Anticholinergic drugs
Such medications have an antispasmodic effect, that is, the smooth muscles of the irritated part of the intestine will contract less frequently.
The most popular drugs in this group:
- Dicyclomine. The medicine helps relax the smooth muscles of the irritated intestines, but it does not affect the production of gastric juices. It takes effect a couple of hours after administration and the effect lasts for about four hours. They usually drink it four times a day before main meals and bedtime. There are situations when a patient, while taking Dicyclomine, suffers from dizziness, dry mouth, blurred vision, drowsiness, irritability and general weakness. Treatment with this drug is prohibited in case of individual intolerance to the components, bleeding, intestinal obstruction, etc. A complete list can be found in the instructions.
- Hyoscyamine. It helps reduce the volume of gastric juices, slows down peristalsis and relieves spasm from the smooth muscles of other organs. Take Hyoscyamine only on the recommendation of a doctor. Take the tablets half an hour before meals. You should not consume more than 1.5 mg per day. Side effects are similar to Dicyclomine. It is forbidden to drink Hyoscyamine if you have an individual intolerance, glaucoma, obstruction, or closure of the urinary tract.
The role of diet in the treatment of pathology
With this disease, compliance with the diet is more important than strict diet. Changes are needed towards the correct ratio of proteins, fats and carbohydrates. You should eat often, but little by little; overeating can make you feel worse.
The diet is selected depending on the type of syndrome. When experiencing flatulence, it is important to give up soda and legumes, or at least reduce their consumption to a minimum. If you have diarrhea, reduce the amount of dairy products, as well as fruits and vegetables in your diet; if you have constipation, you should eat less fatty and salty foods and drink more fluids.
The diet is selected strictly individually, in addition, even patients with an already selected diet must monitor their well-being and, if discomfort appears after something, it is better to refuse this food. A professional nutritionist can also help you select a diet.
Nutrition for irritable bowel syndrome should be balanced and varied so that the body receives all the necessary substances, but it is important to control the amount of food eaten to prevent overeating. It is better to eat little, but often, this will reduce the load on the digestive system. You should also ensure that meals occur at the same time every day; skipping them is highly discouraged.
Antidiarrheal drugs
The action of these drugs is aimed at slowing down the passage of food and suppressing the production of gastric juices. The most commonly prescribed medications are:
- Lomotil. A drug that helps reduce the frequency of bowel movements during diarrhea and slow down the contractions of the walls of the irritable intestine. The composition contains a substance that is similar in action to narcotic drugs to reduce pain, but it affects the irritable intestines to a greater extent. It also contains atropine, which reduces peristalsis and secretion of gastric juices. Adults first drink a couple of tablets four times a day, and then the amount is gradually reduced according to an individual scheme. Children under 13 years of age are prescribed syrup. Relief is usually observed within the first two days. Treatment with Lomotil sometimes causes side effects identical to those described above. Contraindications include allergies, obstructive jaundice, intestinal obstruction, diarrhea, and muscle weakness.
- Loperamide. This medicine, which slows down the contraction of the organ walls, makes the stool harder and relieves diarrhea, is most often prescribed for irritable bowel syndrome. Adults are usually prescribed a couple of tablets, and then the dosage is reduced by half. They drink them after every trip to the toilet. You should not drink more than 8 pcs per day. side effects are the same, but contraindications include allergies, bloody diarrhea, fever, infectious diarrhea and constipation.
Why does IBS occur?
There is no one universal reason why irritable bowel syndrome develops.
- Stress
It has been noted that pathology occurs with increased excitability of the nervous system against the background of chronic stress (therefore, young people and women are more likely to get sick). In this case, a vicious circle arises when an unfavorable emotional background causes intestinal irritation, and the disease itself drives the patient into depression, against the background of which other organs and systems begin to suffer. In some patients with IBS, when examined by a neuropsychiatrist, psychopathy and neuroses are revealed.
Doctors jokingly call IBS “irritable head syndrome,” because in addition to the main symptoms, there are often signs of a disorder in the autonomic and central nervous systems.
- Intestinal motility disorder
Also among the causes of the development of the syndrome, intestinal motility disorders and shifts in the transmission of nerve impulses to the intestinal muscles, which cause the intestines to contract, have been identified. In this case, there are no disturbances in the intestinal wall or in the nervous apparatus of the intestine, but there is a periodic deregulation of contractions and relaxations.
- Patients also have increased sensitivity to bowel overflow and distension. Pain sensitivity also increases.
- There is also some relationship with hormonal levels. Thus, in women, the last day of the cycle and the first days of menstruation can be combined with diarrhea and intestinal pain against the background of a temporary increase in prostaglandin E in the blood.
- Unusual, excessively fatty or high-calorie foods can also cause symptoms of intestinal distress. Among the drinks, alcohol, coffee, tea and sweet sodas have provoking properties.
- Hereditary predisposition is also not discounted: the syndrome is more often observed in people whose parents suffered from a similar disorder.
- Intestinal infections are a trigger for IBS in 30% of patients
- Dysbacteriosis and lack of ballast substances in the diet also lead to the development of irritable bowel syndrome.
Antidepressants
Often problems with the gastrointestinal tract arise against the background of nervous disorders, and this state of affairs is observed in 75% of 100% of cases. This group of medications helps reduce pain and fight depression. Irritable bowel syndrome should be treated after normalization of the emotional and psychological state.
Most often, the doctor prescribes Amitriptyline, which has an analgesic effect, increases the period of passage of food through the irritable intestines, reduces the frequency of stools and improves overall well-being. It is prescribed in a dosage of 10-50 mg once a day before bedtime.
Treatment with Amitriptyline cannot be carried out in case of individual intolerance, in the acute period of myocardial infarction, during breastfeeding and in case of glaucoma. It should not be given to children under 12 years of age. Some people, when taking the drug, experience constipation or, conversely, diarrhea, nausea, changes in appetite, rash and other abnormalities. It is prohibited to combine Amitriptyline and alcohol.
Irritable bowel syndrome: what it is and how to treat it
If your stomach starts to hurt, cramps, or diarrhea occurs before an important meeting or exam, then you most likely know what irritable bowel syndrome (IBS) is. Sometimes colloquially it is called “bear disease,” but the essence remains the same. This is a common problem characterized by short-term or relatively long-term episodes of digestive system disorders. IBS can manifest as stomach cramps with nausea and malaise, bloating, acute diarrhea just before an important meeting, or constipation before an exam.
It is estimated that 1 in 5 people will suffer from IBS at some point in their lives, and it usually develops between the ages of 20 and 30. Moreover, women more often experience this condition due to greater emotionality. The problem is usually lifelong; you will have to suffer with your stomach with every stress, although the condition may improve with age.
How does “bear disease” manifest itself?
Symptoms of IBS vary from person to person. One only experiences “butterflies in the stomach” before a date, while another suffers from severe diarrhea before a meeting with the boss or an exam. Manifestations tend to come and go at certain times in life when stress levels are elevated. The episodes of digestive “embarrassment” themselves can last from a few minutes or hours to several months with periods of relief or worsening. Often the intestines fail during times of stress or after eating certain foods. Some IBS symptoms disappear almost completely or are significantly reduced after going to the toilet and having a bowel movement.
The most common symptoms of IBS are:
- Abdominal pain and cramping, which can be relieved by having a bowel movement;
- changes in your toilet habits: the appearance of diarrhea or constipation, a combination of both problems at once;
- bloating and stomach cramps;
- excessive gas formation, flatulence in the most inappropriate places;
- urgent need to go to the toilet immediately;
- feeling like you haven't completely emptied your bowels after going to the toilet.
In addition to the main symptoms, some people with IBS experience a number of other problems. These may include:
- lack of energy and constant lethargy;
- constant feeling of “I’m getting sick”;
- back pain;
- Bladder problems such as having to wake up to urinate at night, an urgent need to urinate, and difficulty emptying the bladder completely;
- pain during sex (dyspareunia);
- urinary incontinence.
Of course, if this happens at home, you can solve the problem. However, if you need to go to work or study and it’s impossible to sit on the toilet for a long time, what should you do? What is the cause of this illness?
Why does the intestine suffer?
The exact cause of such intestinal confusion is unknown, but most experts believe that it is due to increased sensitivity of the intestines to stress and problems with digestion of food. This means you are more sensitive to pain and cramping coming from your intestines, and you may experience constipation or diarrhea because your food moves through your intestines either too slowly or too quickly. Psychological factors such as stress, grief, anxiety or depression may also play a role in bowel irritation. Many causes have been proposed, including inflammation, infections and certain diets, but none have led directly to IBS.
Your body normally moves food through your digestive system by rhythmically contracting and relaxing your intestinal muscles. However, in IBS, this process is altered, causing food to move through the digestive system too quickly or too slowly. If food moves through your digestive system faster than usual, it causes diarrhea because your digestive system does not have enough time to absorb water from food.
If food moves through your digestive system too slowly, it causes constipation because too much water is absorbed, making your stool hard and making it difficult to have bowel movements. It may be that food does not pass through the digestive systems of people with IBS properly because the signals that go from the brain to the gut are constantly interrupted.
It has been suggested that problems such as a deficiency of bile acids in bile, which is produced by the liver to digest fats, may be responsible for some cases of IBS.
Perhaps the reason is increased intestinal sensitivity. Many sensations in the body come from your digestive system. For example, nerves in your digestive system send signals to your brain so you know whether you're hungry or full when you need to go to the bathroom.
Some experts believe that people with IBS may be hypersensitive to signals from the digestive nerves. This means that mild stomach upset, which is barely noticeable in most people, leads to excruciating abdominal pain in patients with IBS.
Psychological factors of “bear disease”
There is also some evidence that psychological factors play an important role in IBS. However, this does not mean that IBS is “all in the head” because the symptoms are very real. Intense emotional states such as stress and anxiety can cause chemical changes that interfere with the normal functioning of the digestive system.
This doesn't just happen to people with IBS. Many people who have never had IBS before may suddenly change their bowel habits when faced with a stressful situation, such as an important exam or job interview.
Some people with IBS have experienced a traumatic event, usually in childhood, such as abuse, a serious childhood illness or bereavement. It's possible that these past turmoil may make you more sensitive to stress and symptoms of pain and discomfort.
IBS problem
IBS symptoms can also have a significant impact on a person's daily life and have a profound psychological impact. As a result, many people with this condition experience feelings of depression and anxiety. However, if you are suffering from bear disease, you need to see a doctor immediately if you experience:
- unexplained weight loss;
- swelling or lump in the abdomen or nodes in the anal area;
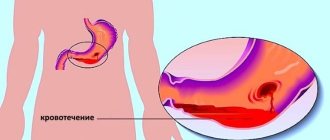
- bleeding from the rectum;
- signs of anemia.
Sometimes this can be a sign of a potentially more serious condition.
IBS triggers: what can be a provocateur?
Certain foods and drinks can trigger IBS symptoms. Triggers, of course, differ for each of us; among the leading ones we can highlight:
- alcohol
- carbonated drinks
- drinks containing caffeine such as tea, coffee or cola
- processed snacks – such as chips and cookies
- fatty or fried foods.
Keeping a food diary can be a useful way to identify possible triggers in your diet. Stress is another common trigger for IBS symptoms. Therefore, finding ways to cope with stressful situations is an important part of treating this disease.
It's also important to know that IBS does not pose a serious threat to your physical health and does not increase your chances of developing cancer or other bowel diseases.
Is it possible to cure bear syndrome?
Unfortunately, tablets or syrups that would cure IBS once and for all have not yet been invented, but the symptoms can be reduced or completely eliminated by changing your diet and lifestyle. For example, it may help:
- identifying and eliminating foods or drinks that trigger your symptoms;
- changing the amount of fiber in your diet;
- regular exercise;
- reducing stress levels.
Sometimes people with IBS are prescribed medications to treat specific symptoms they experience.
Unfortunately, the course of IBS is unpredictable. You can live and work for many months without any symptoms, and then suddenly develop diarrhea or constipation or stomach problems. The condition can be painful and distressing, which can have a negative impact on your quality of life and emotional well-being. Many people with IBS suffer from depression and anxiety, which in turn worsens bowel movements that are already irritated.
Talk to your doctor if anxiety has become a part of your life. He or she may recommend treatments such as antidepressants or cognitive behavioral therapy (CBT), which can help you manage your IBS as well as anxiety and signs of depression. With proper medical and psychological treatment, you can live a normal, fulfilling, and active life with IBS.
Nutrition correction
Changing your diet will play an important role in controlling your IBS symptoms. However, there is no one-size-fits-all diet for people with this condition. The foods that work best depend on your symptoms and how you react to different foods. It may be helpful to keep a food diary and record whether certain foods improve or worsen your symptoms. You can then avoid foods that are causing your symptoms. However, it's important to remember that these foods don't have to be avoided for life.
People with IBS are often advised to change the amount of fiber in their diet. There are 2 main types of fiber: soluble fiber (which dissolves in water) and insoluble fiber (which does not dissolve in water). Foods that contain soluble fiber include:
- oats
- barley
- rye
- fruits such as bananas and apples
- root vegetables such as carrots and potatoes
- flax seeds.
Foods that contain insoluble fiber include:
- whole grain bread
- bran
- flakes
- nuts and seeds (except flax seeds).
If you have diarrhea, reducing the amount of insoluble fiber you eat helps. It is important not to eat the skins, cores and seeds of fruits, berries and vegetables. If you have constipation, increasing the amount of soluble fiber in your diet and the amount of water you drink may help.
If you experience persistent or frequent bloating, a special diet called a low FODMAP diet may be effective.
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. These are types of carbohydrates that are difficult to break down and absorb in the intestines. This means that they begin to ferment in the intestines relatively quickly, and the gases released during this process can lead to bloating.
A low FODMAP diet essentially involves limiting the consumption of various high FODMAP foods, such as certain fruits and vegetables, animal milk, wheat products and beans.
General nutrition tips
Your IBS symptoms may also improve if you:
- eat regularly and take your time while eating
- Don’t skip meals or take long periods between meals
- drink at least eight cups of fluid per day – especially water and other decaffeinated drinks such as herbal tea
- limit your tea and coffee consumption to a maximum of three cups per day
- reduce the amount of alcoholic and carbonated drinks you drink
- Reduce your intake of indigestible starch (starch that resists digestion in the small intestine and reaches the colon), which is often found in processed or re-cooked foods
- Limit fresh fruit to three servings per day - half a grapefruit or an apple is a suitable serving.
If you have diarrhea, avoid sorbitol, an artificial sweetener found in sugar-free sweets, including gum and drinks, and some diabetic and weight-loss products.
If you have flatulence and bloating, oats and flax seeds (up to one tablespoon per day) may help.
Antibiotics
When treating irritable bowel syndrome, such drugs reduce the risk of bacterial overgrowth. The most commonly prescribed drug is Rifaximin, which is a semi-synthetic drug that inhibits protein synthesis in bacteria.
This remedy is usually prescribed for diarrhea, and the dosage is 550 mg every 8 hours. The course of treatment lasts two weeks. You should not take Rifaximin if you are hypersensitive, but the accompanying effects are flatulence, headache, nausea, constipation, abdominal pain, fever and rash.
Diagnostics
Diagnosis of the disease is difficult, because the gastrointestinal tract is usually normal. You should contact a gastroenterologist for help. He will refer you for various tests and studies. Irritable bowel syndrome is diagnosed as a diagnosis for those who have complaints, but all tests are in order. In addition, the frequency and severity of symptoms is important. So, in order to say that this is a disease, bowel dysfunction must occur at least three days a month, and the symptoms must last at least three months.
To identify the disease, studies such as:
- General blood analysis;
- Biochemistry analysis;
- Test for reaction to gluten;
- Stool analysis;
- Colonoscopy;
- Irrigoscopy;
- Esophagogastroduodenoscopy;
- Ultrasound of the abdominal cavity;
- Manometry;
- Electrogastroenterography;
- Rarely: biopsy of the intestinal wall.
Colonoscopy is a method for diagnosing irritable bowel syndrome with flatulence.
The symptoms of the disease are similar to various types of pathologies, so differential diagnosis is also important, which is carried out with such ailments as: anemia, dysbacteriosis, parasitic diseases, gastrointestinal infections, tumors, vitamin deficiencies, polyps, ulcerative colitis , Crohn's disease, intestinal tuberculosis.
Sometimes the diagnosis is repeated after the initial course of treatment to ensure its effectiveness.
Laxatives that increase stool volume
Such products contain substances that, when they enter the irritated intestines, swell, taking on a gel-like state, which facilitates the passage of food and stimulates peristalsis. With their help, you can cope with the symptoms of diarrhea and constipation.
For irritable bowels, Methylcellulose is most often prescribed, which has a mild laxative effect. Take two tablets up to six times a day. Contraindications include individual intolerance, intestinal obstruction, dysphagia, etc. As accompanying effects, flatulence occurs and the activity of the organ increases.
Functional bowel disorder code according to ICD 10
In patient medical histories, functional stomach disorder according to ICD 10 is encrypted as a separate nosological unit.
There is a single official document for medical institutions, in which all existing diseases are included and classified. This document is called the International Statistical Classification of Diseases, 10th revision, developed in 2007 by the World Health Organization.
This document is the basis for conducting statistics of morbidity and mortality among the population. Each medical history is coded according to the final diagnosis.
The FDF code according to ICD 10 belongs to class XI - “Diseases of the digestive organs” (K00-K93). This is a fairly extensive section in which each disease is considered separately. ICD 10 code for functional intestinal disorder: K31 - “Other diseases of the stomach and duodenum.”
What is FRF
Functional indigestion is the occurrence of pain, digestive disorders, motility, and secretion of gastric juice in the absence of any anatomical changes.
This is a kind of exclusion diagnosis. When all research methods do not reveal any organic disorders, and the patient has complaints, this diagnosis is determined.
Functional disorders include:
- Functional dyspepsia. which can manifest itself in different ways #8212; heaviness in the stomach, rapid satiety, discomfort, feeling of fullness, bloating. Nausea, vomiting, aversion to certain types of food, and belching may also occur. In this case, no changes in the gastrointestinal tract are detected.
- Swallowing air (aerophagy), which is then either regurgitated or absorbed into the intestinal tract.
- Functional pylorospasm - the stomach is spasmed, food does not pass into the duodenum and vomiting of eaten food develops.
For these complaints, an X-ray examination, ultrasound and FEGDS are required - however, no changes or disturbances are observed.
https://youtube.com/watch?v=qjAcrMbW8LM
Functional gastrointestinal disorders are treated symptomatically, since the exact cause of the disease is not known. Diet, enzyme preparations, antispasmodics, adsorbents, gastroprotectors, drugs that reduce stomach acidity and normalize motility are prescribed. Sedatives are often used.
Save the link, or share useful information on social media. networks
Intestinal colic
Intestinal colic is a rather painful spasmodic attack in the abdominal area. The concept of intestinal colic according to ICD 10 belongs to the class “Diseases of the digestive organs”.
Since colic is considered a symptomatic manifestation and is not an independent disease, its coding according to the international classification contains some features. Therefore, in ICD 10, the code for intestinal colic may have several options:
- If we mean a functional disorder without the presence of organic disorders, then the pathology will be coded “K 58” and have the name “Irritable Bowel Syndrome”.
- If there is a disorder of the digestive system in the form of acute obstruction, diarrhea or other pathology with the presence of such a symptom, then the disease is classified as “Other functional intestinal disorders” and encrypted “K 59”. This category has seven subcategories (“K 59.0” #8212; Constipation, “K 59.1” #8212; Functional diarrhea, “K 59.2” #8212; Neurogenic intestinal excitability, “K 59.3” #8212; Megacolon, “K 59.4” # 8212; Anal sphincter spasm", "K 59.4" #8212; Other specified functional intestinal disorders, "K 59.9" #8212; Unspecified functional intestinal disorder).
According to the ICD, intestinal colic refers to the underlying disease of which it is a manifestation, and therefore, when writing the final diagnosis, the coding and name of the underlying pathology are written.
Serotonin receptor antagonists
If irritable bowel syndrome is detected, then specialists from this group often recommend Alosetron. It is prescribed to women with IBS, which is accompanied by severe diarrhea. First, 0.5 mg is prescribed every 12 hours. The duration of treatment is 4 weeks, and then, if there are no side effects, the amount is increased to 1 mg.
Treatment with Alosetron is contraindicated in case of individual intolerance, bleeding, constipation, ischemic colitis and severe liver failure. When taking pills, you may experience constipation, abdominal pain, nausea, hemorrhoids, etc. A complete list is provided along with instructions.
Treatment
How and with what to treat irritable bowel syndrome? Treatment for IBS includes:
1. Drug treatment; 2. Diet; 3. Additional treatment.
1. Drug treatment (medicines for IBS)
Due to the fact that the exact cause of IBS is still being studied, drug treatment for this intestinal disorder is aimed primarily at relieving symptoms.
In this regard, a gastroenterologist usually prescribes the following medications for irritable bowel syndrome:
Antispasmodics. This group of medications is used to relieve pain in IBS, especially the appearance of spasms, which sometimes lead to a false urge to defecate.
Among the most popular antispasmodic drugs are No-shpa, Drotaverine, Duspatalin, and m-cholinergic receptor blockers (Buscopan).
Defoamers. This group of medications is used to reduce the production of gases in the gastrointestinal tract, which in turn leads to a reduction or complete prevention of bloating (flatulence).
Among the popular defoamers are “Meteospasmil”, “Espumizan”, “Polysilane”, “Zeolate”.
Antidiarrheals. This group of drugs is used to stop and prevent further occurrence of diarrhea. This step is also important, since frequent diarrhea leads to dehydration of the body with all the ensuing consequences, which can be read about in the article on dehydration.
Read also Vitiligo. Causes, symptoms, treatment of vitiligo
Antidiarrheal drugs include Imodium, Mezim Forte, Smecta, Microlax, Polisorb MP, and Eubicor.
To prevent constipation. For these purposes, laxatives are usually used, although not all of them in a row, otherwise there is a risk of transition from constipation to diarrhea, which is also an equally important problem. For IBS, it is best to use laxatives, the effect of which is to increase the production of feces, as well as increase the water content in them.
Among such drugs one can highlight Citrucel and Metamucil.
Please note that some laxatives cause increased gas formation, which leads to abdominal pain. Be careful.
Against dysbacteriosis. One of the pathogenic factors that can lead to the development of IBS is an imbalance of microflora in the gastrointestinal tract. Thus, in the digestive organs of a healthy person there are various types of bacteria (lacto, bifido), thanks to which the process of normal digestion and assimilation of food occurs. In some cases, for example, with the uncontrolled use of certain antibiotics and other drugs, the balance of bacteria is disturbed - along with pathogenic bacteria, the antibiotic also kills beneficial bacteria. This leads to disruption of normal digestion and, accordingly, a number of gastrointestinal diseases.
For the treatment of dysbiosis the following are used:
Probiotics (Linex, Enterol, Bifikol, Lactobacterin) are preparations that contain ready-to-use gastrointestinal bacteria - bifidobacteria, lactobacilli and others.
Prebiotics (Hilak-Forte, Normaza, Duphalac) are drugs that are not absorbed or fermented by the gastrointestinal tract, but are a nutrient medium for beneficial microflora, which leads to an increase in their numbers.
To normalize the functioning of the nervous system. To correct the functioning of the nervous system, sedatives, antidepressants and tranquilizers are used. However, the choice of drug is made purely on the basis of diagnosis, otherwise there is a risk of worsening IBS, including increased depression in combination with a functional disorder of the intestines and other gastrointestinal organs.
The simplest group is sedative medicines based on motherwort, valerian, and lemon balm.
Among antidepressants, drugs of the tricyclic group (Amitriptyline) and serotonin reuptake inhibitors (Fluoxetine) have shown the greatest effectiveness against IBS.
Diet for irritable bowel syndrome
Diet for IBS is almost the main point in the treatment of this disorder. After all, it is unbalanced and poor-quality nutrition that in most cases contributes to disruption of the functioning of the gastrointestinal tract.
Basic nutrition rules: regular meals, small portions, no overeating, drinking plenty of water.
Food products are selected individually, depending on the accompanying symptoms.
It is recommended to avoid eating foods such as peas, beans, cabbage, potatoes, grapes, milk, kvass, soda, sorbitol-containing foods, alcohol, fatty and heavy-for-the-stomach foods. Also reduce the daily consumption of fresh vegetables and fruits.
For IBS with diarrhea, it is recommended to eat soup with low-fat broth, lean meats and fish, rice or semolina with water, dried bread, strong tea, jelly with a berry-fruit base.
For IBS with constipation, it is recommended to eat buckwheat and oatmeal, black bread, vegetables, fruits, freshly squeezed juices and purees with pulp, prunes, senna leaves, vegetable oil. There are no recommendations for a complete ban on certain products.
Read also Peritonitis - symptoms, causes, types and treatment of peritonitis
Additional treatments
- Physical activity - daily exercises, exercise therapy, daily walks in the fresh air, gym, swimming;
- Normalization of the daily schedule of work, rest and sleep, you need to get enough sleep;
- Correction of mental health with a psychotherapist;
- Spa treatment, drinking mineral waters;
- Physiotherapeutic procedures.
Chloride channel activators
Treatment with these drugs is aimed at increasing the volume of fluid in the intestines, which promotes emptying, so they are prescribed for constipation. In this group, it is worth paying attention to Lubiprostone, which is prescribed to women who are over 18 years old.
Take 8 mcg every 8 hours. You should not drink it if you have an individual intolerance to the components of the product or mechanical obstruction. Some people experience nausea, vomiting, swelling, fatigue, etc. when taking Lubiprostone.
What is intestinal colic? Reasons for appearance
Intestinal colic, ICD code 10 – K59
, belongs to diseases of the digestive system. It is characterized by paroxysmal pain in the abdominal area, which can go away on its own. Despite the wave-like nature of the attacks, colic can signal serious diseases of the digestive tract (gastritis, ulcers).
Coding of intestinal colic according to ICD 10
Intestinal colic is not an independent pathology, but a symptom of indigestion.
In accordance with ICD 10, intestinal colic is considered as an addition to the main pathology; when writing a diagnosis, the encoding of intestinal colic and the name of the main disease are used.
Functional gastrointestinal disorder
By “functional disorder of the stomach and intestines” we mean a number of disorders of the gastrointestinal tract that are not associated with changes in the structure of the digestive organs. FGIT (functional disorder of the gastrointestinal tract) is characterized by the presence of:
- Functional bloating.
- Functional constipation.
- Diarrhea.
- Irritable colon or small intestine syndrome (gastrointestinal dysfunction).
FRF appears due to:
- Hereditary predisposition.
- Mental instability (severe stress, constant worries).
- Heavy physical work.
- Infectious diseases of the gastrointestinal tract.
FGIT is spoken of when its symptoms have bothered the patient for 6 months or more. Moreover, symptoms must actively manifest within 3 months.
_____________________________________________________________________________________
The NetGastritu project was created with the goal of providing people with accurate and up-to-date information on medical topics. Articles are written by professionals and, unfortunately, development costs slow down the development of the project. If you want to support us, use the form below.
Let's make the world a better place together
Thank you for your attention
_____________________________________________________________________________________
What causes intestinal colic?
Colic is a consequence of irritation of the intestinal walls by a provoking factor. G
The smooth muscles respond to this with a strong contraction (spasm). Intense physical activity can trigger colic. During this, tension in the mesentery occurs, which leads to stabbing pain in the left side of the abdomen.
Colic occurs due to:
- Immaturity of gastrointestinal tract structures, flora insufficiency (in children).
- Eating heavy foods that contribute to the formation of gases (flour products, fried foods, soda).
- Exposure to large amounts of air when eating. This can happen if you talk during a meal or eat on the go.
- Constipation.
- Entry of a foreign body into the gastrointestinal tract.
- Food allergy (to lactose).
- Allergic reactions.
- Disorders of blood supply to various parts of the intestine. This occurs due to ulcerative formations and diverticulosis.
- Intestinal obstruction.
Symptoms of colic in adults
The pathological condition is characterized by pain in the abdomen with tingling. The localization of painful sensations is different, because spasms gradually move from one part of the intestine to another. Pain syndrome is accompanied by:
- Nausea.
- The urge to vomit.
- Increased gas formation.
- Bloating.
To ease the attack, the person takes a position that helps reduce pain - leaning forward with the body.
Manifestation of colic in children, their causes
In an infant, intestinal colic is a widespread phenomenon. It often occurs in 1-4 months of a baby’s life. A child reacts to the appearance of colic as follows:
- Facial hyperemia.
- Constant screaming and anxiety.
- Pressing your knees towards your stomach.
The baby's tummy is tense. Its palpation brings painful sensations to the little patient. The attacks occur at certain hours at night and recur within a week or two.
In children under 4 months of age, colic is not a pathology, but a consequence of enzymatic disorders. Its symptoms are observed in children, both bottle-fed and natural-fed.
The cause of discomfort in the intestinal area may be:
- Infection.
- Allergy to dairy products or breast milk.
- Inflammation.
- Psychogenic factor (tense family situation, mother's depression).