What is peptic ulcer of the stomach and duodenum?
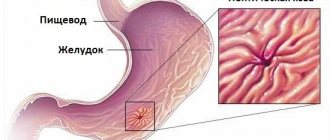
A set of substances that are peptic aggressors regularly enters the stomach cavity: hydrochloric acid, enzymes. Their action is aimed at breaking down food products. To prevent these substances from damaging the wall of the stomach or duodenum, the stomach produces a special protective factor, which consists of mucus and bicarbonates.
- The predominance of aggressive factors in combination with the depletion of the protective layer leads to damage to the stomach wall.
- Erosion appears, and then an ulcer.
- The acidic contents of the stomach enter the duodenum.
- Inflammation occurs - duodenitis; erosions and ulcers can also develop in its mucosa.
- Of particular importance in the development of the problem is the microbe Helicobacter pylori, which aggravates and provokes damage to the mucous membrane of both the stomach and duodenum.
The chronic nature of the pathology involves alternating exacerbations and remissions. Exacerbations occur against the background of physical and mental overload, diet violations, and bad habits. Peptic ulcer disease most often affects men. The working age of the main group of patients with gastric ulcers indicates the social and economic significance of the problem.
Operations for perforation of an ulcer
A perforated stomach ulcer is an emergency condition. If the operation is delayed, it can lead to the development of peritonitis and the death of the patient.
Usually, when an ulcer is perforated, it is sutured and the abdominal cavity is sanitized, and less often, an emergency gastrectomy is performed.
Preparation for emergency surgery is minimal. The intervention itself is performed under general anesthesia. Access – upper median laparotomy. A revision (examination) of the abdominal cavity is performed, a perforation hole is located (it is usually several millimeters), and it is sutured with absorbable thread. Sometimes, for better reliability, a large oil seal is sewn to the hole.
Next, the stomach contents and effusion that have entered there are sucked out from the abdominal cavity, and the cavity is washed with antiseptics. Drainage is being improved. A tube is inserted into the stomach to suction out the contents. The wound is sutured layer by layer.
The patient is on parenteral nutrition for several days. Broad-spectrum antibiotics are mandatory.
If the course is favorable, the drainage is removed on the 3-4th day, the sutures are usually removed on the 7th day. Working capacity is restored after 1-2 months.
When peritonitis develops, repeated surgery is sometimes required.
Suturing a perforated ulcer is not a radical operation, it is only an emergency measure to save life. The ulcer may recur. In the future, it is necessary to undergo regular examinations for early detection of exacerbations and the appointment of conservative therapy.
Causes of stomach ulcers
There are etiological factors of the disease and risk factors that increase the likelihood of ulcers. Among the causes of peptic ulcer disease are the following:
- presence of the bacterium Helicobacter pylori in the body,
- decreased local immunity in the stomach,
- burdened heredity,
- imbalance between the protective factors of the gastric mucosa and its secretion,
- taking certain medications.
Among the drugs that destroy the gastric mucosa, non-steroidal anti-inflammatory drugs (NSAIDs) should be highlighted. Long-term treatment with their help, without proper protection of the mucous membrane, leads to the occurrence of ulcers and bleeding from them.
Causes of callous ulcers
In most cases, gastric ulcers can be completely cured, but in some cases they can become chronic and in this case are called callous ulcers. Most often, ulcers are formed as a result of thinning of the mucous membrane or its complete absence; as a result, hydrochloric acid has direct contact with the walls of the stomach, corroding them, which causes the formation of an ulcer.
In more detail, hydrochloric acid, due to weak mucous membrane or its absence, begins to destroy the cell membrane, which mainly consists of phospholipids with elements of various proteins. And the acid emulsifies fat molecules, while cell proteins coagulate. Proteolytic enzymes also promote the breakdown of protein into its component parts.
After the mucous cells are destroyed, the submucosal cells are destroyed next in line, which begins proliferation processes with a local character, since hydrochloric acid has an aggressive effect only on a certain area in the stomach.
Australian research shows that one of the most common causes of ulcers is Helicobacter pylori infection. This bacterium causes ulcers in almost 40% of all cases worldwide. Previously, it was commonly thought that no microorganisms could survive in hydrochloric acid, but this bacterium is able to weaken the effects of hydrochloric acid by secreting special enzymes, which in turn produce ammonia.
Because of this, the mucous membrane is destroyed and the walls of the stomach become more vulnerable. The bacterium also destroys the walls of the stomach itself, so that nothing at all prevents the appearance of an ulcer. It is quite difficult to detect these bacteria, the same goes for eliminating them, since they have extreme resistance to various adverse effects, not to mention their favorite habitat in the stomach, which in itself is certain death for most other pathogenic bacteria.
Other causes include glucocorticoids and some other anti-inflammatory drugs, especially those that are non-steroidal. Each of the groups reduces the production of prostaglandins, which in turn does not allow the mucous membrane to recover, and some even directly destroy it. One of the well-known such drugs is aspirin.
Not so long ago, stress situations began to be considered in medicine as the cause of the formation of acute ulcers. Since peripheral spasm may occur during a shock situation, metabolic processes slow down noticeably and cells may die.
An ulcer can also appear as a result of diseases of the glands of the endocrine system, but to date this area of the issue has not been sufficiently studied, so this cannot be stated unequivocally.
Symptoms of peptic ulcer disease in the presence of an ulcer
- Symptoms of the disease usually appear quite clearly, which makes it possible to promptly identify the disease and begin appropriate treatment. The main symptom is pain
, depending on the nature of the pain, you can understand where exactly the ulcer is localized. The timing of pain is also important. Peptic ulcers with localized ulcers in the stomach are characterized by so-called “hunger pains” that appear on an empty stomach, as well as several hours after eating.
- If the cardiac part of the stomach is affected (it is adjacent to the esophagus), then pain occurs closer to the solar plexus 20 minutes after eating. Often the pain extends to the chest in the area of the heart, which can be confusing and cause a misdiagnosis such as a heart attack when trying to self-diagnose. Such localization of a peptic ulcer is never accompanied by pain after physical activity.
- Ulcer damage to the pyloric part of the stomach (closer to the duodenum) causes prolonged acute pain, manifested in attacks. Sometimes the duration of one attack can be more than 40 minutes. The pain develops an hour after eating. May occur at night. Dyspeptic symptoms often occur: nausea, feeling of bloating, vomiting. The ulcer of this localization is 5-10% malignant. Complications such as penetration, perforation, bleeding, and pyloric stenosis due to cicatricial deformation are also common.
- 10-15% of ulcers are localized in the antrum, located between the pyloric and cardiac. Moreover, if the defective formation is located in the lesser curvature of the stomach, the patient will feel severe pain in the left hypochondrium 1-1.5 hours after eating. Stabilization of the condition occurs after the contents of the stomach are digested. Most of these patients experience pain in the evening.
- An ulcer localized in the greater curvature of the stomach is characterized by a less pronounced clinical picture; it occurs less frequently, more often in the elderly, and in 50% of cases it is malignant, and such an ulcer is quite difficult to detect.
- Continuous aching pain, experienced mainly in the evening and at night, may indicate the location of a defective formation in the antrum. In this case, the pain syndrome does not correlate with food intake.
- The nature of pain with a duodenal ulcer is characterized by the fact that it appears 1.5-2 hours after eating, often at night. This location of the ulcer is more common in men under 40 years of age. The genetic factor is more significant for this category of patients. Dyspeptic disorders are less common than when localized in the stomach, but quite often patients are bothered by constipation.
Features of patient selection for surgical treatment of peptic ulcer
In emergency situations (perforation, bleeding), the question is about the life and death of the patient, and here there is usually no doubt about the choice of treatment.
When it comes to planned resection, the decision must be very balanced and thoughtful. If there is even the slightest opportunity to manage the patient conservatively, this opportunity should be used. The operation can get rid of the ulcer forever, but it adds other problems (quite often manifestations occur, designated as operated stomach syndrome).
The patient should be informed as much as possible about both the consequences of the operation and the consequences of not taking surgical measures.
Other signs of a stomach ulcer
In addition to pain, the following signs may also indicate the presence of a peptic ulcer:
- Nausea,
sometimes accompanied by vomiting. This occurs due to impaired gastric motility. If there is an ulcer, vomiting may begin 2 hours after eating. - Heartburn
. Most patients suffer from this symptom, which manifests itself as a burning sensation in the epigastric region. With heartburn, the acidic contents of the stomach end up in the lumen of the esophagus, which is accompanied by a rather unpleasant sensation. - Feeling of heaviness in the stomach
. It is observed after eating, regardless of the amount eaten. - Poor appetite.
The symptom is associated with the fear of heartburn and vomiting, which torment the patient after eating. This is a psychological factor that explains the deterioration of appetite by the patient’s desire to avoid unpleasant sensations. - Belching of air
can also be accompanied by the reflux of stomach contents into the oral cavity, after which an unpleasant sourish or bitterish taste remains in the mouth. - Increased gas formation
.
Patients often complain of constipation caused by intestinal dysfunction. Atypical symptoms include a white coating on the tongue, sweaty palms, and pain when pressing on the abdomen. Sometimes the ulcer does not manifest itself with any symptoms, in which case it can be found in a rather advanced state.
Medical educational literature
Clinically, callous ulcer is manifested by a long course of the disease. The pain becomes more persistent and intense. They occur after eating not only spicy food, but also food that is slightly irritating to the mucous membrane, and do not disappear after vomiting.
Radiologically, such an ulcer is characterized by larger niche dimensions than with a normal ulcer, and most importantly, a higher marginal shaft. During dynamic observation of such an ulcer, persistent constancy of radiological signs is noted. Such ulcers are usually localized in the subcardial and antral parts of the stomach.
Callous ulcers are dangerous due to their degeneration into a malignant tumor. During gastroduodenoscopy, it is often difficult to determine the nature of pathomorphological changes in tissues. Therefore, a biopsy is necessary to clarify the diagnosis.
Conservative treatment for callous ulcers is not indicated.
Penetration of an ulcer is a slowly, gradually and gradually developing destruction of the wall of the stomach or duodenum, ending with a complete violation of its integrity with the transition of the inflammatory process to neighboring organs, which cover the defect in the wall of the stomach or duodenum. Most often, ulcers located on the back wall of the stomach or duodenum penetrate. Typically, the ulcer penetrates into the pancreas, hepatoduodenal ligament, hepatogastric ligament, lesser omentum and liver.
With a penetrating ulcer, the patient's general condition is more severe. Clinical signs characteristic of perivisceritis and encysted perforation are revealed: intense, often constant pain and increased body temperature. The pain characteristic of the ulcerative process is layered with pain characteristic of the organ involved in the pathological process. Often these pains dominate over ulcerative pain. The blood test shows an increase in ESR, leukocytosis with a neutrophilic shift in the formula appears.
An X-ray examination reveals a large ulcerative niche, consisting of three layers - barium, liquid and gas, around which an infiltrate is detected. Noteworthy is the pronounced hypersecretion of the stomach with a violation of its motor function.
Penetrating ulcers require surgical treatment.
Degeneration of an ulcer into cancer (malignization). Stomach ulcers usually develop into cancer. Ulcers of the greater curvature and prepyloric part of the stomach are especially unfavorable in this regard. The literature describes only isolated cases of duodenal ulcers degenerating into cancer.
Callous ulcers in patients over 40 years of age are susceptible to malignancy. An ulcer greater than 1.5 cm in diameter should be considered potentially malignant.
The criterion for the transition of an ulcer to cancer should be a set of signs that make the assumption of a malignant process more likely. S.S. Yudin emphasized that the larger the ulcer, the deeper the niche, the older the patient, the lower the acidity of gastric juice, the more likely the possibility of such an ulcer degenerating into cancer. An important indication of the possibility of malignancy of an ulcer is a change in the nature of pain, which usually consists of the disappearance of their frequency and the appearance of constant dull pain. In some cases, the pain completely disappears. The ineffectiveness of a 4-6 week course of conservative therapy should raise suspicion of malignancy of the ulcer.
Endoscopic examination of the stomach is of great help in diagnosing malignant ulcers. The discovery in the stomach of an ulcer of an irregular, polygonal shape with uneven edges that have a bright red color, combined with the pale color of the mucous membrane adjacent to the ulcer, with an uneven, tuberous bottom, makes one think about the degeneration of the ulcer into cancer. Histological examination of a piece of tissue taken from the edges of an ulcer during endoscopic examination allows one to accurately determine the nature of pathomorphological changes in the lesion. Any suspicion of the presence of a malignant ulcer is an indication for radical surgery.
Perforation of an ulcer is one of the most serious complications of peptic ulcer disease. According to the literature, the frequency of perforations among all patients with peptic ulcer disease ranges from 3 to 30%. More often (in 55% of cases) perforation occurs in patients with duodenal ulcers.
With a perforated ulcer, the contents of the stomach or duodenum flow through a hole in the wall of the organ into the free abdominal cavity in 85% of cases, which contributes to the development of peritonitis and, if the patient is not treated in a timely manner, leads to death. In 6.5% of cases with perforation of the wall of the stomach or duodenum, the contents of these organs flow into the encysted spaces of the abdominal cavity (into the bursa of the lesser omentum, the right lateral canal), and in 8.5% of cases the perforation is covered by a neighboring organ (usually the greater omentum ), which prevents the contents of the stomach or duodenum from leaking into the abdominal cavity.
The diagnosis of perforation of the wall of the stomach or duodenum is based on clinical and radiological data. Mondor (1937) divided all the signs of a perforated ulcer into two groups: the main symptoms are pain, tension in the muscles of the anterior abdominal wall, previous gastric disorders and side symptoms, which he divided into functional, physical and general signs.
Pain is the first sign of ulcer perforation. It is characterized by suddenness of appearance and such pronounced intensity that it is compared to the pain “from a blow with a dagger.” The pain is initially localized in the epigastric region, and then quickly spreads throughout the abdomen. Sometimes the pain radiates to the supraclavicular region or the region of the scapula (on the right - if the perforation is located in the pyloroduodenal region, on the left - if it is in the body or vault of the stomach). If an ulcer located on the posterior wall of the stomach or duodenum perforates, the contents of these organs enter the retroperitoneal tissue or omental bursa and the pain is less intense.
Tension of the abdominal wall muscles is the first symptom detected during examination of the patient. It is determined by palpation of the abdominal wall, and sometimes is clearly visible. “As a rule, the abdomen is flat, contracted, often wrinkled and does not participate in respiratory movements” (Mondor). Muscle tension can be so pronounced that the stomach is called “wooden” or “board-shaped.”
An ulcer history, as a rule, can be identified by questioning the patient. However, in some cases, no signs of gastric disease can be established from the anamnesis - “silent ulcers”. According to the literature, “silent ulcers” occur in 2-37% of cases (S.S. Yudin). Among the functional signs, Mondor identifies: vomiting, retention of stool and gas, severe thirst.
Vomiting with a perforated ulcer can be early or late. Early vomiting occurs immediately after perforation and is of a reflex nature. Late vomiting appears in the stage of peritonitis due to intestinal paresis. It is extremely rare that when an ulcer perforates, bloody vomiting is observed. Retention of stool and gases often coincides with the onset of the disease and occurs before the development of peritonitis. However, sometimes this symptom is observed only in the presence of peritonitis. Severe thirst, according to many authors, is a common sign of ulcer perforation.
Physical signs are detected by inspection, palpation, percussion and auscultation. Patients with a perforated ulcer, as a rule, take a forced knee-elbow position, avoid unnecessary movements, have a pained expression on their face, and their skin is pale.
Palpation of the abdomen reveals muscular protection of varying degrees of severity and skin hyperesthesia. In cases where there is no pronounced “board-shaped” abdominal wall, Shchetkin’s symptom is always detected - Blumberg.
By percussion of the abdominal wall, it is possible to determine the presence of free fluid and gas in the abdominal cavity. Of great importance is the symptom of disappearance of hepatic dullness, which occurs in 86% of patients with a perforated ulcer.
Auscultatory symptoms for diagnosing perforated ulcers are not widespread. A rectal examination of the patient reveals the presence of tenderness in the anterior wall of the rectum (Kulenkampff symptom), indicating irritation of the pelvic peritoneum (pouch of Douglas). General symptoms include changes in pulse, respiration, and temperature.
In the clinical picture of a perforated ulcer when the contents of the stomach or duodenum enter the free abdominal cavity, depending on the time elapsed from the moment of perforation, three periods are distinguished.
- The first period (up to 6 hours from the moment of awakening) is characterized by a sharp expression of all the above symptoms and is defined as primary shock. The pulse is often slow (irritation of the vagus nerve, blood pressure is slightly reduced, breathing is shallow and rapid.
- The second period (from 6 to 12 hours from the moment of awakening - a period of imaginary well-being) is manifested by a gradual smoothing of the symptoms of the disease, an improvement in the general well-being of the patient, and often the appearance of euphoria. This is explained by the consequence of paralysis of the endings of the sensory nerves of the peritoneum. The pulse increases, the abdominal wall becomes less rigid, and breathing becomes freer. Exudate formed in the abdominal cavity is localized in the right iliac region, in the pelvic cavity. The pain shifts to the right iliac region, which often causes diagnostic errors (acute appendicitis is diagnosed). Against the background of apparent improvement, peritonitis develops.
- Third period (after 12 hours after perforation - the period of a clear clinical picture of diffuse peritonitis) - The patient’s general condition sharply worsens, facial features become sharpened, pain spreads throughout the abdomen, uncontrollable vomiting appears, retention of stool and gases, the tongue becomes dry, the abdomen is swollen, peristalsis there is no intestine, the pulse is up to 110-140 beats per minute, blood pressure decreases, body temperature rises to 38°.
With a covered perforation of the wall of the stomach or intestine (perforatio tecta), described for the first time in 1912 by A. Schnitzler, the contents of the organ do not enter the free abdominal cavity in large quantities. Therefore, the clinical picture has two periods:
- the first, when the contents of the organ begin to enter the abdominal cavity, is characterized by a typical picture of ulcer perforation;
- the second, when the perforation hole is covered, is manifested by a rapid subsidence of clinical symptoms, which is due to the cessation of the flow of organ contents into the free abdominal cavity. At the same time, abdominal pain disappears, the general condition of the patient improves, and tension in the muscles of the anterior abdominal wall decreases. However, palpation of the epigastric region causes pain, the Shchetkin-Blumberg symptom is determined here, and body temperature remains elevated.
Covered perforation in 8.5-15% of cases can result in self-healing. However, more often the protective barrier is destroyed and diffuse peritonitis develops.
Rice. 33. Radiographs of pneumoperitoneum: a — gas on the floor of the right dome of the diaphragm (patient standing position); b - gas between the edge of the costal arch and the liver (patient position lying down)
Diagnosis of perforation of the wall of the stomach or duodenum is helped by plain radiography of the abdominal cavity, which reveals the presence of free gas in it (Fig. 33). When the patient is in an upright position, this gas accumulates in the subdiaphragmatic space in the form of a crescent-shaped strip. In the presence of pneumoperitoneum and the corresponding clinical picture, the diagnosis of a perforated ulcer becomes indisputable. However, the absence of pneumoperitoneum does not always indicate the absence of perforation. The presence of free gas in the abdominal cavity during perforation of the wall of the stomach or duodenum occurs in 47-80% of cases (N.E. Dudko, S.S. Yudin).
If you find an error, please select a piece of text and press Ctrl+Enter.
Pages: 5
Complications of ulcers
If left untreated, complications may develop. There are 5 conditions that threaten the patient if the ulcer is not treated:
- Perforation of an ulcer is a perforation of the stomach wall through.
- Bleeding - if the integrity of the blood vessel in the walls or at the bottom of the ulcer is damaged.
- Stenosis of the pyloric region of the stomach is a narrowing of the outlet of the stomach, accumulation of food there.
- Penetration of an ulcer is the perforation of an ulcer into a neighboring organ.
- Malignancy of an ulcer is the growth of a malignant tumor.
Possible complications
Peptic ulcer disease is most dangerous due to its complications, which arise if diagnosis and treatment are not timely.
All of them require immediate hospitalization of the patient in the surgical department:
- Hemorrhage into the lumen of the stomach - occurs most often in the acute phase of the disease. Sometimes leads to the development of hemorrhagic shock.
- Perforation (perforated ulcer) into the lumen of the abdominal cavity with the development of peritonitis.
- Penetration of an ulcer with chemical damage to nearby anatomical structures (liver, pancreas, omentum).
- Deformation of the lumen of the stomach.
- Development of a malignant neoplasm (stomach cancer).
Methods for diagnosing stomach ulcers
In order to make a final diagnosis, it is necessary to undergo esophagogastroduodenoscopy
(EGD)
, the more common name is gastroscopy.
An endoscope is inserted through the mouth and esophagus into the stomach.
- This is a thin tube that is equipped with a special optical device. Thus, the doctor gets the opportunity to clearly see the gastrointestinal tract from the inside. Endoscopy allows you to assess the size of the ulcer, number (with multiple processes), localization, and the presence of complications. During the study, samples of gastric juice are taken, a biopsy of the mucous membrane for morphological examination and the presence of Helicobacter pylori. If the patient does not tolerate the procedure of such a study, it is recommended to use medicated sleep. To clarify the depth of the ulcer, gastrointestinal motility, some complications of peptic ulcer disease, such as stenosis, penetration, etc., fluoroscopy and radiography with a contrast agent are used. Diagnostic procedures may also include tests for Helicobacter pylori, laboratory testing of urine, blood and stool. Ultrasound does not allow a diagnosis of peptic ulcer.
Diagnostics
If, based on the results of a patient interview, there is a suspicion of a callous ulcer, a number of examinations are performed, including those listed below.
- Blood analysis. Allows you to detect a decrease in hemoglobin and the development of anemia. Other indicators will be normal.
- Palpation in the area of projection and small flexure of the stomach. A new formation similar to a tumor is palpable.
- Radiography. Shows a specific niche in the stomach wall. The ulcer will be characterized by smooth and even edges and bottom.
- Endoscopy. Allows you to examine ulcerative lesions, assess their size and severity. The ulcer does not deform after touching the probe.
- Biopsy of scar tissue. The sample is sent for histological and cytological analysis, which makes it possible to detect the development of cancer at an early stage, as well as study the structure of the cells.
Treatment methods for stomach ulcers
It is important for patients to adhere to the established daily routine, avoid stressful situations if possible, not resort to smoking and drinking alcoholic beverages, at least for the duration of treatment, follow the diet prescribed by the doctor, and adhere to the correct daily routine. As usual, the duration of the active course of treatment is about two weeks, and then maintenance therapy is required with mandatory adherence to proper nutrition.
Individual treatment is selected for each patient, taking into account such significant factors as age, physical condition, and the presence or absence of concomitant chronic diseases. A stomach ulcer is characterized as a rather serious, deadly disease, therefore, at the slightest suspicion, you should immediately undergo diagnosis by visiting a specialist doctor.
Drug therapy consists of the following drugs:
- antibacterial drugs
- the action is aimed at eliminating Helicobacter pylori from the body; - antacids
- drugs that reduce the secretion of gastric juice; - proton pump inhibitors
- their action affects the chemical composition of hydrochloric acid and disrupts its structure; - H2-histamine blockers
- reduce the aggression of gastric secretions; - antispasmodics
are symptomatic drugs that relieve pain.
Medicines must be taken strictly as recommended by a doctor. Each of the medications is indicated only under certain circumstances of the disease. Medicines must be taken within the prescribed period. If the patient feels relief, this does not mean that the drugs can be discontinued on their own. The process of drug treatment is controlled by the attending physician; only he can make any changes to the intake.
Gastric resection
The most common operation for peptic ulcer disease is gastric resection. It can be carried out both as an emergency (for bleeding or perforation) and as a planned procedure (chronic long-term non-healing, often recurrent ulcers).
From 1/3 (for ulcers located close to the outlet) to 3/4 of the stomach is removed. If malignancy is suspected, subtotal and total resection (gastrectomy) may be prescribed.
gastrectomy
Resection of part of the stomach is preferable, rather than simply excision of the area with the ulcer, because:
- Removing only the ulcer will not solve the problem as a whole, the peptic ulcer will recur, and you will have to do a second operation.
- Local excision of the ulcer followed by suturing of the stomach wall can subsequently cause severe cicatricial deformation with impaired passage of food, which will also necessitate a repeat operation.
- The gastric resection operation is universal, it has been well studied and developed.
Preparing for surgery
To clarify the diagnosis, the patient must undergo:
- Gastroendoscopy with biopsy from the ulcer.
- X-ray contrast examination of the stomach to clarify the function of evacuation.
- Ultrasound or CT scan of the abdominal cavity to clarify the condition of neighboring organs.
In the presence of concomitant chronic diseases, consultation with relevant specialists is necessary, compensation for vital systems (cardiovascular, respiratory, blood sugar levels, etc.). In the presence of foci of chronic infection, their sanitation is necessary (teeth, tonsils, paranasal sinuses).
At least 10-14 days before surgery, the following are prescribed:
- Blood and urine tests.
- Coagulogram.
- Determination of blood group.
- ECG.
- Biochemical analysis.
- Blood testing for the presence of antibodies to chronic infectious diseases (HIV, hepatitis, syphilis).
- Examination by a therapist.
- Gynecologist examination for women.
Progress of the operation
The operation is performed under general endotracheal anesthesia.
An incision is made along the midline from the sternum to the navel. The surgeon mobilizes the stomach and ligates the vessels leading to the part to be removed. At the border of removal, the stomach is stitched either with an atraumatic suture or with a stapler. The duodenum is stitched in the same way.
Part of the stomach is cut off and removed. Next, an anastomosis is performed (most often “side to side”) between the remaining part of the stomach and the duodenum, less often – the small intestine. A drain (tube) is left in the abdominal cavity, and a tube is left in the stomach. The wound is sutured.
You cannot eat or drink for several days after the operation (intravenous infusion of solutions and liquids is being established). The drainage is usually removed on the 3rd day. The stitches are removed on 7-8 days.
Painkillers and antibacterial drugs are prescribed. You can get up in a day.
Surgical treatment (surgery to remove stomach ulcers)
The need for surgical intervention may arise only in case of long-term non-healing ulcers, or when complications occur. Such an operation can be planned or carried out urgently. Emergency surgical intervention is indicated for perforation of the ulcer, bleeding that cannot be stopped by conservative measures. The ulcer is sutured, the bleeding is stopped, and the narrowing of the digestive tube is widened. Previously used planned operations to remove a section of the stomach in order to reduce its secretion are now practically not used, since properly selected modern drug treatment, as a rule, leads to remission.
In case of malignancy (malignancy) of an ulcer, surgical treatment is necessary, the extent of which depends on how early the tumor is detected - whether it has managed to grow through all layers of the stomach, or has only affected the mucous and submucosal layers, whether it has managed to spread to nearby organs or lymph nodes, or has already gave metastases to distant organs. The earlier the malignancy of the ulcer is detected, the less the scope of surgical intervention will be. In this case, surgery to remove the ulcer can be performed endoscopically or laparoscopically. Otherwise, extended intervention is carried out in the traditional way.
Diagnostic measures
To diagnose callous ulcer pathology, the gastroenterologist must conduct a very thorough examination of the patient. The first thing the specialist does is collect an anamnesis of the disease, he conducts a survey of the patient, the purpose of which is to obtain information about his lifestyle, working conditions, nutrition, and rest. After this, the patient’s temperature and pressure are measured, and the doctor begins palpation. During an examination of the abdominal cavity using this technique, the gastroenterologist will be able to feel a small compaction in the stomach area, which has smooth contours and somewhat resembles a benign or malignant neoplasm.
After a personal examination of the patient, the specialist prescribes a set of laboratory and instrumental tests:
- First of all, the patient takes tests of stool, blood and urine . It is worth noting that with this form of pathology, the result of blood tests will be generally good, with the exception of the hemoglobin level, which will be underestimated due to developed anemia.
- Without fail, the patient is sent for radiography , which is carried out using a contrast agent. This diagnostic technique allows you to assess the condition of the walls of the stomach and identify a characteristic niche (or multiple foci) on them, which has a smooth bottom and edges.
- Examination of the stomach using an endoscope . This diagnostic technique allows you to visually assess the condition of the mucous membrane and identify all lesions. At the same time, specialists collect biological material, which is sent for histological examination. Histology results can identify cancer cells or confirm the benign origin of the pathology.
This is interesting: How dangerous is hepatitis C carriage and what awaits a person with such a diagnosis
Prevention and prognosis
To prevent gastric ulcers, you should:
- devote at least 6 to 8 hours of sleep per day;
- minimize the consumption of smoked, fatty and fried foods, such foods irritate the mucous membrane;
- take care of your dental health so that you can always chew food well;
- avoid frequent stressful situations, as they lead to nervous tension and cause pain in the stomach;
- do not drink alcoholic beverages or smoke;
- If you have stomach pain, undergo the necessary examinations;
- increase the number of meals to 6 per day. Food should be chopped, jelly, porridge, steamed meat, omelet, vegetables are indicated.
Symptoms
This form of ulcerative pathology is accompanied by characteristic symptoms, which, as a rule, manifest themselves during an exacerbation:
- Severe pain syndrome, which has a cutting and stabbing nature . In most cases, pain occurs at night, as well as after meals. Quite often, pain can radiate to the spine or to the left side of the chest, which is why some patients mistakenly suspect they have heart problems.
- Loss of appetite (partial or complete) , which is why people begin to rapidly lose weight. Severe weight loss due to prolonged fasting can provoke another attack of pain.
- Gag reflex , after which the patient experiences a brief feeling of relief.
- Heartburn , which may be followed by belching. These symptoms appear due to the fact that food accumulates in the patient’s stomach, in which putrefactive processes begin. The patient’s condition can improve after taking an adsorbent, for example, activated carbon, or artificially inducing a gag reflex.
- Disruption of bowel movements , for example, intestinal upset or constipation. Patients also experience increased gas formation and rumbling in the stomach.
- A very unpleasant odor emanates from the oral cavity . It becomes more severe in the morning, immediately after waking up.
- Salivation increases due to disruptions in the digestive system.
- Due to the fact that the ulcer constantly bleeds, the patient develops anemia.
- Severe intoxication of the body occurs.
- Headaches appear , which in terms of intensity can be classified as migraine.
- Sleep is disturbed.
- Patients experience frequent outbursts of anger, which gradually give way to a depressive state .
If people notice alarming symptoms, they should not self-medicate, since incorrectly chosen medications or folk recipes can lead to very disastrous consequences. At the first manifestations of a callous ulcer, they need to contact a medical institution, a gastroenterologist.
Important
- We should not forget that a stomach ulcer affects the functioning of the entire body, and therefore it is better to prevent this disease than to then adapt to it all your life, easing the pain with medications.
- Attacks can be prevented by following a diet and proper nutrition, giving up alcohol and cigarettes. You should visit a doctor at least once a year. For preventive purposes, patients are prescribed antiulcer medications in courses in spring and summer. It is at this time that the disease makes itself felt with the most striking manifestation of symptoms.
- It is also necessary to remember for patients suffering from peptic ulcer disease about annual endoscopic monitoring, which must be completed even in the absence of pain after the ulcer has healed. The need for such control is associated with the high probability of malignancy of gastric ulcers.
Author of the article: Tryapitsyn Alexander Valerievich (gastroenterologist, candidate of medical sciences)
Nature of the pathology
Callous gastric ulcer is considered a complication of peptic ulcer disease when it lasts for a long time, with inadequate therapeutic tactics. The manifest form of callous ulcer can be established over long-term observations. This type of ulcer is characterized by high, rigid and slightly undermined edges, similar to calluses, the bottom is lumpy, heterogeneous, and covered with necrotic plaque.
The mucous membrane in the pathological focus is infiltrated, reminiscent of a non-healing wound. The primary diagnosis of peptic ulcer disease never determines the callous process, but after 3-4 months the examination is repeated. If the wound does not heal, then a biopsy is performed to examine the structure of the pathological unit. The main features of the pathology include: patients experience severe pain; the gastric mucosa is not restored; frequent exacerbations of the disease.
The mechanism of the disease is due to the constant exposure of various irritants to the gastric mucosa as a result of reduced protective function of the stomach. Regular damage to ulcerated tissue by hydrochloric acid literally burns through the mucous structure of the stomach from the submucosal layer down to the cell membranes. Callous ulcers take a long time to form, and the disease gradually becomes chronic. Cases of exacerbation occur quite often, which is due to constant discomfort and pain in the stomach.
This is interesting: Can a child have an enema if he has diarrhea?
Prevention
The goal of preventive measures is to eliminate the negative impact on the gastric mucosa and thereby prevent the development of ulcers. For these purposes, doctors recommend the following:
- in case of existing stomach pathology, even the most insignificant at first glance, it is imperative to undergo treatment in a timely manner;
- try to adhere to a healthy lifestyle;
- use medications only as prescribed by a doctor;
- avoid stressful situations or learn to relieve negativity with the help of your favorite hobby;
- monitor your diet and minimize the consumption of junk food and carbonated drinks. You need to remember that one cup of coffee invigorates, the second dehydrates the body, and the third and subsequent ones cause irreparable harm.
Protecting yourself from callous ulcers is not as difficult as it might seem. The main thing is to listen to your own body and not ignore its signals. Only in this case will it be possible to avoid irreversible consequences and live a long life.
Definition of disease
The danger of this pathology is that from the moment of formation and scarring the ulcer does not change its type. Upon palpation, such a formation cannot be deformed, and the shape of the ulcer does not change even when the probe comes into contact.
Often, it is by the type of edges that a specialist determines how the wound zone was formed, for example:
- if the edges are uneven or their outlines are curved, this indicates that the ulcer was formed intermittently;
- in the case when the scars are outlined with smooth edges, this means that the pathology developed intensively and continuously.
If the ulcerative formation does not heal after drug therapy, the patient should undergo a detailed examination, the purpose of which is to refute or confirm suspicions of the development of a callous disease. For these purposes, the following methods are used:
- collection of biological material to determine hemoglobin levels;
- initial examination by palpating the flexure of the stomach to identify a neoplasm;
- X-ray. This type of examination is necessary to determine the affected area in the gastric wall;
- endoscopy. Using this technique, it is possible to visualize foci of ulcerative pathology. As a rule, if a patient actually develops a callous ulcer, the mucous membrane will be covered with small erosive formations and folds, the origin of which is taken from the zone of dislocation of the pathology. Moreover, after touching the probe, the ulcer will not change its shape.
In addition, it is necessary to conduct histology and cytology. These studies will help determine the structure of the formation and identify malignant cells at the initial stage.
Symptoms
A callous ulcer always remains in the form it took during scarring. It does not deform upon palpation or when a probe touches it. Judging by the appearance of the edges of the ulcer, one can understand what the entire process of its formation was like:
- Curved, uneven outlines indicate its impetuous formation;
- An even scar indicates that it was formed in a measured and stable manner.
A callous ulcer is a consequence of an acute ulcer. By neglecting treatment, as well as supportive therapy and diet, a person provides all the conditions for the development of a chronic disease.
If such symptoms appear only at their initial stage, you should immediately seek medical advice and help.
Symptomatic complex
Signs of a callous ulcer appear gradually, increasing as the disease progresses. The main symptoms of peptic ulcer disease are the following:
- severe pain;
- increased gastric secretion;
- metabolic disorders;
- Iron-deficiency anemia;
- Digestive problems.
Seasonality does not affect the frequency and episodes of exacerbations, which is associated with the characteristics of scar tissue. Pathologically changed tissue at the site of ulceration loses its ability to regenerate, so the wound does not heal. The intensity of pain may also depend on the main location of the damaged stomach tissue. Unpleasant sensations occur when eating and on an empty stomach after waking up. Pain from a callous ulcer is radiating in nature and is felt by patients even in the spinal regions.
Another distinctive feature of the disease is the appearance of hungry night pains. The disease can also cause other symptoms:
- vomiting and regular nausea;
- excessive salivation;
- constant heartburn;
- sour belching;
- problems with stool (frequent constipation).
After profuse vomiting, patients often experience relief, so inducing vomiting for many patients is one of the options to alleviate the pain syndrome. With callous ulcers, patients lose weight due to the psychological connection between food and pain. Patients simply stop eating, keeping their diet to a minimum in order to avoid discomfort.
Minor signs
The disease is often provoked by dyspeptic disorders and internal intoxication, which provokes the occurrence of additional symptoms:
- headaches, even migraines;
- frequent mood swings and emotional instability;
- insomnia;
- hot flashes in women.
Pain from callous ulcers is localized in the stomach, so clinical manifestations are often confused with cholecystitis. All symptoms can be attributed to an intensively developing stomach ulcer. Signs usually appear during exacerbations of a chronic process. A clear manifestation of symptoms is expressed precisely in the exacerbation stage. During the period of remission, pain is manifested by mild pain that appears at night.
Surgery to eliminate a progressive ulcer
Callous gastric ulcers can only be treated surgically. The affected tissue is treated with a special laser, thus causing cell regeneration. Also during the operation it is possible to suturing the ulcer and excision it based on indications. Next, the patient is prescribed complex drug treatment aimed at restoring the functions of the stomach and intestines. For treatment, drugs are used that promote rapid regeneration of damaged areas.