Types of disease
There are two basic types of intestinal ulcers: large intestine and small intestine.
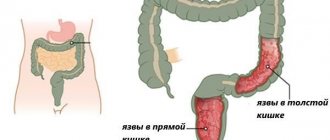
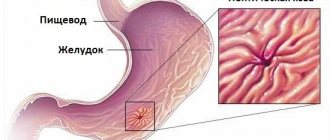
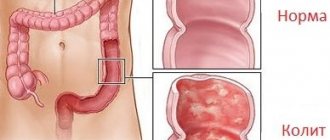
An ulcer of the large intestine often develops into ulcerative colitis, a chronic disease that occurs with exacerbations due to a failure of metabolic functions or a genetic predisposition to inflammation. With a colon ulcer, the integrity of the epithelial layer is disrupted and single or multiple lesions begin to appear. This form can develop over a long period of time; with routine medical examinations, it is possible to diagnose the disease on time and cure the ulcer.
A small intestinal ulcer is an inflammation of the mucous membranes of the small intestine under the influence of an acidic environment. Ulcerations in the small intestine are not so common, and therefore the pathology is considered nonspecific. It can occur in an acute form or have a chronic course. Exacerbation of the ulcer occurs more often in the off-season - spring-autumn; in the remission phase it may not even manifest any symptoms. The number of ulcerations varies from single to numerous.
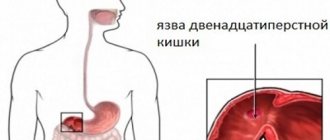
More often than others, a duodenal ulcer is formed. More often, this pathology appears in adults aged 30–60 years. This disease occurs more often in men than in women due to smoking and alcohol abuse.
Ulcer symptoms
The main symptoms of an intestinal ulcer can be compared with those that appear during inflammation of the gastric mucosa. They appear immediately, so a diagnosis can be made in time. With an intestinal ulcer, the symptoms are as follows:
- heartburn;
- the pain syndrome has a boring, hungry and pulling character, localized in the lower abdomen. Pain from an ulcer can radiate to the spine, behind the sternum;
- with an ulcer, the stool becomes black, its consistency is tarry, viscous;
- with increased acidity, the pain becomes more frequent, which provokes belching. Food takes a long time to digest;
- the presence of pain during an intestinal ulcer provokes a gag reflex and profuse vomiting.
Symptoms of ulcerative colitis include the following manifestations from the body:
- diarrhea, sometimes mixed with blood, rarely pus;
- abdominal pain;
- the ulcer provokes weakness, apathy and weight loss;
- lack of appetite;
- increased body temperature;
- internal bleeding;
- perforation.
During exacerbation, the following symptoms of an ulcer appear:
- cramping abdominal pain;
- diarrhea with blood, mucus;
- body temperature 39 degrees;
- vomit;
- flatulence.
Having discovered the listed symptoms of an ulcer, the patient should take urgent measures and visit a doctor. Treatment of ulcers is a long, labor-intensive and painful process that should not be neglected.
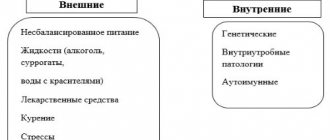
Causes of intestinal ulcers
There are 4 factors that contribute to the development of ulcers:
- presence of the bacterium Helicobacter pylori. This bacterium affects the stomach and duodenum, lives under the mucous membrane, preventing the healing process of erosions from beginning.
- hereditary predisposition. If one of the parents has an ulcer, there is a possibility that the child will develop one in the future.
- presence of bad habits - smoking and alcohol abuse (can cause alcoholic gastritis).
- improper diet, eating junk food. Eating on the go, snacking from fast food, lack of a diet - all this disrupts the functional activity of the stomach and intestines, and can become an impetus for the development of initial pathologies.
The process of accelerating the formation of stomach ulcers can be facilitated by the lack of adequate treatment for previous pathologies, frequent stress, poor sleep, and abuse of non-steroidal anti-inflammatory drugs.
Professional activity plays a significant role in the formation of intestinal ulcers - it can cause stress, interfere with active life, and limit physical activity.
Prevention
The basis of preventive measures is proper nutrition and the elimination of abuse of medications and alcoholic beverages. At the first symptoms, you should consult a doctor rather than carry out self-treatment. In this case, it is possible to prevent the chronicization of the pathological process and exclude the development of complications.
Esophageal diverticula are a pathological process that is characterized by deformation of the esophageal wall and protrusion of all its layers in the form of a pouch towards the mediastinum. In the medical literature, esophageal diverticulum also has another name - esophageal diverticulum. In gastroenterology, this particular localization of saccular protrusion accounts for about forty percent of cases. Most often, the pathology is diagnosed in males who have crossed the fifty-year mark. But it is also worth noting that usually such individuals have one or more predisposing factors - gastric ulcer, cholecystitis and others. ICD 10 code – acquired type K22.5, esophageal diverticulum – Q39.6.
Signs of an intestinal ulcer
A stomach ulcer in some advanced cases is considered a direct threat to the patient’s life, so the patient may require hospitalization and surgical intervention. The disease manifests itself:
- Diarrhea, which may alternate with constipation.
- Vomiting and nausea after eating food.
- Frequent heartburn.
- Pain before and after meals in the upper and lower abdomen, colic.
Background signs are: loss of appetite, fatigue, vitamin deficiency, lethargy.
Symptoms of duodenal and stomach ulcers strongly resemble gastric lesions of the organs. The main distinguishing feature of one from the other is that gastritis usually worries constantly and for a long time, and ulcers tend to appear and disappear again. The chronic nature of the pathology causes exacerbations in the spring and autumn, but the signs of an ulcer are usually more pronounced than with gastritis.
With stomach and duodenal ulcers, symptoms can appear in the early stages, and they are expressed by the following signs: boring pain, nagging pain in the lower abdomen (possibly under the sternum and in the middle of the spine), such symptoms are possible especially after eating and only go away with the onset of hunger. Such painful sensations can provoke a gag reflex or a desire to induce it. After this, the unpleasant symptoms disappear, but soon return. The stool becomes black and becomes viscous.
Increased acidity provokes pain, heartburn, and sour belching.
The symptoms of an ulcer in each patient can be expressed differently, and the pain is of a different nature depending on whether there is a single ulcer or multiple lesions are present, and the symptoms also depend on the level of stomach acidity and the depth of tissue damage.
A common symptom is “hunger pain,” which occurs more often at night, or no earlier than 2 hours after eating.
Symptoms of an intestinal ulcer, in addition to pain, include:
- heaviness in the stomach;
- poor appetite;
- general malaise;
- gray-brown coating on the tongue;
- nausea.
An ulcer of the small intestine is manifested by the presence of: diarrhea, fever, abdominal pain of various types, cramps, vomiting, colic (before or after eating), heartburn.
Symptoms of a colon ulcer are: pain in the anus, atypical discharge from the anus, flatulence, abdominal distension, frequent uncontrolled release of gases, mucus and blood may be present in the stool.
Often the symptoms of colon ulcers overlap with signs of other diseases. This can be explained by the fact that the ulcer does not have any specific signs, so differential diagnosis is recommended to make the correct diagnosis.
In some cases, there are no signs of a small intestinal ulcer, and acute manifestations occur only when the ulcer is perforated.
Symptoms
The signs of an intestinal ulcer at an early stage will be almost identical to how the inflammatory process occurs in this organ.
Symptoms of a small intestinal ulcer are as follows:
- a pain syndrome of a pulling, cramping nature, which often radiates to the retrosternal region, to the spine;
- heartburn, which intensifies after eating, while diet does not play a special role;
- repeated vomiting, which intensifies after eating and does not always bring relief;
- stool becomes black, which will indicate rectal or internal bleeding (a solitary rectal ulcer may be suspected);
- diarrhea, in especially severe cases, pus will be present in the stool;
- loss of appetite;
- weight loss;
- pale skin, increased sweating at night;
- increased body temperature;
- weakness;
- symptoms of anemia.
With an exacerbation of the pathological process, the clinical picture will be characterized as follows:
- high body temperature – up to 39 degrees;
- increased flatulence;
- cramping abdominal pain;
- diarrhea up to 10-15 times a day, mixed with blood and mucus.
Such clinical signs require immediate medical attention, since in its advanced form, an intestinal ulcer leads to perforation of the intestinal walls and even death.
Treatment of intestinal ulcers
Treatment of intestinal ulcers begins with eliminating the causes that caused it. For example, if the bacteria Helicobacter pylori is present in the body, antibiotics will be included in the treatment regimen.
Conservative treatment of intestinal ulcers consists of taking medications that eliminate the cause of the pathology and relieve the symptoms of the disease, following a strict diet for a long time.
In the acute stage, the ulcer is treated only in a hospital setting, since at this time the patient may require bed rest and medication treatment. The course of treatment for intestinal ulcers includes the use of different groups of drugs:
- antibacterial;
- having an antisecretory effect;
- antacids;
- bismuth-containing;
- prokinetics.
In addition, the patient may be prescribed medications to strengthen the immune system and replenish the lack of nutrients and vitamins.
When drug treatment does not show its effectiveness for a long time, and the patient gets worse, surgery is considered the only way out. It must be performed in case of bleeding - since this is a direct threat to human life.
Treatment with folk remedies
For non-advanced ulcerative lesions, when surgery is not required, treatment at home can help.
To relieve spasms, soothe the mucous membranes, and get rid of nausea, it is effective to drink decoctions and tinctures of chamomile, sage, mint, and calendula.
To normalize the intestinal microflora, it is recommended to consume lactic acid products.
To normalize stool and relieve spasms, it is good to use flax seeds or jelly made from them. To do this, eat flax seeds (2 tablespoons) that have been boiled on an empty stomach, or drink half a glass of jelly.
Cumin will help eliminate strong rumbling and reduce gas formation. Dried apricots and prunes will help regulate stool.
Aloe juice will speed up the healing of intestinal ulcers. 1 tbsp. Mix a spoonful of juice and a spoonful of honey and drink it.
By diluting honey with novocaine, you can stop the process of intestinal destruction during ulcers and relieve pain.
A mixture of white clay with water (1 tbsp per 200 ml of water) can reduce acidity and relieve heartburn.
To prepare propolis tincture, grind 200 g of the product and add 100 ml of alcohol with a strength of 70%. Leave at room temperature for three days, shaking occasionally. It is recommended to use 2-3 times an hour before meals, 20 drops diluted in warm water.
To prepare an aloe tincture with honey and red wine, aloe leaves are passed through a meat grinder in such a quantity that they fill half a glass. Add honey to them (three-quarters of a glass) and leave for three days in a dark place. Red wine (1 glass) is poured into the resulting mixture and left in the dark for a day. Consume 1 tbsp before meals three times a day. spoon for several months.
Treatment
Conservative treatment of intestinal ulcers consists of taking medications and following a diet.
The pharmacological part of treatment includes taking the following medications:
- laxatives or astringents, depending on the current symptoms;
- antispasmodics;
- non-steroidal anti-inflammatory drugs.
It is mandatory to follow a diet, and the specific dietary table will be selected by the attending physician on an individual basis.
If conservative treatment does not give the desired result or is not at all effective in a certain clinical case, surgery is performed - the affected area of the intestine is subject to resection. A solitary rectal ulcer often leads to complications than other forms of this disease.
Diet for intestinal ulcers
If you have an intestinal ulcer, you should be careful about your diet. A number of foods should definitely be excluded from your diet:
Among the provocateurs that cause symptoms of intestinal ulcers:
- black bread;
- products with coarse fibers;
- marinades;
- canned food
Such products contribute to irritation of the intestinal mucosa and can cause the development of an inflammatory process along the edges of the ulcer. There are also dishes, the use of which has a positive effect on the condition of the organ - they have the ability to envelop the stomach and intestinal walls and reduce pain, even until it disappears completely. These dishes include:
- mashed potatoes, broccoli, zucchini puree;
- pureed soups; milk soups;
- slimy porridge (from oatmeal);
- steamed minced meat or fish products.
Puree-like boiled or steamed lean dishes, baked vegetables or fruits have similar properties. All food consumed should be as finely chopped as possible and not hot, but at a comfortable temperature.
A significant role in the treatment of intestinal ulcers is played by fractional balanced nutrition. The patient is advised to adhere to a diet that helps the ulcers heal.
During the acute phase of the ulcer, olive oil or butter should be added to soups and cereals. It is recommended to add to the diet for intestinal ulcers: milk porridge, veal, chicken, turkey, biscuits, crackers, stale bread, honey, jam, jelly, marshmallows, homemade jelly, tea with milk, non-carbonated mineral water. Thanks to a balanced diet, ulcers will heal better and the healing process will occur faster.
Video on the topic:
Causes of the disease
Causes of pathology:
- mechanical damage to the mucosa;
- vascular diseases (thrombosis, constrictions, spasms);
- improper diet;
- chronic overwork, a large number of stressful situations;
- depression;
- bad habits (tobacco smoking, alcoholism);
- genetic predisposition (in some people, the production of gastric juice exceeds the norm, this pathology is inherited).
There are several mechanisms for the development of small intestinal ulcers:
- negative effect on the mucous membrane of hydrochloric acid;
- penetration of pathogenic microorganisms into the gastrointestinal tract, causing ulceration.
Disease prevention
To prevent the disease, certain rules must be followed:
- get rid of bad habits;
- Healthy food;
- avoid stressful situations;
- If you suspect a disease, contact a specialist.
List of references: https://astery-med.ru/whatailsyou/pishevarenie/zab_tol_kishki.php https://www.kp.ru/guide/zabolevanija-kishechnika.html https://empendium.com/ru/chapter/B33 .II.4.28. https://www.gmsclinic.ru/diseases/inflammatory-bowel-diseases https://apteka911.com.ua/medical-uses/yazva-pryamoy-kishki-s16791 https://astery-med.ru/whatailsyou/ pishevarenie/zab_tonk_kishki.php https://www.cochrane.org/ru/CD011523/UPPERGI_medicamentoznoe-ili-operativnoe-lechenie-pri-yazvennoy-bolezni-zheludka-i-verhnih-otdelov-tonkoy dr-kruglov.ru/instrumentalnyie- metodyi-diagnostiki-i-lecheniya/diagnostika-onkologicheskih-zaboleva/opuholi-bryushnoy-polosti-i-zabryushinno/dobrokachestvennyie-opuholi-zheludka-i/yazva-tonkoy-kishki/ https://policlinica.ru/yazva-tonkoy- kishki-prostaya.html https://ru.wikipedia.org/wiki/Dodenal_ulcer https://www.medkompas.ru/about-health/diseases/yazva-dvenadcatiperstnoy-kishki/ https://tsn.ua/ru/ blogi/themes/health_sport/kak-izbezhat-yazvy-dvenadcatiperstnoy-kishki-1171413.html https://yandex.ru/health/turbo/articles?id=4415 Notes from the author of the article, based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/18/2020
What is a small intestinal ulcer: description of the pathology
A small intestinal ulcer is a lesion of the mucous and submucosal layer of the intestinal wall with the formation of a defect. The name has several synonyms - nonspecific, idiopathic, round, simple, etc.
Often the disease is asymptomatic for a long time, so it is diagnosed after it has become chronic. During the pathology, relapses (exacerbations) are replaced by periods of remission.
Most often, signs of intestinal ulcers are found in men 30-60 years old.
Classification
In the international classification ICD 10, the disease is coded as K63.3 - intestinal ulcer or primary ulcer of the small intestine.
Full explanation of the diagnosis:
- K00-K93 - diseases of the digestive system;
- K55-K63 - other intestinal diseases;
- K63 - other intestinal diseases;
- K 63.3 - intestinal ulcer.
Complications
They are quite rare (up to 3-5% of cases), but have a high incidence of deaths (up to 90%).
Complications include:
- Perforation of an ulcer (perforation) is a rupture of the intestinal wall with the release of contents into the abdominal cavity. Depending on the location of the perforation, diffuse or local peritonitis (inflammation of the peritoneum) may develop.
- Intestinal bleeding - develops when the vessels supplying the small intestine are damaged. Minor bleeding may occur without obvious symptoms. They are detected during laboratory tests (traces of blood are found in the stool). More massive bleeding is accompanied by changes in stool (melena - tarry stool), hemodynamic disturbances (increased heart rate, decreased blood pressure). A picture of posthemorrhagic anemia develops.
- Cicatricial narrowing of the lumen of the small intestine (stenosis) - slowing down the passage of the food bolus until the development of intestinal obstruction.
Complications most often develop in patients who have undergone surgery on the abdominal organs. Such conditions require emergency surgery.
Manifestations of colonic lesions
Symptoms of rectal ulceration often manifest as pain during bowel movements.
Colon ulcer
- The intensity of pain varies widely, periodically disturbing the patient at rest. However, when visiting the toilet, the patient feels more pain.
- In addition to pain, the patient experiences bleeding or slight bloody discharge from the anus. Bleeding increases with emptying the rectum.
- If the ulcer is infected, pus or copious amounts of mucus are released from the anus.
- Damage to the rectum is characterized by special spastic contractions that simulate the urge to defecate, called tenesmus. False urges can be extremely painful, causing suffering to the patient.
- Chronic constipation has become a common symptom of chronic intestinal ulcers.
- With prolonged intestinal bleeding, anemia develops due to significant blood loss.
- An infection of the rectum is characterized by severe itching. In the area of the anus, skin irritation, ulcers and weeping were recorded.
An early sign of an ulcerative lesion of the rectum is the sudden appearance of loose stools, which have no apparent reason for the development. Sometimes the stool contains mucus, foam or blood. The patient's body temperature does not change.
Differential diagnosis
The symptoms listed above may be characteristic manifestations of other diseases affecting the intestines. It is important to carry out accurate differentiation for treatment.
A rectal ulcer is differentiated by the development of anal fissures, inflammation of the hemorrhoidal veins, rectal polyposis, benign and malignant neoplasms of the intestine, and inflammation of the tissue around the rectum.
Diagnostic procedures
First of all, the doctor carefully examines the patient’s complaints and history, analyzes the character, and carefully examines the patient. The general condition of the patient and the local condition of the rectum are assessed using digital examination. To make a final diagnosis, it is necessary to conduct a laboratory and instrumental examination, including the following types of research:
- Sigmoidoscopy.
- Irrigoscopy.
- Colonosocpia.
Diagnostic features
The clinical picture of a small intestinal ulcer is nonspecific, so making an accurate diagnosis can be difficult.
The algorithm includes:
- Interviewing the patient, collecting complaints and medical history.
- Physical examination, palpation of the abdomen.
- Lab tests.
- Instrumental research.
Differential diagnosis is carried out with secondary ulcers (for tuberculosis, typhoid fever), damage to the large intestine, and gastric ulcers.
Data collection and inspection
The examination begins with the collection of complaints and medical history. During a conversation with the patient or his relatives, the doctor finds out:
- The nature of the complaints is the severity of pain, the connection with food intake, physical activity and other factors, the presence of nausea and vomiting, and extraintestinal manifestations.
- How long ago did the complaints appear, how did the symptoms develop?
- Do the patient’s immediate blood relatives suffer from gastrointestinal diseases?
- How does a person eat, what foods predominate in the diet.
- What concomitant diseases, injuries, surgeries did he undergo?
During the examination, pay attention to the general condition, body weight (in patients with damage to the small intestine it is usually reduced). The skin is dry and pale, and there may be “seals” in the corners of the mouth.
Palpation of the abdomen reveals tension in the abdominal wall, local pain in the epigastric region or upper right.
Instrumental studies
Endoscopic examination can identify ulcers. Diagnosis is carried out using a flexible endoscope and a miniature video camera. If necessary, a tissue sample can be taken for histological examination.
Examination of patients with ulcers of the jejunum and ileum is significantly difficult due to the anatomical features of these organs. Standard research methods (radiography, endoscopic methods) make it possible to identify pathology of the duodenum, but do not allow assessing the condition of the small intestine.
Experts call a relatively new method, capsule endoscopy, more effective. A special “video capsule” is introduced into the body, which moves through the intestines and takes a large number of pictures. The data is transferred to the recording device.
The effectiveness of such diagnosis may be reduced if the ulcerative defect is located in a fold or there is an area of stenosis in the intestine. Laparoscopic surgery and ultrasound of the abdominal organs help diagnose complicated ulcers.
Laboratory research
There are no specific laboratory tests that can identify an ulcer with 100% certainty. However, there are indirect signs that, in combination with complaints and instrumental studies, confirm the diagnosis:
- in a general blood test - a decrease in hemoglobin level (with anemia, lack of absorption of nutrients);
- in a general urine test - an increase in the amount of calcium (with hyperparathyroidism);
- in biochemical analysis – hypoproteinemia (decreased amount of protein);
- in the coprogram - altered red blood cells (a sign of bleeding).
For gastrojejunal ulcers, a test is performed for Helicobacter pylori, a bacterium that provokes an inflammatory and erosive-ulcerative process in the stomach and intestines.