditis. Inflammation of the sigmoid and rectum.
- Pacocolite. Generalized intestinal inflammation.
Symptoms in a child
The disease begins suddenly and acutely with severe intoxication of the child’s body.
The disease is accompanied by the following complaints from the child:
- nausea;
- vomit;
- weakness;
- abdominal pain;
- frequent stool.
Colitis is characterized by hyperthermia, nausea, and vomiting. Due to intestinal spasms, the child experiences pain and tenesmus localized in the iliac region. The frequency of stool reaches up to 15 times a day. The stool becomes greenish in color with mucus or streaks of blood. If an adult's stool has turned green, you can find out the reasons here.
Infants may experience rectal prolapse; symptoms of dehydration are severe: lethargy, dry mucous membranes and a decrease in the amount of urine and frequency of urination.
Chronic colitis has a wave-like nature, that is, remission of the disease is replaced by relapses. During relapses, symptoms of acute colitis appear.
Stool disorder in children with chronic colitis is expressed by alternating constipation with diarrhea. The feces have the appearance of undigested food, “sheep” or ribbon-like feces. Children often suffer from rectal fissures due to the passage of hard feces.
Psychovegetative disorders may appear in children with chronic colitis:
- headache;
- weight loss;
- weakness;
- sleep disturbance;
- irritability.
Causes of colitis in children
Colitis appears in children for the following reasons:
- intestinal infection;
- allergy;
- eating disorder;
- food poisoning;
- unfavorable state of residence;
- antibacterial therapy;
- stress;
- helminths;
- heredity;
- dysbiosis.
Diagnostics
It is very important to differentiate colitis from other diseases with similar symptoms. After all, treatment tactics and the outcome of the disease depend on the diagnosis.
List of diseases for differential diagnosis:
- Crohn's disease;
- hemorrhagic vasculitis;
- intestinal infection;
- helminths;
- shigellosis;
- abdominal form of tuberculosis;
- appendicitis syndrome;
- tumors and polyps of the colon;
- celiac disease.
Necessary laboratory and instrumental studies:
- general blood analysis;
- blood chemistry;
- stool analysis;
- X-ray of the intestine;
- intestinal endoscopy;
- biopsy of material.
Treatment of colitis
A therapeutic diet is necessary for patients with acute forms of colitis, and is also recommended for its chronic forms. The diet helps reduce the inflammatory process in the intestines as a result of reducing the processes of fermentation and rotting of food in the digestive system.
Diet No. 4
Table No. 4 implies limiting the intake of fats and carbohydrates in the diet and using a gentle regime for the intestines to avoid irritation of the digestive organs. The recommended energy value of the diet should be no more than 2050 kcal.
Diet features:
| Nutrient elements | Quantity |
| Fats | 70 gr. |
| Squirrels | 100 gr. |
| Carbohydrates | 250 gr. |
| Free liquid | 1500 l. |
Indications for prescribing the diet:
- inflammatory bowel diseases.
- dysentery;
- gastroenteritis;
- colitis;
- gastritis.
Diet principles:
- The treatment table should be high in protein.
- In case of diarrhea, food is consumed in crushed and pureed form. What food to choose for diarrhea, read here.
- The frequency of meals is 6 times a day, warm.
- All products must be boiled.
- The duration of the diet is no more than 7 days.
- Mandatory carbohydrate restriction.
- Eating cold and hot foods is prohibited.
- You can't overeat.
What is possible and what is not?
Recommended Products:
- low-fat fish;
- dairy products with fat content less than 2.5%;
- dishes made from chicken eggs in the form of an omelet;
- pasta and vermicelli;
- lean meat;
- weak tea, jelly and compotes;
- butter;
- decoctions of buckwheat and rice groats.
Prohibited products:
- cereals;
- sauces;
- lemonades and any sweet drinks;
- vegetables;
- fruits;
- bread;
- flour products;
- canned food;
- seasonings and spices.
Approximate menu for the day
Approximate daily diet menu for a child:
- Breakfast: a glass of rosehip decoction, 150 gr. egg white omelette. A couple of crackers.
- 2nd breakfast: 100 gr. cottage cheese.
- Lunch: 100 gr. liquid soup with shredded chicken breast, 100 gr. noodles with boiled cutlet. A glass of blueberry jelly.
- Afternoon snack: with a takana of boiled rice.
- Dinner: 200 gr. vermicelli with boiled fish. A glass of weak tea.
- 2nd dinner: with 1% kefir, crackers.
Diet depending on the type of colitis
Colitis may occur with constipation or diarrhea. Depending on the nature of the stool disorder, the list of prohibited foods may change.
List of prohibited foods for colitis with constipation:
- rich soups;
- fatty meat and mushrooms;
- pasta;
- semolina;
- fresh bread;
- chocolate, strong tea;
- spicy seasonings.
List of prohibited foods for colitis with diarrhea:
- legumes;
- milk;
- vegetables and side dishes made from them;
- sugar;
- candies, cookies.
Nutrition for nonspecific and ulcerative colitis
For these types of colitis, it is necessary to follow several recommendations that can speed up the recovery process:
- It is recommended to have light dinner no later than 20.00.
- Products consumed by the patient must be fortified with calcium and potassium.
- Liquid intake should be limited.
- It is necessary to eat in small portions, but often every 3 hours.
- The diet should include foods containing proteins up to 150 grams.
- Food should be eaten warm.
- You only need to steam or boil foods.
List of prohibited products:
- carrot;
- cabbage;
- greenery;
- radish;
- fruits;
- smoked products;
- legumes;
- juices;
- semi-finished products;
- chocolate.
Nutrition for spastic colitis
This type of colitis requires strict abstinence from sweets.
In addition, it is necessary to increase the amount of fiber-rich foods consumed, so the basis of the diet is the following foods:
- vegetables;
- bran bread;
- legumes;
- fruits.
In the absence of pain, cereals and juices diluted with water are allowed. In case of relapse, these products are prohibited from consumption.
List of prohibited products:
- fatty meats;
- oil;
- dairy products;
- cheeses with a high percentage of fat.
Diet for colitis during exacerbation
During the period of exacerbation of colitis, it is recommended to drink tea and rosehip decoction. It is necessary to exclude sweet foods and juices from the diet. From the 2nd day, the table can be expanded, and permitted foods are allowed to be consumed. All products must be boiled.
Recommended Products:
- slimy porridge;
- wheat crackers;
- decoctions of rosehip and quince;
- soups with weak broth;
- weak tea.
Nutrition for colitis in remission
During the period of remission, a large number of foods are allowed, only cooking involves: boiling, stewing, baking.
List of permitted products:
- porridges and cereals, with the exception of pearl barley and millet;
- dairy products;
- eggs in the form of an omelet;
- vegetables only stewed or baked;
- fruits are best consumed baked;
- dried bread;
- tea and coffee with milk;
- lean meats and semi-finished products;
- jelly and compotes;
- fresh cucumbers and tomatoes.
Rehabilitation after treatment
After recovery and in the remission stage of colitis, it is recommended to undergo a rehabilitation course.
Rehabilitation includes:
- treatment in a sanatorium;
- Exercise therapy, massage and breathing exercises;
- taking a course of probiotics and enzymes.
Forecast
With timely diagnosis and treatment, the prognosis is favorable. The disease can go into a stage of stable remission. With frequent relapses of the disease, the physical development of the child and their social development in society suffers.
Complications
With untimely treatment and late consultation with a doctor, the risk of developing the following complications increases:
- perforation of the ulcer;
- intestinal obstruction;
- peritonitis;
- sepsis;
- vascular thrombosis;
- necrosis of intestinal tissue;
- fistulas;
- haemorrhoids;
- sphincter weakness.
Prevention
For primary prevention of the disease, the following recommendations must be followed:
- proper nutrition;
- sanitation of foci of infection;
- timely treatment of infectious diseases;
- compliance with personal hygiene rules;
- instilling proper eating habits;
- exemption from physical activity at school.
For secondary prevention of colitis, it is recommended to adhere to the following recommendations:
- clinical examination;
- drug therapy once every 2 years.
Colitis in a child is an intestinal disease accompanied by inflammatory-dystrophic changes in the organ. In newborns and babies under one year of age, it is diagnosed as enterocolitis, since the inflammatory process simultaneously affects the large and small intestines. In schoolchildren, the pathology affects the organ in isolation, causing its different segments to suffer, and doctors make two diagnoses - colitis and enteritis.
Why do children get colitis?
Intestinal tract disease in children develops for various reasons. The most common provoking factors are:
- stress;
- intestinal infections;
- influence of radiation;
- heredity;
- helminthic infestations;
- violation of nutrition rules;
- autoimmune disorders;
- aggravated course of allergies;
- intolerance to certain foods;
- underdevelopment of the digestive organs;
- frequent treatment with antibacterial drugs;
- living in an unfavorable ecological environment.
In infants, colitis is associated with intestinal dysfunction of an unclear nature.
Clinical features of colitis
The pathological process in the large intestine in children can be widespread and limited to one/several segments. Based on these features, colitis is divided into such varieties as:
- proctitis (rectum);
- typhlitis (damage to the cecum);
- typhlocolitis (blind and ascending parts);
- transversite (transverse colon segment);
- sigmoiditis (sigmoid colon);
- proctosigmoiditis (straight and sigmoid sections);
- pancolitis (generalized inflammation);
- angulitis (junction of the transverse colon with the descending colon).
According to the nature of the course, colitis is acute and chronic, and according to severity - mild, moderate and severe. Based on morphological and endoscopic data, the type of disease is determined as catarrhal, ulcerative, atrophic. According to the type of course, the pathology is classified as monotonous, recurrent, latent and progressive colitis.
Taking into account the etiology, colitis is divided into secondary, nutritional, radiation, infectious, neurotic, parasitic. There are also medicinal and toxic forms and the “colitis of unknown nature” type.
The main clinical forms diagnosed in young patients are acute and chronic colitis, spastic colitis, ulcerative nonspecific colitis.
How to recognize colitis
Acute colitis caused by infections occurs with all the signs of toxicosis:
- vomit;
- weakness;
- sudden weight loss;
- temperature increase.
Pain from intestinal spasm radiates to the ileal region. During bowel movements, rectal prolapse is sometimes observed.
Symptoms of pathology are easy to recognize by stool - it comes out watery and foamy, has a greenish color, bloody streaks or mucous inclusions. The frequency of the urge to defecate increases from 4 to 5 times to 15 trips to the toilet in one day.
Other symptoms of infectious colitis are dry mucous membranes, decreased skin turgor, and pointed facial features.
With a prolonged course, colitis is manifested by stool disorders: both constipation or diarrhea, and alternating abnormalities. Defecation becomes more frequent up to 7 p.m. per day. Stools are produced of different nature and consistency:
- liquid masses;
- "sheep balls";
- ribbon-like thick masses;
- defecation products with mucous inclusions or remnants of undigested food.
In case of constipation with subsequent passage of hard feces, the symptoms are complemented by red blood in the stool, leaked due to a fissure in the anus. Chronically current colitis causes rumbling in the intestines, bloating and increased gas formation. Psychovegetative disorders in children include headache, weakness, irritability, and sleep problems. Colitis affects the health of an infant by anemia, retarded growth and weight gain, and hypovitaminosis.
In the spastic form of colitis, the symptoms of the disease will be as follows:
- weakness;
- abdominal pain and bloating;
- temperature increase;
- disturbance of stool with the release of mucus, blood, foam;
- excessive dryness of the skin and drying out of the mucous membranes.
Diagnostic measures for colitis
An accurate diagnosis is made based on an external examination of a sick child by a gastroenterologist and data from examinations performed. Valuable information about the condition of the intestines during colitis can be obtained by such types of studies as:
- sigmoidoscopy;
- irrigography;
- colonoscopy;
- rectoscopy;
- endoscopic biopsy;
- barium passage radiography;
- blood test showing decreased levels of electrolytes and red cells, hypoalbuminemia;
- stool scatology to identify leukocytes, amilorrhea, steatorrhea, creatorrhoea;
- analysis of defecation products for dysbacteriosis and its bacteriological examination.
Prolonged colitis requires differentiation from intestinal dyskinesia, diverticulitis, cystic fibrosis, Crohn's disease, celiac disease, enteritis, and latent appendicitis.
How to improve bowel function
Treatment of colitis requires an integrated approach. Children are transferred to the Pevzner diet (table No. 4), the principles of which include a complete abstinence from dairy foods and a predominance of protein products in the diet. To strengthen the immune system, newborns are given rosehip decoctions. Artificial animals are fed pureed food, steamed or boiled. Dishes are not salted. Children are given broths that are not rich, fish and cottage cheese are not fatty. It is useful for older children to eat berry jelly made from cherries and blueberries (the dessert has astringent properties).
Drug treatment consists of several groups of drugs:
- antihistamines – Suprastin, Fenistil, Diazolin;
- enzymes – Digestal, Mexaza, Abomin;
- antibiotics – Sulfasalazine, Mexaform, Erythromycin;
- probiotics – Bifikol, Intestopan, Bifidumbacterin, Colibacterin;
- analgesics, ganglion blockers, anticholinergics - Metacin, Novocaine, Platyfillin;
- vitamin complexes with substances of groups B, A, PP.
Physiotherapy is indicated for exacerbation of colitis. Dry heat and a heating pad are applied to the child's epigastric zone. In the remission stage, treatment is supported by diathermy, paraffin therapy, and ozokerite.
Often these measures are enough to improve intestinal functions. But if the conservative approach does not produce lasting results, Dr. Komarovsky suggests performing surgery on the child. Its essence consists in excision of the problem segment and fusion of the iliac and rectal sections.
Our specialist comments
- Remember that any form of colitis is dangerous due to chronicity of the process, inflammation of the peritoneum and intestinal perforation. In turn, these pathologies cause anemia, exhaustion of the body and endocrine disruption.
- Among the folk remedies, it is recommended that children suffering from colitis be given a decoction of alder cones for a long time (only 4 months).
- Microclysters with sea buckthorn oil are given to 2-year-old children in the amount of 25 g of the substance; for adolescents, 60 g of oil is administered one time.
The doctor explains why the child has a stomach ache and what needs to be done
Colitis is a disease of the colon that occurs with inflammatory changes. There are many causes and symptoms for this diagnosis. This condition can be life-threatening, especially for a child. Therefore, its timely detection and timely treatment are necessary measures.
This disease occurs in children in 10% of cases among pathologies at an early age. It often becomes a chronic process, especially if parents hope for its independent resolution. As a rule, colitis appears much more often in boys. This is explained by the peculiarities of hormonal levels.
Treatment and prevention
Treatment of colitis in children under three years of age and older is carried out to a large extent by normalizing the diet and diet. To alleviate the child’s condition and reduce the intensity of symptoms, a dairy-free diet enriched with meat, fish, and eggs is prescribed. Artificial children up to one year old are transferred to lactose-free hypoallergenic milk formula.
In the case of breastfed children, identifying the etiology of the disease is of great importance, since some cases of allergic colitis require an urgent transfer of the child to artificial nutrition or a strict diet for the nursing mother.
From the diet of older children during periods of exacerbation, it is necessary to exclude all foods that complicate the digestion process, corrode the walls of the mucous membrane, and contribute to increased gas formation.
Such products include flour sweets, chips, crackers, salty and spicy crackers, all fast food, sweet carbonated drinks, mayonnaise, ketchup, store-bought and homemade pickles and preserves, cocoa, coffee, chocolate. It is necessary to minimize the consumption of legumes, raw fruits and berries (apples, grapes, plums, peaches, bananas, currants, raspberries, etc.), fatty meats, yeast baked goods, corn and rice cereals.
The basis of the menu should be soups based on boiled vegetables and meat, stewed and boiled beef, rabbit, chicken, turkey, porridge (especially oatmeal, buckwheat, pearl barley). For flour products, you can eat hard pasta, rye and slightly dried white bread, and bran buns. Herbal drinks, jelly, black and green teas are useful.
Drug treatment for colitis involves taking oral medications that improve digestion, protect and restore the intestinal mucosa. Local therapy in the form of therapeutic enemas helps well. Taking painkillers, laxatives or restoratives, antiviral and antibacterial drugs, glucocorticoids, and antipyretics will help relieve symptoms. In the most severe cases, which are not amenable to conservative therapy, resection is performed - removal of a section of the intestine.
Preventive measures include annual medical examination with mandatory drug treatment, maintaining proper nutrition, and moderate physical activity.
Causes
If we talk about acute colitis, it usually develops after an intestinal infection. This disease can also appear after illnesses such as:
- gastroenteritis;
- acute gastritis;
- enteritis.
However, pathology can also occur against the background of other reasons. The most common factors for its manifestation include the following:
- heredity;
- food poisoning;
- stressful situations;
- intestinal dysfunction in newborns;
- long-term medication use;
- weakened immune system;
- eating disorder;
- autoimmune diseases;
- environmental pollution;
- worms.
As we see, colitis in children can develop against the background of various signs. This disease is similar to such a specific diagnosis as Crohn's disease. Only an experienced doctor can distinguish them. Despite the similar symptoms and causes, the treatment of these two diseases is different.
Classification of the disease
Changes in the colon during colitis can be multiple or limited, the latter, as a rule, having one or more lesions. Therefore, the following classification is introduced:
- typhlitis - inflammation of the cecum, limited;
- typhlocolitis - the ascending and large intestine are inflamed;
- transversitis - inflammation of the transverse colon;
- sigmoiditis - inflammation of the sigmoid colon;
- angulitis - the transition between the descending and transverse colon is inflamed;
- proctitis - inflammation of the rectum;
- simple sigmoiditis - the sigmoid and rectum are simultaneously inflamed;
- pancolitis is a generalized inflammation.
Colitis in children can be nutritional, toxic, infectious, radiation, secondary, neurotic. Also, colitis can vary based on the state of the level of motor skills in children; they can be with a predominance of diarrhea or constipation.
Colitis is divided into atrophic, catarrhal, erosive-ulcerative, according to its nature it is divided into chronic and acute, according to the type of course of the disease, colitis is divided into: progressive, monotonous, latent, recurrent. The most common forms of colitis are: acute, chronic, ulcerative, spastic.
Infectious acute colitis occurs with severe toxicosis, elevated temperature, vomiting, weakness, and anorexia. Due to regular spasms, the child will complain of pain and increased bowel movements up to 15 times a day. The stool itself will have a foamy, watery appearance with a greenish tint, and may contain mucus and blood. During defecation, rectal prolapse may occur, as with hemorrhoids.
Chronic colitis occurs in children with a variable course, periods of exacerbation alternate with relief and even remission. The disease manifests itself through pain in the navel and iliac region, and stool disturbance also occurs. Pain occurs after eating and during bowel movements.
Stool disorders can be expressed in both diarrhea and constipation, which can even lead to the appearance of cracks in the anus. Children suffering from chronic colitis complain of severe bloating and rumbling in the abdomen, flatulence, weakness, irritability, headache and sleep problems may appear.
Why do children get UC?
UC is a pathology similar in development and clinical picture to Crohn's disease. It is distinguished from other IBD by alternating stages of remission and exacerbation.
It is not known for certain why children of different ages suffer from CT pathology, but behind the scenes gastroenterologists are inclined to genetic predisposition as the main risk factor.
External factors play an important role. Colitis is associated with external agents, which, when entering the gastrointestinal tract, provoke inflammation in the colon.
The prevalence of UC is in the range of 41-116 cases per 100 thousand people. A high mortality rate is observed if the symptoms of ulcerative colitis in children appear in a pronounced form, and the disease proceeds with lightning speed. In such scenarios, malignant neoplasms form in the intestines within a year.
Symptoms of pseudomembranous colitis
In mild forms of this disease, the presence of diarrhea due to medication is noted. Within 7-10 days, as a result of treatment with antibiotics, a severe form of clostridial colitis may develop. In this case, the first sign will be liquid diarrhea. All this has a negative effect on water and electrolyte metabolism in the body and causes tachycardia, general fatigue, and decreased tone of all muscles.
- dizziness;
- nausea;
- thirst;
- rapid pulse;
- fainting;
- rare urination;
- dry skin.
In very severe cases, bleeding from the rectum is observed. Diarrhea and dehydration have an intoxicating effect, the symptoms of which are:
- weakness;
- headache;
- pain in the abdominal area;
- poor appetite, refusal to eat;
- body temperature is above 38°.
Most often, the patient experiences pain before defecation, and the process of bowel movement itself is difficult. Palpation of the colon causes painful and unpleasant sensations, the abdomen is swollen.
A symptom of the development of complications of pseudomembranous and clostridial colitis is intestinal perforation, as well as its increase in size. This can be caused by constipation, which has a toxic effect on the body. With intestinal perforation, very severe headaches are observed, the abdominal muscles are tense and painful. In addition, fluid appears in the abdominal cavity, which further aggravates the general condition of the patient. To improve the condition, it is necessary to select the necessary treatment regimen for pseudomembranous colitis.
Development of membranous colitis
- renal failure;
- malignant formations;
- operations performed in the abdominal area;
- chronic inflammatory bowel condition;
- taking cytostatic drugs;
- Crohn's disease;
- long-term stay near infectious patients;
- installation of the probe.
Pseudomembranous colitis in children
In the first year of life, a child is most vulnerable, so cases of the spread of the Clostridium difficile microbe are not uncommon. Children also suffer from atresia of the membranous type. To treat obstruction, membrane excision is used.
Another well-known method, but more traumatic, is the treatment of membranous obstruction of the duodenum using bypass anastomoses.
The occurrence of pseudomembranous colitis at this age occurs much less frequently, even despite prolonged use of antibiotic drugs.
Prolonged hospital stay to take antibiotics contributes to the development of pseudomembranous colitis. Most often, this disease affects newborns with Hirschsprung's disease, children with a lack of leukocytes in the blood, as well as infants with chronic inflammatory processes - colitis or Crohn's disease.
Typically, pseudomembranous colitis in a child begins as mild colitis and is not severe. A feature of the disease is the absence of symptoms of intoxication of the body, diarrhea predominates. If left untreated, it can lead to life-threatening dehydration. Complications of pseudomembranous colitis may be accompanied by heavy bleeding, the development of sepsis and intestinal perforation.
Diagnosis of pseudomembranous colitis
Computed tomography will reveal pathological changes in the intestines. Using a colonoscopy, a specialist will diagnose the intestinal walls and take a biopsy for analysis.
Treatment regimen for pseudomembranous colitis
The main goal of treating pseudomembranous colitis is to eliminate the symptoms of inflammation.
For diarrhea, you must follow a fasting diet. The treatment regimen should be as follows:
- Drinking large amounts of liquid - herbal infusions or just water, if tea, then unsweetened;
- After the diarrhea subsides, you can take cottage cheese, kefir;
- You need to eat frequent and small portions;
- Eat bananas, rice, baked potatoes, as these foods significantly reduce diarrhea;
- Eliminate fried and spicy foods from your diet, so you need to stick to the right diet.
Bacterial therapy is also used for treatment, which has a bactericidal effect on the fecal flora and eliminates the symptoms of the disease.
In severe forms of pseudomembranous colitis - perforation, perforation or expansion of the walls of the colon - surgical intervention is necessary. In this case, the affected part is removed. After this operation, the patient’s condition stabilizes and the chances of recovery increase significantly.
Complications
Long-term UC can lead to local and systemic complications.
Local complications include:
- Lesions in the anus and rectum:
- haemorrhoids;
- sphincter failure (incontinence of gases and feces);
- fistulas;
- cracks;
- abscesses.
- Perforation of the intestine and subsequent development of peritonitis (inflammation of the serous membrane of the abdominal cavity).
- Intestinal bleeding.
- Stricture (narrowed lumen) of the colon due to scarring of ulcers.
- Acute toxic dilatation (expansion) of the large intestine.
- Colon cancer.
In children, local complications develop in rare cases. The most common cause of any form of ulcerative colitis is dysbiosis (imbalance of beneficial microflora in the intestine).
Extraintestinal, or systemic, complications are diverse:
- skin lesions (pyoderma, erysipelas, trophic ulcers, erythema nodosum);
- damage to the mucous membranes (aphthous stomatitis);
- hepatitis (inflammation of liver tissue) and sclerosing cholangitis (inflammation of the bile ducts);
- pancreatitis (inflammatory process in the pancreas);
- arthritis (joint inflammation, arthralgia (joint pain));
- pneumonia (pneumonia);
- eye damage (episcleritis, uveitis - inflammation of the membranes of the eye);
When examining a child, you can identify manifestations of hypovitaminosis and chronic intoxication:
- pale skin with a grayish tint;
- blue circles near the eyes;
- dull hair;
- jams;
- dry, cracked lips;
- brittle nails.
Increased heart rate and arrhythmias are also noted, a heart murmur may be heard, and shortness of breath often occurs. With active hepatitis, yellowness of the skin and mucous membranes appears. The child lags behind not only in physical but also in sexual development. In teenage girls in the active phase of the disease, the menstrual cycle may be disrupted (secondary amenorrhea occurs).
In the chronic process, erythropoiesis (production of red blood cells) is inhibited, which, in addition to bleeding, contributes to the development of anemia.
After 8-10 years from the onset of the disease, the risk of a malignant tumor in the rectum increases by 0.5-1% annually.