What is a stress ulcer of the stomach and duodenum?
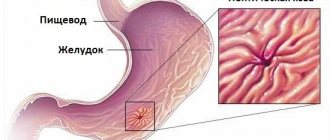
Stress gastroduodenal ulcers, characterized by a deeply penetrating violation of the integrity of the mucous membranes of the stomach and duodenum, are the result of severe injuries and serious somatic diseases that have a powerful effect on all systems of the human body.
Being, as a rule, multiple, stress ulcers very often occur in patients undergoing intensive care or resuscitation, since their stomach is the first to take on the effects of negative factors.
The most serious complication of stress ulcers is bleeding that develops in the upper gastrointestinal tract. Thus, of 60% of patients who were on artificial ventilation for a long time, bleeding was recorded in 25% of cases.
The problem of correct approaches to the prevention and treatment of this pathology, due to the high level of deaths, continues to be relevant to this day for resuscitators, surgeons and gastroenterologists.
The first to prove the existence of a connection between the severity of the underlying disease and bleeding from the upper gastrointestinal tract was the American cardiologist Harold Jeremy Swan.
In 1936, Canadian endocrinologist and pathologist Hans Selye proposed the term “stress ulcer” to denote the connection between severe somatic illness and the occurrence of ulcerated lesions in the mucous membranes of the stomach and duodenum.
Before him, stress ulcers were classified as primary pathologies, not considered a consequence of ischemia of the gastroduodenal mucosa. This gave rise to an erroneous approach to treatment tactics that gave unsatisfactory results.
Data on the incidence of gastroduodenal stress ulcers in the medical literature differ significantly.
Thus, the number of Curling ulcers observed in patients with widespread burns ranges from 12-75% of cases, and Cushing ulcers occurring in patients with traumatic brain injuries and patients who have undergone neurosurgical surgery - in 13-15% of episodes.
Such a striking contrast is probably explained by the complete asymptomatic nature of the pathology, which is often discovered only after autopsy.
Complications
Serious complications are rare, but there are a few you should be aware of.
Some mouth ulcers are actually a type of oral cancer. Ulcers and sores that do not heal even after treatment and appear on the tongue, between the cheek and gum, or under the tongue may be a sign of oral cancer.
Untreated or stomach ulcers can in some cases cause the following serious symptoms:
- loss of appetite and weight loss;
- labored breathing;
- dizziness;
- vomit;
- nausea;
- black tarry stools;
- internal bleeding;
- gastric obstruction.
Stomach and duodenal ulcers
A stress ulcer is most likely to develop when you are already under medical care for a serious illness, surgery, or injury or bruise. The presence of a stress ulcer adds further complications to other diseases. As with stomach ulcers, the most serious complications are internal bleeding and obstruction.
Reasons for development
Stress ulcers are an example of functional disorders, the impetus for which is stressful situations that activate the activity of the hypothalamus (a small area of the diencephalon), leading to inflammation of the gastroduodenal mucosa.
Under the influence of stress, the structures of the hypothalamus begin to produce excess amounts of corticosteroid hormones, which negatively affect the properties and volume of protective mucus produced by the cells of the stomach. The consequence of this process is damage and poor restoration of gastroduodenal epithelial tissues.
Ulcers caused by stress are often called pseudoulcers.
Stress ulcers can occur in patients:
- those who have suffered serious injury to internal organs;
- suffering from acute renal or liver failure;
- those in a terminal state (for example, in collapse caused by cardiovascular failure), accompanied by loss of consciousness and posing a threat to life;
- have undergone complex surgery;
- suffering from diseases of the abdominal cavity or gastrointestinal tract that occur in an acute form.
The simultaneous confluence of several stressful situations exacerbates the risk of pathology, since in this case all systems and internal organs of the human body begin to work to the limit of their capabilities, provoking the production of huge amounts of catecholamines and corticosteroids.
It has been established that the development of the inflammatory process in the stomach begins within two to three hours after exposure to stress, and the occurrence of bleeding erosions can be observed three days later.
Stress can provoke an exacerbation of peptic ulcer disease due to a significant deterioration in blood microcirculation in the muscle tissues of the stomach, which entails ischemia of its mucous membranes.
Increased production of gastrin (a hormone produced by cells located in the pyloric part of the stomach) leads to the fact that the main digestive organ begins to secrete too much gastric juice.
Stress ulcers that affect gastric motility significantly complicate the transport of food into the intestines, while the absorption of amino acids into the blood also worsens.
Curlinga (Curling) ulcers.
Acute ulcers of the alimentary canal, developing as a complication of burn disease. Ulcers can be either single or multiple. Most often localized in the stomach and duodenum, less often in the intestines. Bleeding and perforation of ulcers are observed, but more often they are asymptomatic.
Cushing's ulcer.
One or more ulcers of the digestive canal (usually in the lower esophagus or stomach), formed under the influence of stress. In their
In addition to the occurrence of ischemia of the wall of the stomach or esophagus, certain importance is attached to steroids, alcohols, aspirin, which increase the permeability of the mucous membrane to hydrogen ions, disrupt its barrier function with the formation of ulcers prone to rapid perforation.
Lambling syndrome.
Extreme emaciation, anemia, edema, diarrhea, hypothermia after gastrectomy.
Lengof.
Retraction under the right costal arch during a deep breath in liver echinococcosis.
Leotta.
The appearance of pain when pulling and displacing the skin fold of the abdomen in the presence of adhesions.
Lepera.
Oxalemic diathesis with damage to the intestines and urinary tract: chronic dyspepsia, flatulence after meals, colon spasms, liver enlargement, biliary dyskinesia, cholelithiasis, pancreatic insufficiency, intolerance to eggs, rice, spinach, etc. oxaluric renal colic. There may be dolichocolon and diverticulosis of the colon.
Lüthi-Sord-Bütler syndrome.
Manifested by enlarged mesenteric lymph nodes, iron deficiency anemia, hypoalbuminemia, increased levels of alkaline phosphatase, ESR.
Mac Fedden.
Pain at the outer edge of the right rectus abdominis muscle with mesadenitis.
Maskhof's disease.
Reticulocytic mesadenitis - abdominal pain increases over 7-10 days, most often in the right lateral region. The abdomen is moderately painful, not tense. An infiltrate is palpable in the area of the cecum. There are no chills or vomiting. The temperature increased to 39 degrees. The causative agent is presumably pseudotuberculosis pasteurella.
Mayer's triad.
Intestinal colic with bloody diarrhea, polyneuritis and polymyositis with periarteritis nodosa.
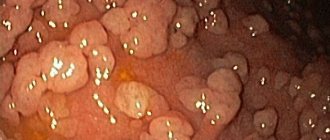
Menetrie's disease.
Tumor-like gastritis: excessive growth of the gastric mucosa along the greater curvature in the sinus area, often with prolapse through the pylorus into the duodenum. Clinic: feeling of pressure, spasm and pain in the epigastric region, heartburn, bloating, lack of appetite, weight loss, vomiting, sometimes with blood. There may be black stool, swelling of the hands and feet. Hypoproteinemia, decreased acidity of gastric juice. Local and diffuse thickening of the folds of the mucosa, which may be uneven, deformed, sometimes with jagged contours. There are warty and papillary growths.
Monprofi is the bomb.
A closed space located between the sutured duodenal stump and the intestinal stricture located more aborally. In this space, an abscess may form with a breakthrough into the abdominal cavity.
Moore's syndrome.
Abdominal epilepsy: irregularly recurring attacks of acute abdominal pain, accompanied by vomiting and diarrhea. May cause prostration and convulsions. EEG shows damage to the cerebral cortex, especially the frontal lobes. Attacks occur for several years.
Marleya.
Tenesmus and a feeling of fullness in the rectum with simultaneous pain in the lower limb when the pelvic veins are involved in the thrombophlebitic process.
Obraztsova.
Loud rumbling upon palpation of the cecum with enteritis.
Oppel diabetes.
Accompanied by acidosis in patients with surgical diseases during forced fasting after surgery and in exhausted patients.
Ortner's syndrome.
Abdominal tonsillitis: paroxysmal abdominal pain, vomiting, bloating, shortness of breath. Develops in old age as a result of impaired mesenteric circulation.
Patella disease.
Pyloric stenosis in tuberculosis.
Peutz-Jeghers syndrome.
A combination of intestinal polyposis with pigmentation of the skin and mucous membranes in the lips, mouth, nasal folds, and eyelids.
Petrovsky.
Compression of the mediastinum that appears after eating due to stretching of the esophagus during cardiospasm.
Potena syndrome.
Reflex disturbance of hemodynamics in the pulmonary circulation due to severe pain syndrome in diseases of the stomach and biliary tract.
Rapunzel syndrome.
In a number of mental illnesses, patients can swallow hair, which forms a trichobezoar that can cause obstruction.
Roemheld syndrome.
Gastrocardiac syndrome.
Senhouse-Kirks syndrome.
Shock syndrome: azotemia, nausea, vomiting, diarrhea, hypothermia, convulsions, tachycardia, arrhythmia, acrocyanosis, hemorrhage, coma. Observed in case of hemorrhage in the adrenal glands or in case of toxic-allergic damage.
Trevsa zones.
The area of the small intestine between the 1st and 3rd vascular arcades and in the terminal ileum, at the point where it enters the cecum, has a weaker blood supply compared to other parts.
Turko syndrome.
Poloiposis of the colon in combination with a tumor of the central nervous system,
Waterhouse-Friderichsen syndrome.
Fulminant meningococcal sepsis, adrenal apoplexy. Develops acutely. Suddenly there is a sharp headache, abdominal pain, vomiting, diarrhea, fever, cyanosis, followed by pallor. There is no shortness of breath. After a few hours, petechiae and bruising appear. Blood pressure drops sharply. Collapse, coma, delirium, and convulsions develop. Children get sick more often. The cause is an acute (usually meningococcal) infection, damage to the adrenal cortex. Death occurs as a result of acute adrenal insufficiency.
Fitz-Hugh syndrome.
Gonococcal peritonitis of the upper half of the abdominal cavity.
Schmiden's disease.
Hypertrophic pyloric stenosis due to prolapse of the mucosa.
Schmidt.
Edema of the lower extremities in the absence of organic changes in the heart and kidneys with sarcoma of the small intestine.
Stirlina.
The terminal section of the ileum is in the form of a clearly shaped chain. Determined in Crohn's disease.
MEDIASTINITIS .
Birenbaum.
Increased pain sensitivity on palpation of the abdominal aorta.
Ignatovsky.
Parasternal pulsation.
Filosofova.
The “thicket” symptom is a percussion-determined expansion of the boundaries of the mediastinum.
SPICY.
Gehrke.
In the presence of anterior mediastinitis, tilting the head back causes increased pain under the sternum.
Ravich-Scherbo.
Jugular: retraction of the jugular cavity during inspiration with anterior
mediastinitis.
Paravertebral: retraction of intercostal spaces paravertebral with
posterior mediastinitis.
Steinberg.
The appearance of rigidity of the cervical muscles with posterior mediastinitis.
Riddinger.
Substernal pain when swallowing and breathing with posterior mediastinitis.
Romanova.
Retrosternal or interscapular pain, aggravated by swallowing and throwing back the head in acute mediastinitis due to rupture of the esophagus.
BREAST.
Benzadone.
Retraction of the nipple of the mammary gland when squeezing it with two fingers and simultaneously pulling the palpable tumor inward with the fingers of the other hand in case of breast cancer.
Davydova.
Redness and swelling of the skin of the breast after lubrication with an alcohol solution of iodine for breast tuberculosis.
Gilbert's syndrome.
Gynecomastia, massive metastases to internal organs, most often the lungs, with a testicular tumor.
Krause.
Thickening of the nipple and areola due to breast cancer.
Cooper syndrome.
Mastodynia: pain in one or both mammary glands without local changes. Observed in young nervous women, occasionally in men.
Paget's disease.
Eczema-like cancer of the nipple of the breast. Stages: 1 - thickening of the nipple; 2 - ulceration; 3 - regional metastases.
Pribram.
When you pull on the nipple, the cancerous tumor moves along with it.
I advertise a disease.
Multiple breast cysts. Often bilateral.
Sorgius.
Sorgius node: in breast cancer, a lymph node the size of a pea to a hazelnut is palpated at the outer edge of the pectoralis major muscle.
Varieties
Stress gastroduodenal ulcers are usually divided into:
- Curling's ulcers;
- Cushing's ulcers;
- ulcerative defects of the mucous membranes caused by myocardial infarction;
- post-traumatic erosions of the gastric mucosa.
Kurlinga
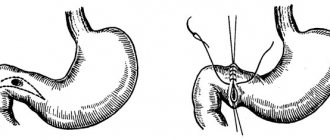
Curling's ulcer, which affects the mucous membrane exclusively of the duodenum, develops as a result of extensive trauma (most often burns) covering most of the body.
At the same time, the blood volume in the patient’s body (including the skin and organs of the gastrointestinal tract) is significantly reduced.
It is this factor that becomes the trigger that gives impetus to the emergence of pseudoulcers.
Cushing
The main factor provoking the formation of a Cushing's ulcer is an acute cerebrovascular accident or significant damage to brain structures, observed during strokes or traumatic brain injuries.
Cushing's ulcer, a common complication of brain surgery, can affect the mucous membranes lining the walls of the stomach, duodenum, and esophageal tube.
This type of pseudoulcer, which is usually not accompanied by clinically significant symptoms, can provoke:
- the occurrence of bleeding;
- perforation of the walls of the intestines and stomach;
- development of sepsis and peritonitis.
Common causes and recurrence of ulcers
Causes mouth ulcers:
- viral infection;
- biting or damaging the lips, tongue, and inside of the cheek;
- changes in hormone levels in women;
- stress;
- some products;
- some medical diseases.
Causes of stomach ulcers may include:
- Helicobacter infection;
- NSAIDs, including Aspirin, Ibuprofen, Naproxen and other medications for severe stress, depression and some other mental illnesses possibly related to the brain.
Some physical factors that can cause ulcers are:
- some surgical procedures;
- severe burns;
- brain injuries;
- traumatic injuries to the body;
- serious injuries, usually requiring hospitalization or intensive care;
- injuries of the central nervous system.
Symptoms
The main danger of pseudoulcers is the absolute asymptomatic nature of their clinical course.
The symptoms of stress ulcers are very often covered up by the clinical picture of the underlying pathology. A distinctive feature of this type of ulcerative lesion of the gastrointestinal tract from ulcers of other etiologies is the complete absence of pain.
The first signs of pathology, caused by the influence of irritating factors on the surface of enlarged ulcerative lesions, make themselves known:
- the appearance of severe pain in the stomach or lower abdomen (this depends on the location of the pseudoulcer);
- brown coloration of vomit due to the admixture of blood;
- the occurrence of dizziness;
- loss of consciousness;
- black stool.
The admixture of blood in the vomit and the dark color of the stool are extremely alarming symptoms, indicating bleeding and the likelihood of perforation, which can lead to the development of peritonitis.
Their appearance is an indication to immediately seek qualified medical help, since delay can be fatal.
According to medical statistics, gastroduodenal bleeding caused by stress ulcers is observed in 25% of patients treated in the intensive care unit, and in 5% of cases, blood loss poses a serious threat to the patient’s life.
However, experts are confident that these data are greatly underestimated. The fact is that stress ulcers, which in the vast majority of cases are shallow, are accompanied by hidden bleeding that does not lead to clinically significant manifestations. They can only be identified during a targeted diagnostic examination.
Intense bleeding is accompanied by:
- the occurrence of severe general weakness;
- rapid heartbeat (tachycardia);
- drop in blood pressure;
- pale skin;
- vomiting scarlet blood.
Forecast
For stress ulcers, the prognosis is largely favorable. However, the prognosis directly depends on how severely the stomach and its mucous membrane were affected, the amount of blood loss, and the duration of the disease. Stress ulcers rarely become the subject of surgical intervention; usually everything is limited to medications. With proper nutrition and the absence of stressful situations, relapse is extremely rare. If there was no heavy bleeding, the ulcers will heal quickly.
But it is worth remembering that with heavy gastrointestinal bleeding, the mortality rate can be 80%. For this reason, patients who are in the intensive care unit or intensive care unit are given appropriate prophylaxis, since the risk of developing a stress ulcer against the background of other diseases is extremely high.
Diagnosis of pathology
The initial stage of diagnosing stress-induced ulcers is:
- collection and assessment of anamnesis;
- physical examination of the patient;
- palpation of the abdominal cavity.
Based on the data obtained, the doctor makes a preliminary diagnosis that requires confirmation (instrumental and laboratory).
The set of laboratory tests includes:
- General and biochemical blood tests. The change in blood characteristics is very indicative. During the first hours after bleeding, they will indicate a high platelet count and accelerated blood clotting. By the end of the second or third day, the concentration of hemoglobin and red blood cells will be significantly reduced.
- Analysis of feces for occult blood.
- Analysis of gastric contents for occult blood, helping to prevent false negative results due to low pH levels.
The most informative instrumental methods for identifying stress ulcers are:
- The procedure of esophagogastroduodenoscopy (EGD), which allows to detect the presence of ulcerative lesions of the mucous membranes of the stomach and the bulbar part of the duodenum. The study is carried out only if the patient does not have severe pain or bleeding.
- Contrast radiography is a safe and painless procedure that can be used to determine not only the number of erosions, but also the degree of damage to the mucous membranes.
Ulcers due to hyperparathyroidism
Hyperparathyroidism is a disease caused by pathological hyperproduction of parathyroid hormone by the parathyroid glands.
Gastroduodenal ulcers in hyperparathyroidism occur with a frequency of 8-11.5%. The mechanism of ulcer formation is as follows:
- excess parathyroid hormone has a damaging effect on the mucous membrane of the gastroduodenal zone and stimulates gastric secretion and the formation of hydrochloric acid;
- hypercalcemia stimulates the secretion of hydrochloric acid and gastrin;
- with hyperparathyroidism, the trophism of the mucous membrane of the gastroduodenal zone sharply decreases.
Clinical features of the course of gastroduodenal ulcers in hyperparathyroidism:
- ulcers are most often localized in the duodenum;
- ulcers have an atypical course for a long time;
- clinically manifest forms are characterized by severe pain, persistence, resistance to antiulcer therapy, and a tendency to complications (bleeding, perforation);
- Frequent recurrence of ulcers is typical.
FEGDS and fluoroscopy of the stomach reveal an ulcer, characterized by the same endoscopic and radiological manifestations as a regular peptic ulcer.
The clinical picture and diagnosis of hyperparathyroidism are described in the corresponding chapter of the manual “Diagnostics of diseases of internal organs”.
Treatment methods
The main goal of treating stress ulcers is to relieve (eliminate) the causes that provoked their occurrence, as well as to prevent possible complications.
Drug therapy for stress ulcers should primarily be aimed at activating the body’s protective functions, restoring the functioning of the immune and nervous systems, as well as all types of metabolic processes.
The treatment regimen includes medications that help reduce the secretion of gastric juice and restore blood supply to organs located in the upper gastrointestinal tract.
The main medications used to treat stress-induced ulcers are represented by the following drugs:
- "Pantoprazole."
- "Dobutamine."
- "Misoprostol."
- "Omeprazole."
- "Somatostatin".
- "Sucralfate."
If gastric bleeding occurs, the patient undergoes a surgical operation, during which laser coagulation (cauterization) of the bleeding vessels and surgical suturing of ulcerative formations are performed.
An important factor in the successful treatment of stress ulcers is adherence to a special diet, which the patient will have to adhere to for the rest of his life (to avoid the formation of new erosions).
The basic principles of a therapeutic diet are:
- By excluding from the daily diet foods that promote increased synthesis of hydrochloric acid: fatty, salty, fried foods, coffee, alcoholic and carbonated drinks.
- It is mandatory to consume cereals, fish and lean meats, sweet fruits, thermally processed vegetables, non-sour and low-fat dairy products.
- In compliance with separate and fractional meals (small portions at equal intervals), requiring the need for dinner, taken at least two hours before departure for the night's rest.
- Significantly limiting salt and drinking two liters of clean drinking water per day.
Prognosis and Prevention
The prognosis for symptomatic ulcers is determined by the course and outcome of the underlying disease, the development of complications such as bleeding or perforation.
Prevention consists of careful administration of drugs that have an ulcerogenic effect (if it is impossible to replace them with other drugs) and the simultaneous administration of antacids (see). When patients with diseases of internal organs and systems develop dyspeptic disorders or pain in the epigastric region, they are prescribed diet No. 1 (see Medical nutrition), antacids and anticholinergic drugs (see Anticholinergic substances).