Causes and symptoms
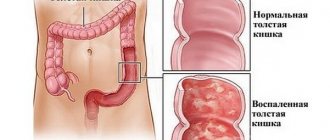
Any intestinal pathology inevitably affects digestive function. In addition, they are characterized by pain and deterioration of the general condition. The presence of colitis can be determined by the following symptoms.
Main signs of the disease:
- Digestive disorders: constipation, vomiting or diarrhea.
- Increased gas formation.
- Pain in the abdominal area, which subsides after bowel movement.
- General intoxication of the body, weakness, drowsiness and a feeling of constant fatigue.
- Attacks of insomnia, anxiety and sudden mood swings.
- Bad breath, belching and bitter taste.
Symptoms appear very quickly and in many ways can be confused with food poisoning. The temperature may rise, fever and chills may appear. In addition, with a progressive disease, impurities of mucus and blood in the stool are often observed.
Many negative factors can lead to the development of catarrhal colitis of the intestine. First of all, these are nutritional errors, because eating too fatty, spicy and other “heavy” foods can lead to such problems. In addition, catarrhal colitis is often diagnosed after previous infections, infection with parasites and the activity of staphylococcal and streptococcal infections.
Possible causes of colitis:
- Strict diet.
- Weakening of the immune system.
- Intestinal dysbiosis.
- Taking medications for a long time.
- Chronic constipation.
- Parasitic infestations.
- Exacerbation of chronic diseases.
- Intestinal injuries and burns.
- Food poisoning.
The peak of diseases occurs in the summer months, when fresh fruits and vegetables predominate in the diet. In addition to the fact that they cannot always be thoroughly washed and a lot of pathogenic flora enters the body, the process of breakdown of plant fiber is often accompanied by fermentation and accumulation of putrefactive bacteria. All this creates ideal conditions for inflammatory processes of various etiologies, and therefore leads to the formation of colitis.
Treatment
It is carried out on an outpatient basis (in a clinic with the patient receiving recommendations for therapy at home) or in a hospital (if there is a threat to health and life, unfavorable dynamics of the general condition, in case of infection - if it is impossible to isolate the patient). The goal is to eliminate inflammatory foci, prevent complications, and in the acute form, transition to the chronic stage.
Diet for acute form
How to treat a patient? In case of infection, the consequence of which is inflammation of the intestines, it is recommended to limit the amount of food load. When appetite appears, the following are allowed:
- slimy soups;
- white stale bread;
- crackers;
- dry unsweetened cookies;
- porridge without oil;
- weak meat broths without pepper;
- baked peeled apples;
- pureed lean meat;
- boiled lean fish;
- steam omelette without seasonings.
The return to the usual menu should be gradual, after 3-4 weeks of the diet.
In this case, prohibited foods and drinks should be:
- Milk.
- Seasonings.
- Fatty meats and fish.
- Smoked meats, pickles, canned food.
- Garlic, marinades.
- Fresh fruits and vegetables, herbs.
- Carbonated drinks.
- Coffee, hot chocolate.
- Alcohol.
- Packaged juices.
It should be taken into account that the healing process, even after high-quality therapy, takes several weeks, and functional disorders of the intestines may persist for 1-3 months. Therefore, milk and refractory fats must be introduced into the diet with care, and if you are intolerant, it is better to abandon them altogether.
Diet for chronic form
The same foods are prohibited as for acute colitis. During the period of relapse (resumption of symptoms), the nutritional regimen already described in the section above is used. After entering the remission stage (improvement of condition, absence of complaints), the diet should be balanced - it includes:
- porridge;
- lean meat and fish;
- fruits and vegetables;
- according to tolerance, taking into account the impairment of lactose absorption - fermented milk products.
You need to stick to the diet constantly, even if treatment is completed, since the intestinal mucosa can respond to an inappropriate product by exacerbating the inflammatory process. In this regard, the diet should be planned so that it covers energy costs during the day.
Drug therapy
Treatment of intestinal catarrhal colitis in acute form can be carried out using drugs such as:
- Antispasmodics (“Mebeverine”).
- Antibiotics (Nifuroxazide, Intetrix).
- Sorbents (“Enterosgel”).
- Antidiarrheals (“Smecta”).
- Enzymes (“Pancreatin”).
- Probiotics (Linex).
- Means for relieving flatulence (Espumizan).
- Detoxifiers (“Sodium chloride solution 0.9%”).
Therapeutic measures for the chronic form include, depending on the cause of inflammation and the individual characteristics of the disease:
- probiotics (“Bifidumbacterin”, “Yoghurt”);
- antispasmodics (“Drotaverine”);
- laxatives (“Mukofalk”, “Tissasen”);
- prokinetics (“Domrid”);
- anti-inflammatory (“Salofalk”);
- defoamers (Simethicone).
If you have catarrhal colitis, you should not take antimicrobial drugs on your own. Such treatment can lead to adverse consequences - in particular, to antibiotic-associated diarrhea and the development of a pseudomembranous form of inflammation of the colon.
Other methods
For chronic colitis, your doctor may recommend physical therapy:
- Applications of mud, ozokerite.
- Inductothermy, electrophoresis.
- Microclysters from mineral water.
- Warm baths.
- UHF therapy.
- Microwave.
The course of therapy is usually carried out in a sanatorium-resort environment, and an institution is selected that specializes in pathologies of the digestive organs and intestines in particular.
Mineral waters may also be useful (not during an exacerbation). These are “Essentuki No. 17”, “Batalinskaya” for those with a tendency to constipation, and “Berezovskaya” for patients with diarrhea.
Forms of catarrhal colitis
Despite the variety of causes leading to the development of the disease, it is customary to distinguish only two forms of catarrhal colitis: acute and chronic. Diagnostics includes a survey and examination of the patient, as well as special laboratory and instrumental examinations.
How to determine colitis:
- A blood test in case of this disease shows leukocytosis, increased ESR, decreased red blood cell count and hemoglobin level.
- A general stool analysis shows the presence of mucus and bloody discharge. In addition, you can detect undigested fiber, an increased number of white blood cells and the causative agent of the disease itself.
- An endoscopy will help confirm or refute problems with the digestive system.
- Fluoroscopy and irrigoscopy are special examinations using a contrast agent. Helps identify possible intestinal dysfunctions.
- Anoscopy and colonoscopy are instrumental methods for examining parts of the intestine. They are very informative for any diseases of this organ; they allow you not only to see possible causes, but also to take a biopsy of damaged tissue.
Examinations using special equipment will allow you to assess the extent of damage and the rate of progression of the disease. In addition, this will help to exclude other possible intestinal diseases, and, if necessary, take material for biochemical analysis.
Causes of the disease
Common causes that could provoke catarrhal colitis:
- infectious infection, viruses;
- parasitic and helminthic infestation;
- toxins and toxic substances that enter the body with food or drugs;
- severe stress, neurosis;
- dyspepsia;
- medicines.
Quite often, catarrhal colitis develops in humans due to decreased immunity. A weakened immune system is unable to resist pathogenic factors that affect the mucous membrane of the digestive system, so inflammatory processes begin.
An exacerbation of the disease is observed in the summer, when people eat more raw fruits and vegetables. Sometimes the body cannot cope with complex fiber, which comes in large quantities, which leads to a malfunction of the digestive system. Stagnation of food mass in the intestines leads to its rotting and fermentation.
Features of the development of acute catarrhal colitis
Catarrhal colitis of the intestine in the acute stage will certainly “remind” itself of a sharp deterioration in well-being, pain in the abdominal area on palpation and digestive disorders. Tachycardia, surges in blood pressure, sweating and increased body temperature are less common. In these cases, it is imperative to call an ambulance and undergo the necessary examinations. Such symptoms are characteristic of many diseases, so only a specialist can determine the exact etiology of the disease. With insufficient or untimely treatment, acute colitis quickly turns into a chronic form, and this is a diagnosis “for life.”
Types of colitis
Erosive intestinal colitis treatment
Depending on the nature of the manifestation of symptoms, catarrhal type colitis can be moderate or severe.
If we are talking about a moderate course of the disease, then symptoms can appear at different times and with any intensity. There also come periods when the signs fade away for a while.
The severe form of colitis is characterized by sharp and painful sensations, which include nausea and malaise. At the same time, gas formation increases, and the urge to have frequent bowel movements appears.
The disease has a pronounced symptomatic picture of an infectious type. In this case, its course is complicated by pathogenic bacteria that have managed to enter the intestines.
Moderately severe colitis can be ischemic or ulcerative. Symptoms include painful spasms of a pulling nature. Appetite is lost, diarrhea appears, mucous and blood impurities can be found in the stool.
If such a disease is detected late, it can become chronic. It is difficult to determine what it is until a lot of mucus begins to appear in the stool. With such a symptom, we are already talking about chronic colitis, and it comes in several types:
- Distal. Characterized by significant tone of the descending intestinal tract.
- Spastic. Promotes even greater tone of the intestinal walls, stimulates the formation of frequent spasms.
- Hypertensive. Causes hypertonicity of the colon; inside the body, the lumen becomes uneven and narrow. It is easy to identify a disease of the hypertensive type. It is detected by the slow movement of feces, which are mixed with purulent mucus.
The last type of chronic colitis is typical for people who abuse flour products and sweets. It is also common for those who have suffered from dysbacteriosis or an intestinal infection.
Chronic colitis: symptoms and types
The development of chronic colitis is most often preceded by its acute forms. The course of the disease is less pronounced, sluggish and asymptomatic. The most common type is focal catarrhal colitis, which is also classified into three types.
Types of focal colitis:
- Spastic colitis - due to increased tone of the intestinal walls, they spasm.
- Distal colitis - hypertonicity of the descending and sigmoid sections is formed.
- Hypertensive colitis is a narrowed intestinal lumen and hypertonicity of all parts of the colon.
Depending on the type and extent of the lesion, the necessary treatment is determined. It should be noted that chronic forms of colitis are less treatable and can often cause periodic problems throughout life. It is very difficult to completely get rid of the disease.
Causes
Catarrhal colitis of the intestine most often develops with infections:
- Shigellosis (dysentery).
- Salmonellosis.
- Escherichiosis.
- Campylobacteriosis.
Sometimes there is damage to the mucous membrane of the colon as a result of the influence of staphylococci, Proteus, clostridia, and Klebsiella.
The cause of the inflammatory process may also be:
- consumption of poor quality food;
- exposure to ionizing radiation;
- enzyme deficiency;
- disaccharidase deficiency;
- impaired immune status;
- chemical poisoning;
- trauma to the mucous membrane (for example, as a result of colonoscopy).
Colitis can be combined with enteritis (damage to the colon) and gastritis (inflammatory process in the stomach). This pathological process can transform (for example, the appearance of ulcers, purulent foci).
Treatment of catarrhal colitis
The chosen treatment plan must take into account the individual characteristics of the patient and the degree of development of the disease. The nature of the origin of this disease can be different, so the first step is to eliminate the provoking factors. Suitable drug therapy is prescribed by a doctor, treatment varies in duration. During the treatment period, it is imperative to adhere to a strict diet, give up bad habits and follow all doctor’s instructions.
Approximate treatment plan:
- Taking medications that restore normal microflora.
- Elimination of muscle spasm of smooth muscles.
- The use of special enzyme preparations that facilitate the digestion process.
- Medicines that have a positive effect on digestive functions. If the patient has diarrhea, it is necessary to use astringents; for chronic constipation, a mild laxative is used.
- Taking antibiotics is necessary if pathogens act as a provoking factor. The choice of appropriate drugs is made by the doctor based on clinical tests.
- Removal of intoxication of the body is carried out with special preparations and plenty of drinking.
Throughout the entire treatment period, it is very important to provide the patient with complete rest. It is necessary to avoid physical activity and psychological stress. Typically, chronic catarrhal colitis is treated in a hospital until acute symptoms are relieved, after which the patient continues the selected methods of therapy at home. It should be noted that for successful treatment it is necessary to strictly adhere to the diet and doctor’s instructions, otherwise there is a high risk of relapse of the disease.
Symptoms
Nonspecific ulcerative colitis of the intestine, who has had it?
Colitis can occur in acute or chronic form. A constantly existing inflammatory process occurs if, during the bright period of primary manifestations, the patient did not receive treatment or did not complete a full course of therapy, there are factors that aggravate the condition and repair (restoration) of tissues: additional infection, trauma, intoxication, allergies, immunodeficiency.
Acute form
With inflammatory damage to the large intestine, you can observe the following symptoms of catarrhal colitis:
- Abdominal pain, mainly in the lower regions on the left side.
- Tenesmus is a false urge to stool.
- Liquid feces mixed with mucus and blood, sometimes “green”, “swamp mud”.
- Painful bowel movements, often without a feeling of relief.
Feces in colitis, as a rule, are not abundant - but this is only true for isolated damage to the colon; when combined with enteritis, obvious diarrhea with a significant volume of liquid feces is observed. The smell of the discharge is unpleasant and pungent. Pain in the abdominal area has a constant or wave-like character - it periodically increases and subsides, intensifies with palpation and pressure on the abdominal wall.
Chronic form
It is characterized by a violation of the motor and secretory function of the colon, and can occur with a predominance of constipation or diarrhea, or with their alternation. Chronic catarrhal colitis is manifested by the following symptoms:
- absence of independent stool for 2-7 days, recurring occasionally;
- liquid feces mixed with blood and mucus;
- bloating, flatulence;
- tenesmus (false urge to defecate);
- abdominal pain of the colic type, spastic, cramping.
Sometimes there is an imperative urge to defecate - such a strong desire to empty the intestines that the patient is unable to suppress it. Abdominal pain may intensify when visiting the toilet, physical activity, or shaking. It has a bright, sharp character (if caused by a spasm) or dull, aching, monotonous, colicky (with flatulence).
Additional signs
In addition to typical symptoms, the inflammatory process is also characterized by extraintestinal symptoms:
- Weakness.
- Fast fatiguability.
- Decreased performance.
- Deterioration of sleep.
- Weight loss.
- Poor appetite.
- Headache.
- Depressed mood.
If colitis is combined with other types of damage to the gastrointestinal tract, symptomatic manifestations such as:
- nausea;
- vomit;
- fever;
- profuse diarrhea;
- heaviness in the epigastrium;
- fever.
Dyspeptic syndrome is also present, symptoms of which include nausea, belching, bitterness and an unpleasant taste in the mouth. Anorectal lesions are characterized by redness and swelling of the mucous membrane in the area around the anus.
Folk remedies for the treatment of catarrhal colitis
The use of traditional treatment recipes gives a good positive effect. To do this, you must consult your doctor and strictly follow the dosage and frequency of taking the chosen remedy.
Treatment of colitis with folk remedies:
- Decoctions of oak bark, chamomile and St. John's wort can be used for enemas. These herbs have wound healing and regenerative properties, and also remove the inflammatory process in tissues.
- If you are not allergic to bee products, you can use the following recipe. Dissolve a teaspoon of fresh honey in a glass of warm water. Drink the resulting solution three times a day half an hour before meals. The course of treatment is a month, after which a break is taken.
- Another vital product of bees, bee bread, is also very useful. For a therapeutic effect, you need to eat half a teaspoon three times a day.
- Homemade jelly from dogwood, blueberry or viburnum greatly promotes intestinal healing. The lights have an enveloping effect and promote the regeneration of mucosal cells.
- Microenemas with potato juice. To do this, freshly prepared juice is diluted with boiled water exactly in half and an enema is given with this solution. The method is effective, because starch helps heal wounds and relieves inflammation. The course of procedures is at least ten; before each microenema, the intestines should be cleansed.
Such treatment cannot replace drug therapy, but will perfectly complement it. Before use, you must ensure that there is no allergic reaction to the components of the mixture. Consultation with your doctor before using this or that composition is also required.
Diagnosis of the disease
To confirm the diagnosis of catarrhal colitis, a number of procedures are necessary. A general analysis of blood, urine and feces should confirm the presence of inflammation in the body. Biochemical studies can determine the degree of damage to the digestive organs. Instrumental procedures are necessary to visualize the changes occurring in the mucous membranes.
Diagnostic stages:
- blood test for leukocytosis;
- general analysis of stool;
- colonoscopy;
- endoscopy;
- fluoroscopy;
- anoscopy;
- irrigoscopy.
Nutrition
A special diet is important in the treatment of colitis. The effectiveness of the measures taken, as well as the duration of the medication course, will depend on proper nutrition. It is necessary to exclude from the diet all fresh and canned fruits and vegetables, as well as foods that irritate the intestines and stimulate increased gas formation. In addition, the following rules should be adhered to.
Organization of a diet for colitis:
- The daily diet should be divided into five to six servings.
- Food should be at a warm temperature, neither hot nor cold.
- During an attack of acute colitis, it is necessary to avoid eating altogether, but drink actively to avoid intoxication of the body.
- Food should be ground to a puree consistency.
- It is preferable to steam or bake foods. Boiling is also an option, but fried and smoked foods should be excluded from the diet. In addition, you should not eat foods that are too hot, spicy or fatty.
In addition to diet, it is advisable to carry out sanatorium treatment of the digestive organs at least once a year. If you have the opportunity to purchase such a ticket, this will be an excellent opportunity to forget about such an illness forever.
Common symptoms and signs of the disease
Colitis is usually accompanied by abdominal pain and bloody or watery diarrhea. Other symptoms:
- blood in stool;
- nausea;
- tenesmus: painful and convulsive urge to defecate;
- spasms and pain in the lower abdomen, often appearing in waves;
- weight loss;
- headache;
- nausea or vomiting;
- muscle pain;
- dehydration;
- high fever, chills and other signs of infection and inflammation.
Infectious colitis is accompanied by bloody diarrhea, nausea, vomiting, stomach cramps and fever. Ischemia, or lack of blood supply to the intestines, causes severe pain, fever, and bloody diarrhea. The main signs of microscopic colitis are watery diarrhea, abdominal pain, mucus in the stool and weight loss.
Disease prevention
Symptoms of catarrhal colitis most often appear as a result of poor nutrition and poor personal hygiene. It is very important to properly process food, especially those consumed fresh. A healthy lifestyle and proper nutrition will help strengthen the body from the inside and also strengthen the immune system. In addition, you should give up bad habits, and also exclude “quick” dry snacks. Regular visits to the doctor are also a good way to prevent intestinal diseases, especially for previously diagnosed problems.
Intestinal diseases manifest themselves very quickly and require mandatory hospital treatment. One of the most common diseases of this organ is colitis. Our article will tell you how to recognize the disease, as well as how to treat catarrhal colitis.
Symptoms
In order to recognize the inflammation that has begun inside in time, you need to know the symptoms of catarrhal colitis. These include the following violations:
- gas formation increases, the stomach swells;
- pain occurs in the lower abdominal cavity, reminiscent of cramping spasms;
- a person begins to get tired faster;
- weakness during the day is felt throughout the body, appetite disappears;
- blood clots and mucus can be found in the stool;
- the appearance of causeless irritability;
- sleep is disturbed, the person is bothered by insomnia;
- there is a bitterness and/or unpleasant odor in the mouth;
- body temperature rises significantly;
- constipation gives way to diarrhea.
All these signs indicate that inflammation has already begun in the large intestine. This means that the next step should be an accurate diagnosis of the sick person’s condition and comprehensive treatment.
As mentioned above, the inflammatory process promotes swelling of the walls of the colon, stimulating its increase in size. Because of this, the lumen of the organ narrows significantly, further provoking the formation of painful cracks. Inflammation gradually covers not only individual parts of the intestine, but also its entire surface.
The severity of symptoms depends on how the inflammation spreads. With focal colitis, the general condition will not be critical. But diffuse catarrhal colitis affects every part of the intestine, so the symptoms are extensive.
Symptoms of the disease
Diffuse intestinal colitis most often affects both parts at once and is severe. Since colitis affects both the large and small intestines, symptoms become apparent from the very first day. The symptoms include both signs of gastritis and signs of enteritis.
The symptoms of the disease have been well studied. Endoscopy shows total damage to the left side of the large intestine. Patients complain of stool disorders. Some are bothered by constant diarrhea, others, on the contrary, suffer from constipation, while others note that they have unstable stools (alternating constipation and diarrhea).
In some cases, diffuse intestinal colitis is accompanied by pain, the localization of which is difficult to determine independently. This occurs because the inflammatory process affects different parts of the colon. Pain is not always present, it occurs periodically, most often in the afternoon after the main meal, and is cramp-like in nature. Patients report a feeling of severe abdominal distension.
Pain is almost always combined with tenesmus - a false urge to defecate in the complete absence of feces. They are accompanied by the passage of gas and small lumps of feces. The following symptoms add to the clinical picture:
- Flatulence.
- Dyspeptic disorders.
- Symptom of insufficient emptying.
- Constant rumbling in the stomach.
- Belching.
- Sensation of bitterness in the mouth.
Patients have pale skin, their tongue is coated with a pale gray coating, and there is a constant unpleasant odor coming from their mouth. On palpation, pain is noted along the entire length of the intestine.
The described clinical picture can be taken as a description of another disease - enteritis, but, unlike it, diffuse colitis is accompanied by psychovegetative disorders. Over time, the patient develops severe dizziness, weakness, general malaise, the person loses a lot of weight, and develops anemia.
The psychological status also changes. There is a feeling of anxiety, a tendency to irritability, irritability, sleep disturbance. Typically, chronic diffuse colitis lasts a long time, characteristic symptoms appear only in the stages of exacerbation, during remission the disease becomes sluggish, but atrophic changes in the intestinal walls continue to progress. And this is the most dangerous complication.
During the period of exacerbation, patients experience an unpleasant taste in the mouth, a decrease and sometimes loss of appetite, diffuse pain along the colon is noted, which periodically intensifies, acquiring the character of colic, and is sometimes accompanied by reflex phenomena from the heart: palpitations, less often pain. Usually, during an exacerbation, stools become more frequent up to 3-5 times a day, and with more severe damage to the distal parts of the intestine, false, painful urges to lower down are possible. The bowel movements often have a “cow-like” appearance; before defecation, the pain intensifies and often ends with an imperative urge to defecate. Sometimes the pain continues for some time (1-2 hours) after defecation.
In some cases, loose stools soon after eating are accompanied by belching, nausea, and sometimes vomiting. In other cases, the urge to defecate and the release of liquid, foul-smelling feces appear 6-7 hours after eating, when the bulk of food debris enters the large intestine, sometimes this is observed early in the morning (5-6 hours) - “alarm clock diarrhea.”
Causes
The development of catarrhal colitis is most likely in a certain risk group:
- people with weakened immune systems;
- those who constantly or frequently and for a long time experience stress;
- those whose body is depleted of vitamins and minerals;
- those who often suffer from dysbiosis, intestinal disorders - constipation or diarrhea.
Doctors include the following as the main reasons for the development of catarrhal colitis:
- intestinal infections caused by Escherichia coli, streptococci, staphylococci;
- activity of parasites, helminths;
- stress of neurotic origin;
- disturbances in the digestive process that begin in the stomach;
- taking strong medications, especially antibiotics, for a long period;
- toxins of various types.
A connection has been established between the occurrence of catarrhal colitis and the summer season. During this period, the consumption of vegetables and fruits, especially raw, increases. In case of digestive disorders or a significant amount of food eaten, fermentation processes occur in the intestines, possibly putrefactive, which ultimately leads to inflammation of the organ mucosa and even ulceration of its walls.