Standards and course of treatment of pancreatitis in hospital
Treatment of pancreatitis in a hospital is indicated in cases where an acute form of the disease is diagnosed. Due to the high probability of disability as a result of severe pathological changes in the pancreas and the increased risk of death, the patient is hospitalized at the first signs of an acute attack. Further therapeutic tactics are determined by the person’s condition. The decision on the advisability of surgical intervention or a course of intensive therapy is made by the doctor based on the results of the preliminary examination.
In order to stabilize the condition of patients with severe pain accompanying an acute attack of pancreatitis, 2 types of treatment measures are selected - emergency surgical care or intensive conservative therapy. Preference is given to drug treatment methods; surgery is prescribed strictly according to indications when the development of pancreatitis threatens the patient’s life.
Surgical therapy
In most cases, patients with an acute attack of pancreatitis are admitted to the hospital with swelling or necrosis of the pancreas. Surgery is recommended by doctors in 30% of cases, at the stage when inflammation of the pancreas causes extensive tissue necrosis. The operation is performed in several formats, determined by the severity, etiology of the pathological process and the degree of its spread to other organs of the abdominal cavity:
- for non-infectious forms of necrosis, laparoscopy is indicated;
- in case of enzymatic peritonitis, puncture-drainage intervention is prescribed;
- in case of extensive internal inflammation with the formation of multiple ulcers, infection of true and false cysts, widespread pancreatic necrosis, phlegmon or peritonitis, laparotomy is performed.
If minimally invasive manipulations in a hospital setting in combination with taking medications do not produce the expected result, more large-scale surgical interventions are undertaken - distal or subtotal resection of the pancreas, necrosequestrectomy (removal of contents from fluid formations inside the pancreas).
Intensive conservative therapy
In case of moderate condition of the patient, relief of the attack is carried out in the intensive care unit. In the early stages of the disease, to stop the pathological process and prevent destruction of the pancreas, a complex of inpatient conservative treatment is prescribed, including:
- measures to reduce the activity of the affected organ (fasting, gastric lavage using a thin tube, intravenous or intramuscular administration of medications that reduce the acidity of gastric juice);
- reduction of intoxication caused by excess pancreatic enzymes (intravenous administration of agents to regulate the secretory function of the organ - aminocaproic acid, Gordox, Contrikal);
- analgesic therapy (analgesic drugs during exacerbation of pathology are combined with myotropic antispasmodics);
- antibiotic therapy (Tienam is the drug of choice; combinations of other antibiotics are also used, which are administered by infusion);
- correction of vascular insufficiency (intravenous drip administration of solutions of hormones, adrenaline, norepinephrine or dopamine);
- restoration of water and electrolyte balance (using droppers with sodium chloride or glucose solution).
Treatment of patients with acute pancreatitis
The acute form of the disease can last several weeks. To relieve pain in acute pancreatitis, targeted medications are prescribed, including:
- cytostatics;
- antispasmodics;
- analgesics;
- anticholinergics;
- blockers of pancreatic enzyme production;
- antibiotics (if the inflammatory process is accompanied by suppuration);
- electrolyte solutions for blood purification during intoxication.
It is important to identify particularly dangerous forms of the disease. Thus, the incidence of purulent-necrotic parapancreatitis reaches 10% of all cases of the disease. Early detection of severe pancreatitis can speed up the recovery and stabilize the patient’s general condition several times, and in some cases even save his life.
Urgent Care
The treatment protocol for adults and children with pancreatitis is drawn up strictly individually, taking into account the patient’s age, weight, blood pressure, results of laboratory and instrumental studies.
First aid for severe acute forms consists of intravenous administration of narcotic painkillers through droppers, ensuring rest and relieving inflammation of the pancreas.
Medicines
Medicines are prescribed to eliminate pain, dyspeptic disorders, manifestations of exocrine or intrasecretory organ failure, and eliminate foci of acute inflammation in the organ itself and in nearby tissues. The course of therapy is selected strictly individually.
Diet
To suppress the production of pancreatic enzymes, the patient is recommended to eat a diet with natural inhibitors. Patients are allowed dietary varieties of meat, fish, vegetable soups, light broths, low-fat dairy and fermented milk products, fresh fruits, vegetables, cereals boiled in water, rosehip decoction, honey, yesterday's bread.
It is necessary to exclude from the diet fresh baked goods, fatty fish and meats, smoked foods, spicy dishes and seasonings, carbonated drinks, rich broths, eggs, legumes, tomatoes, chocolate, coffee, strong tea.
Operation
The surgical protocol for pancreatitis involves the most gentle impact directly on the gland only as a last resort, when conservative measures are ineffective. Most often, intervention is performed to remove (drainage) effusion from the omental bursa.
The doctor observes the surgical site through a special probe.
The operation is carried out using laparoscopy - manipulation with special instruments through pinhole punctures in the tissues. This method allows for minimal invasiveness and leaves almost no marks on the skin.
Standards and course of treatment of pancreatitis in hospital
In case of acute inflammation of the pancreas, the patient must be hospitalized. Treatment of pancreatitis in a hospital is necessary, since due to severe pathological changes in the affected organ there is a high risk of disability or death.
An acute attack of pancreatitis with severe pain can be treated with 2 options for medical care:
- Emergency surgery.
- Intensive drug therapy.
The decision on the appropriateness of a particular treatment tactic is made by a gastroenterologist. Conservative therapy is most often prescribed. Surgical intervention is considered necessary if the severity of the disease threatens the patient’s life.
Surgical therapy
Many patients are hospitalized in critical condition, which is caused by either extensive edema or a necrotic process in the pancreas. According to medical statistics, surgical intervention is prescribed for every third patient with death of organ tissue. The choice of surgical treatment method is determined by the cause of acute pancreatitis, the severity of the disease, and the presence of spread of the inflammatory process to adjacent organs of the abdominal cavity.
Most often practiced:
- Puncture and drainage is a minimally invasive intervention to remove effusion in the development of enzymatic peritonitis.
- Laparoscopy is also a minimally traumatic method used for non-infectious necrosis. It is used to excise dead areas of the gland, drainage pseudocysts, and eliminate neoplasms.
- Laparotomy - opening of the abdominal cavity with multiple infected cysts, phlegmon, peritonitis.
Minimally invasive methods are often used in preparation for laparotomy. If such interventions, together with taking medications, do not lead to the desired result, surgeons resort to radical operations. They are carried out under the control of X-ray and ultrasound machines. This:
- Necrosequestrectomy - puncture of cystic neoplasms, pumping out fluid from them and installing drainage.
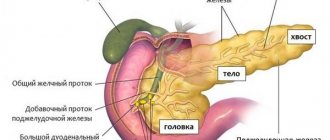
- Distal or subtotal resection. In the first case, the tail and body of the gland are removed, in the second - almost the entire affected organ, with the exception of areas adjacent to the duodenum.
Intensive conservative therapy
If the patient is admitted in a state of moderate severity, the attack is treated in the intensive care unit of the hospital. In order to eliminate the inflammatory process and prevent necrosis of the gland, temporary fasting, gastric lavage and complex drug treatment are prescribed.
The following groups of drugs are used:
- painkillers for exacerbation of pathology simultaneously with antispasmodics: Ketorol, No-shpa;
- medications that reduce gastric acidity: Almagel, Gaviscon, Omeprazole, Ranitidine;
- means for regulating the secretory function of the gland: Gordox, Aminocaproic acid, Contrical (intravenous administration);
- antibiotics: Thienam (imipenem plus cilastatin sodium), Doxycycline (in severe cases, infusions are prescribed);
- drugs for cardiovascular failure: solutions of the hormones Dopamine, Adrenaline (drop administration);
- means that normalize the water-salt balance: solutions of glucose, Sodium chloride, Glucosolan, Regidron.
Treatment methods
Pancreatitis in children is treated using complex methods. Patients are prescribed drug therapy and a special diet is selected to eliminate clinical symptoms.
In the absence of serious complications, it is allowed to use folk remedies, but strictly after consultation with a pediatrician. In serious situations with the progression of pathological processes, patients are indicated for surgical intervention.
Conservative treatment
Therapy is carried out when the patient's condition is stable. The child is prescribed bed rest and fasting for a certain period. Conservative treatment is necessary to ensure functional rest of the pancreas.
It is important not only to fast, but also to drink mineral still water (Essentuki, Borjomi) . Glucose and other medications are infused intravenously as prescribed by a gastroenterologist.
With low blood pressure and if the patient is in shock, infusion therapy is performed. Colloid and crystalloid medications are administered through a dropper at a rate of 2-3 liters per day. Infusion therapy can reduce the symptoms of intoxication and remove waste products from the child’s body.
Medication
Traditional therapy helps to stop the clinical signs of the inflammatory-degenerative process, and also restore the functioning of the pancreas and digestive tract. Medicines are prescribed by a pediatrician or gastroenterologist. It is important to adhere to the instructions, since many drugs cause side effects.
| Group of drugs | Name | Application |
| Antisecretory agents | Famotidine, Pirenzepine | The medicine is taken orally, without chewing, with a sufficient amount of water. The pediatric dosage is 20 mg once a day for 4-8 weeks. |
| Antispasmodics | No-Shpa, Baralgin | The daily dosage for children aged 6 to 12 years is 80 mg, divided into 2 doses. Older patients (from 12 years old) are prescribed 40-80 mg 2-4 times a day. |
| Enzymes | Pancreatin, Mezim | The drug is taken orally during or after meals. It is recommended to drink water or fruit juices. The children's dosage is 1 tablet 3 times a day. The treatment regimen and course are selected by a pediatrician, taking into account the child’s condition. |
| Medicines for microcirculation | Pentoxifylline, Trental | The medicine is administered intravenously through a drip. The drug is first dissolved with glucose or sodium chloride. The recommended dosage is 100 mg 2 times a day, morning and evening. |
| Protease inhibitors | Trasylol, Gordox | The medicine is administered in a hospital, intravenously through a drip. The children's dosage is 20 thousand KIU/kg per day. |
| Antibacterial agents | Erythromycin, Sulfanilamide | The medicine is taken orally. For children, the drug is prescribed taking into account body weight, age and severity of the inflammatory process. On average, 20-50 mg/kg per day. The daily dosage is divided into 2-4 doses. |
Drugs are selected individually, taking into account the child’s condition and the degree of development of the disease. It is important to restore your diet while taking medications. Dangerous and progressive conditions are treated in an inpatient setting under the supervision of doctors. Medicines are administered intravenously. Antibacterial therapy is carried out to prevent possible complications.
Surgical
Surgical treatment is indicated in cases where medications have not given positive dynamics, also when serious complications of childhood pancreatitis occur. During medical procedures, the surgeon removes the affected cells of the pancreas, preserving healthy areas of the organ.
Traditional medicine
Pancreatitis in children (symptoms and treatment require a comprehensive examination) allows the use of recipes from healers and healers. Non-traditional remedies help reduce the inflammatory process in the pancreas and also reduce the unpleasant symptoms of pancreatitis.
The use of traditional medicine should be discussed with a doctor, since many of the components used can provoke an allergic reaction or aggravate the child’s condition.
Effective recipes from healers and healers:
| Name | Recipe | Application |
| Honey and herbs | Mix calamus root, dandelion and thyme in equal parts (50 g each). Add nettle root and hops, 25 g each. Mix all ingredients well and chop. Add natural honey (200 g). | It is recommended to give the finished product to the child 1 tsp. 2 times a day. |
| Herbal collection | Mix peppermint and dill seeds 30 g each. Add 20 g of immortelle flowers and hawthorn berries, also 10 g of chamomile flowers. Mix all ingredients well and add hot water (2 tbsp), leave for 2 hours and strain. | The finished product must be given to the child 3 times a day, each time after meals, 30 minutes later. |
| Potato juice | Wash, peel and grate medium-sized potatoes (2-3 pcs.). Squeeze out the juice. | Children are recommended to drink 50 ml of potato juice 2 times a day before meals. The course of treatment lasts 10-14 days. |
| Decoction | Mix St. John's wort, motherwort and immortelle inflorescences in equal parts. Pour 2 tbsp. l. herbal mixture with boiling water (1 l). Place on low heat and heat for 10-15 minutes. Leave the finished broth for another 2 hours and strain. | It is recommended to give the product to children 50 ml before each meal. The medicine is taken for 14-20 days. |
Warm milk and honey help with pancreatitis in children. It is recommended to consume the sweet mixture in the morning.
Standard and scheme
Methods of providing medical care to patients with attacks of acute pancreatitis are selected depending on the cause, severity of the disease and the presence of complications.
When choosing an inpatient treatment regimen, the doctor is guided by the protocol of the initial examination, which is carried out immediately after the patient’s hospitalization, and by a preliminary diagnosis.
If mild pancreatitis is detected, conservative therapy is prescribed. Her tasks:
- pain relief with narcotic analgesics;
- elimination of dehydration due to serial vomiting;
- antibacterial treatment if foci of infection are detected.
Treatment at home
Caring for a patient with pancreatitis at home is possible with a mild course of the disease, when there is no danger of complications, the phase of severe exacerbation has passed. It is impossible to cure pancreatitis forever if the process has entered the chronic stage. But achieve it. To stop the gland from becoming inflamed, you can strictly adhere to all the doctor’s recommendations. As Dr. Komarovsky advises, the dosage of medications must be strictly observed, all prescribed procedures must be followed, and the diet must be strictly adhered to. This is the only way to achieve long-term remission.
Treatment with folk remedies
Due to the particular complexity of the problem, the severity of the disease and complications that can lead to death, the traditional method of treatment for pancreatitis in children is categorically not recommended by specialists. Any medicinal herb can cause an allergic reaction in a child, which will aggravate and complicate the course of the disease.
Deadlines
The duration of inpatient treatment depends on the condition of the person in which he was hospitalized and the accurate implementation of medical prescriptions. Symptoms of mild pancreatitis most often resolve within a few days with intensive drug infusions. Treatment of exacerbations in patients with chronic inflammation of the gland requires much longer hospitalization, especially during surgery.
Acute form of the disease
For a primary attack of moderate pancreatitis, a course of therapy of about 2-3 weeks is required. During this time, in most clinical cases, it is possible to completely improve the pancreas. However, 6 months after discharge from the hospital, treatment must be repeated so that the disease does not become chronic.
Chronic stage
People suffering from a long-term form of pancreatitis need scheduled hospitalization every six months to prevent exacerbations. This is facilitated by medicinal healing of the pancreas and the entire body. The duration of the course of treatment can range from 10 to 21 days.
Symptoms and signs of pancreatitis
Pathological changes of an inflammatory-destructive nature in a small body can develop for a long time without pronounced symptoms. When the first pathological disorders appear, you should urgently visit a pediatrician. The specialist will conduct an examination and prescribe additional tests, taking into account the complaints of the little patient.
Symptoms of reactive pancreatitis in children
Considering the course of pathological processes, pancreatitis in children is accompanied by the following clinical manifestations:
| Name | Symptoms |
| Spicy |
|
| Chronic |
|
| Reactive |
|
In most cases, children are diagnosed with mild pancreatitis; specialists rarely detect purulent-inflammatory lesions.
Further management of the patient
Complications of acute pancreatitis with concomitant diseases, especially diabetes, pathologies of the digestive system, increase the risk of relapse of inflammation of the gland. Such patients, after discharge from the hospital, require follow-up and preventive treatment. Patients who have suffered pancreatic necrosis should examine the condition of the gland every six months. At the same time, it is important not to violate the diet, lead a healthy lifestyle, and at the first signs of exacerbation of the disease, immediately contact a gastroenterologist.
How is pancreatitis treated in a hospital?
- Author of the article
- Olesya Viktorovna Trinikovich
- Gastroenterologist
- Reviewer
- Sergei Andrianov
- Candidate of Medical Sciences
The main dangers of pancreatitis are the development of sepsis (blood infection) and peritonitis (inflammation of the peritoneal tissue).
They develop in the absence of timely treatment of the disease , and their correction is carried out exclusively in a hospital setting.
The article will discuss the main principles of providing first aid to patients diagnosed with pancreatitis, medications and other forms of medical intervention to eliminate the severe consequences of the disease.
Standard of care for patients with pancreatitis
Approved by order of the Ministry of Health and Social Development of the Russian Federation No. 240 dated November 22, 2004
Patient category: adults, children Nosological form: chronic pancreatitis Diagnosis code according to ICD-10: K86.1 Phase: exacerbation Stage: no Complication: no Condition of provision: outpatient care
1.1 Diagnostics
| Service code | Name | Pre-stop rate | Wednesday, quantity |
| A01.15.001 | Collection of anamnesis and complaints for diseases of the pancreas | 1 | 1 |
| A01.15.002 | Imaging examination for pancreatic diseases | 1 | 1 |
| A01.15.003 | Palpation for diseases of the pancreas | 1 | 1 |
| A02.12.001 | Pulse study | 1 | 1 |
| A02.12.002 | Blood pressure measurement in peripheral arteries | 1 | 1 |
| A04.15.001 | Ultrasound examination of the pancreas | 1 | 1 |
| A09.05.003 | Study of the level of total hemoglobin in the blood | 1 | 1 |
| A08.05.003 | Study of the level of red blood cells in the blood | 1 | 1 |
| A08.05.004 | Study of the level of leukocytes in the blood | 1 | 1 |
| A08.05.006 | Leukocyte ratio in blood (blood count) | 1 | 1 |
| A08.05.008 | Study of the level of reticulocytes in the blood | 1 | 1 |
| A08.05.009 | Determination of color index | 1 | 1 |
| A09.05.010 | Study of the level of total protein in the blood | 1 | 1 |
| A09.05.011 | Blood albumin level test | 1 | 1 |
| A09.05.021 | Study of the level of total bilirubin in the blood | 1 | 1 |
| A09.05.022 | Study of the level of free and bound bilirubin in the blood | 1 | 1 |
| A09.05.023 | Blood glucose test | 1 | 1 |
| A09.28.029 | Determination of diastase in urine | 1 | 1 |
| A09.04.046 | Study of the level of alkaline phosphatase in the blood | 1 | 1 |
| A09.05.041 | Study of the level of aspartate transaminase in the blood | 1 | 1 |
| A09.05.042 | Study of the level of alanine transaminase in the blood | 1 | 1 |
| A09.05.044 | Study of the level of gamma-glutamyltransferase in the blood | 1 | 1 |
| A09.05.045 | Study of amylase levels in the blood | 1 | 1 |
| B03.016.10 | Scatological research | 1 | 1 |
| A11.12.009 | Taking blood from a peripheral vein | 1 | 1 |
| A11.05.001 | Taking blood from a finger | 1 | 1 |
| A12.05.001 | Erythrocyte sedimentation test | 1 | 1 |
| A03.16.001 | Esophagogastroduodenoscopy | 0,5 | 1 |
| A06.31.001 | Survey image of the abdominal cavity and pelvic organs | 0,1 | 1 |
How and with what is pancreatitis treated in the hospital?
Upon admission to the hospital, a sick person begins to be treated according to the following principles of pancreatitis therapy (arranged in sequential order):
- relief of pain (with exacerbation of the disease, patients suffer intolerable pain that requires immediate relief);
- neutralization and prevention of complications (at the stage of organ suppuration, antibiotics are used in loading doses or surgical intervention (if drug correction of the condition is impossible));
- detoxification of the body (during the inflammatory process and purulent formations, a large number of toxins are released into the blood, which must be expedited and neutralized) - forced diuresis tactics are used (administration of large doses of diuretics) and abundant infusion of salt solutions (sodium chloride, potassium chloride, calcium chloride). They restore the water-salt balance, eliminating the development of dehydration, which is especially dangerous for a sick person in a similar condition;
- decreased production of enzymes inside the gland (the main reason for the development of pancreatitis is the stagnation of enzymes produced by the gland within itself; reducing their further production will help to quickly stop the inflammatory process). Drugs from the group of proton pump inhibitors (reduce the production of digestive juices at the cellular level) and H1-histamine blockers (reflexively reduce the production of enzymes) are used;
- symptomatic therapy - elimination of dyspeptic disorders (vomiting, stomach pain, intestinal colic and flatulence). Antacids (Almagel, Phosphalugel), antiemetics (Metoclopramide, Cerucal) and fixatives (Loperamide) are used;
- prescription of a diet (complete fasting during the first days of treatment eliminates the inflammatory process and swelling of the pancreas).
Standard treatment for chronic pancreatitis
There is a significant difference between acute and chronic pancreatitis. These diseases have different clinical presentations and different standards of treatment. You might think that chronic pancreatitis occurs as a sluggish acute process, and acute pancreatitis is an exacerbation of a chronic one. But this is not true at all.
Let's look at the symptoms and signs of acute and chronic pancreatitis
While acute pancreatitis is an excess of enzymes, their aggression, a chemical burn of the pancreas, leading to the melting of its tissues and pancreatic necrosis, chronic pancreatitis is a lack of secretion of the organ, which leads to poor digestion of food and insufficient absorption. Hence the various treatment regimens.
The standard treatment for chronic pancreatitis involves constant correction of enzymatic deficiency and the function of improving digestion.
Treatment of an acute process requires urgent cessation of the destruction of pancreatic tissue caused by autolysis, and surgical elimination of these consequences in order to avoid infection and the development of secondary purulent-septic complications of the gland itself and the abdominal cavity.
It is known that acute pancreatitis begins to be treated by an ambulance, and then treatment continues in a surgical hospital, so the patient most often does not care about what exactly to do.
But this is not the case with chronic pancreatitis: almost always the process is controlled by the patient himself, periodically consulting with a gastroenterologist, and it is up to the patient to adhere to the diet and prevent errors and eating disorders.
The patient himself largely determines the course of the disease.
That is why patients need to understand the standard of treatment for pancreatitis, at least in general terms, because the attending physician does not always have the time and opportunity to explain to the patient what to do correctly, what to do and what not to do in the chronic period of the disease, in order to normalize the function of such a complex organ like the pancreas. Therefore, we provide here a brief treatment plan for chronic pancreatitis for a clear understanding of patients.
General standard of treatment for chronic pancreatitis
Before listing the general principles of treatment point by point, it is necessary to say what the goals of this treatment will be. After all, if you don’t know what to strive for, it will be unclear how to do it. The goal of treatment of chronic pancreatitis will be:
- elimination of digestive disorders and pancreatic enzyme deficiency;
- elimination or reduction of the inflammatory process in the gland and other organs (stomach, duodenum);
- preventing complications of the disease.
It is these strong points that will be the main ones, and all other treatment should be called upon to fulfill them. First of all, we will look at non-drug methods of treating the disease.
Non-drug treatment of chronic pancreatitis
The main principles of the treatment regimen are giving up bad habits, periodic fasting and diet. Let's take a closer look at these provisions:
- In a patient with alcoholic pancreatitis, complete abstinence from alcohol reduces pain or completely leads to its disappearance. Individuals who have not consumed alcohol have a good response to therapy during treatment. If the patient completely abstains from alcohol during treatment, then he will not have suppression of the exocrine activity of the gland;
- It is advisable for patients to switch to reducing the number of cigarettes they smoke if the patient smokes, but it is also possible to quit smoking altogether.
Quitting smoking leads to the fact that aggressive saliva containing components of tobacco smoke does not enter the duodenum. As a result, the frequency of pain attacks decreases. In addition, quitting smoking is a good prevention of complications of this disease;
- It’s no secret that chronic pancreatitis can turn into an acute process if there are errors in the regimen. Therefore, in case of severe exacerbation and intensification of the pain syndrome, prophylactically, patients are recommended to fast for a day or two, with the use of alkaline mineral waters. This is necessary to reduce enzyme aggression and neutralize the acidity of gastric juice;
- Diet is the cornerstone in the treatment of chronic pancreatitis. This is table number 5 according to Pevzner. All food should be low-calorie, no more than 2200 kilocalories per day. It should be taken in small doses, five to six times or more per day.
The patient should make every effort to help the enzymes process food, based on their insufficient quantity. To do this, take lean meat and fish, boil it and twist it. Porridge is pureed in the same way as vegetables in soup.
Regular vegetables and fruits are consumed boiled or baked. Raw fiber is too rough and can cause pain.
It is necessary to limit fat, extractive substances, for example, rich broths, strong tea, coffee and cocoa, carbonated drinks, etc.
During remission, or the exacerbation subsides, the diet is expanded, and the second option of table number 5 comes into effect. The patient is allowed to increase the amount of protein, and less thermally and mechanically process foods. The energy component also increases, up to 3000 kilocalories per day, but the list of products that are prohibited remains the same.
But in any case, the patient must adhere to the following principles:
- food should never be consumed dry, since enzymes always work only in a liquid medium;
- the break between meals should never exceed 5-6 hours or more;
- To avoid the development of exacerbations, you should never eat too much at night, even diet food.
Now we should outline the basic principles of pancreatitis treatment with drugs.
Drug treatment
The drug treatment regimen for pancreatitis can vary significantly, and a variety of drugs can be used, both modern drugs and those that have been known for many years.
Medicines are used to relieve pain, to treat enzyme deficiency and excess secretion of gastric juice, as well as for auxiliary purposes.
Let's look at the main groups of these drugs:
Pain syndrome
The development of pain syndrome is very undesirable in chronic pancreatitis. The fact is that it is pain that underlies chronic spasm, and spasm leads to an increase in enzymatic aggression inside the gland. Therefore, step-by-step relief of pain in chronic pancreatitis plays a paramount role.
Most often, myotropic antispasmodics are used, which are able to relax the smooth muscles of the ducts and sphincters. Drotaverine hydrochloride, or No-spa, is used. This drug can be used either orally, intramuscularly or even intravenously.
In case of exacerbation, the drug is prescribed continuously, in a course. And during remission, the drug is used sporadically, in case of possible errors in the diet. He is able to gently eliminate mild pain.
A drug such as ketoprofen can also be used occasionally in therapy.
In general, non-steroidal anti-inflammatory drugs can be used to relieve moderate pain syndrome only in the absence of chronic liver diseases, gastric and duodenal ulcers.
With the permission of the doctor, other drugs from this group may be the drug of choice. In severe cases, during an exacerbation, Tramadol can be administered intramuscularly, but this situation will require emergency hospitalization.
Antisecretory agents
The treatment regimen for chronic pancreatitis involves taking proton pump inhibitors, and here we are talking not so much about suppressing the secretion of gastric juice, but rather about the protective effect of proton pump inhibitors in pancreatitis. It is known that injection and administration of these drugs suppresses the chemotaxis of polymorphonuclear leukocytes, and this helps reduce inflammation. We are talking about intramuscular administration of pantoprazole, or esomeprazole.
The patient is also prescribed H2-histamine receptor blockers, for example Famotidine in short courses.
Enzyme deficiency
After the acute phase of pancreatitis has been stopped, the patient is prescribed enzymes and enzyme preparations, preferably with enteric spheres and a high lipase content.
Typically, the dose of lipase per meal for adults is about 30,000 units. It is necessary to calculate replacement therapy based on this amount.
Also, when taking drugs such as Pancreatin, Festal, Panzinorm, Enzistal, Creon, you must follow the following rules:
- in the event that the patient completely follows the diet, the amount of enzyme preparations is calculated once and is not increased, and if he regularly makes mistakes in the diet, then the amount of the drug can be increased;
- If the patient eats light snacks, the dose of enzymes is reduced by 50%;
- Enzymes must be taken with food or immediately after it.
The patient must be prepared for the fact that these drugs need to be taken for at least several years, or even for the rest of his life.
Ancillary drugs
As an auxiliary therapy, patients are most often prescribed vitamins of the fat-soluble group (A, D, E). They are needed if the patient has severe steatorrhea and loss of fat through the intestines.
If enzyme preparations do not cope sufficiently with steatorrhea, then the loss of fats, including vitamins, must be compensated.
A lack of vitamins in a patient’s blood can lead to secondary complications not directly related to the disease.
In conclusion, it must be said that patients with chronic pancreatitis do not necessarily need to keep a full range of medications at home, from Tramadol to Octreotide.
Treatment with full adherence to the diet, giving up all bad habits and control over your desires will be much more effective.
As practice shows, the greatest number of exacerbations occur not against the background of compliance with the treatment regimen, but as a result of errors.
Source: https://pankreotit-med.com/standart-lecheniya-xronicheskogo-pankreatita/
What can you bring to the patient?
In the first month after an exacerbation of the disease, the patient is prescribed a strict diet. During the first week of hospital stay, complete abstinence from food is indicated. It is allowed to use only :
- heated mineral water;
- sweet tea;
- decoction of dried fruits.
Excellent options for giving to the patient these days would be: “Borjomi”, ready-made compotes from dried apricots and dried apples, tea, sugar.
From the second week you are allowed to consume:
- vegetable broths;
- boiled meat ( low-fat varieties );
- boiled fish;
- porridge with water from ground or grated cereal;
- dried bread.
You can bring sweet crackers, ready-made broths (potato, carrot), ground cereals, which just need to be poured with boiling water for cooking, boiled protein products.
From the third week the menu expands significantly. It becomes the usual diet for patients with pancreatitis , which will need to be followed for several more months after recovery.
It excludes the consumption of the following dishes and food ingredients:
- fat;
- roast;
- salty;
- smoked;
- spicy;
- fresh vegetables and fruits ( except sweet apples, strawberries, pears, apricots );
- coffee;
- carbonated drinks;
- meat broths (fat);
- salo;
- fatty meat and fish;
- alcohol.
Standards of care in hospital
, the following types of assistance can be provided in a hospital :
- resuscitation measures (for complications that threaten the patient’s life);
- surgical intervention (in case of extensive necrosis (death of cells) of the organ or blockage of the pancreatic ducts);
- intensive drug therapy;
- physiotherapy (during the recovery period);
- constant monitoring by specialists of the patient’s condition.
Surgical therapy
How long does it take?
The operation is performed only if there is a threat to human life and if it is impossible to correct the situation using traditional means of treatment . There are several areas of surgical intervention for pancreatitis:
- organ resection (removal of the dead part in order to stop further necrotic process);
- eliminating blockage of the pancreatic ducts, which prevents the excretion of enzymes into the small intestine;
- removal of abscesses and pseudocysts filled with pus and remnants of dead tissue.
Therapeutic measures
In the absence of arterial hypotension and symptoms of pancreatic necrosis:
- Providing a medical and protective regime;
- With severe pain and a typical clinical picture:
- Drotaverine (No-spa) – 40 mg IM (slow IV bolus) or
- Papaverine 2% – 2 ml IM;
- If there is vomiting :
- Metoclopramide – 10 mg IM (slow IV bolus);
- Medical evacuation (see “General tactical measures”).
In the presence of arterial hypotension, symptoms of pancreatic necrosis:
- Scope of treatment measures according to the “Acute peritonitis” protocol.
How is the acute form treated?
The main tasks in the treatment of the acute form will be:
- elimination of swelling and inflammation of the organ;
- prevention of complications;
- detoxification.
The swelling goes away due to a decrease in enzyme production with the help of centrally acting antienzyme agents - Sandostatin, Octreotide (they affect the brain centers responsible for activating the process of production of digestive juices in the gastrointestinal tract).
Antispasmodics are actively used. They neutralize blockage and spasm of the pancreatic ducts and additionally promote the outflow of enzymes from the organ. In the absence of spasms, the pain syndrome also goes away.
Used: “Duspatalin”, “Sparex”, “No-shpa”, “Trimedat”.
Complications go away thanks to the introduction of large doses of antimicrobial drugs. Detoxification is carried out by “diluting” the blood with salt preparations (saline, etc.) and diuretics.
Terms of treatment for chronic
In the acute form of the disease, the patient remains in the hospital for about a month (perhaps he will be discharged earlier, but subject to strict adherence to the doctor’s instructions and bed rest). After the main treatment, there follows a long period of recovery of the body and a rehabilitation period (if surgery was performed).
Correction of conditions during exacerbation of the chronic form occurs faster - about two weeks. Afterwards, the patient returns home with an extract and a prescribed diet.
Full recovery after an attack occurs in 3-4 months.
Further adherence to the diet and medication will record a positive result and promote recovery.
Use of enzyme preparations
Pancreatitis in children (symptoms and treatment are determined by a pediatrician after a complete diagnosis) is characterized by an inflammatory-degenerative process. Exacerbation of the disease leads to disruption of the pancreas and slowdown of food digestion.
To help the affected organ, the pediatrician or gastroenterologist additionally prescribes enzymes for the child. The preparations contain pancreatin. This is an active component that helps break down carbohydrates, fats, proteins and promotes their absorption into the blood.
The child is prescribed the following medications:
| Name | Application | Contraindications |
| Creon | Capsules are taken orally with a sufficient amount of liquid. Children are prescribed 1-2 capsules during the main meal. The daily dosage should not exceed 15 tablets. |
|
| Panzinorm | The medicine is taken orally with meals. The children's dosage is 100 thousand units per day. |
|
| Festal | The medicine is taken orally 1-2 tablets during meals or after meals 3 times a day. |
|
Medicines should be taken strictly according to instructions or adhere to medical prescriptions to avoid side effects and achieve maximum therapeutic effect.
catalogue of articles
[td] Modern methods of treatment of acute pancreatitis
Standards for the treatment of acute pancreatitis Protocols for the treatment of acute pancreatitis
Profile:
surgical.
Stage:
hospital.
The purpose of the stage:
relief of pancreatic inflammation and removal of necrotic pancreatic tissue. Duration of treatment (days): 16.
ICD codes:
K85 Acute pancreatitis K86 Other diseases of the pancreas.
Definition:
Acute pancreatitis (AP) is characterized by the development of pancreatic edema (edematous pancreatitis) or primary aseptic pancreatic necrosis (destructive pancreatitis) followed by an inflammatory reaction. Acute destructive pancreatitis has a phase course, and each phase corresponds to a specific clinical form.
Classification:
1. Acute mild pancreatitis. 2. Acute severe pancreatitis. A) aseptic pancreatic necrosis, b) infected pancreatic necrosis. 3. Acute severe pancretitis, complicated.
Risk factors:
biliary, toxic-allergic, contact, angiogenic, toxic-infectious, post-traumatic, complicating, cryptogenic.
Diagnostic criteria:
Repeated vomiting, girdle pain, increased amylase in the blood, increased size of the pancreas and fluid content in the omental bursa. In parallel with the diagnosis of acute pancreatitis, it is necessary to determine the severity of the disease.
The most important thing is the early detection of severe pancreatitis, the results of treatment of which are largely determined by the timing of its onset. Signs characteristic of severe AP are the following: peritoneal syndrome, unstable hemodynamics, oliguria, hemoglobin above 150 g/l, leukocytosis above 14x109/l, glucose above 10 mmol/l, urea above 12 mmol/l. The presence of at least two signs makes it possible to diagnose severe AP, which is subject to referral to the intensive care unit. For the remaining patients (non-severe pancreatitis), hospitalization in the surgical department is indicated.
List of main diagnostic measures:
1. General blood test (6 parameters) 2. General urine test 3. Determination of glucose 4. Determination of residual nitrogen 5. Determination of creatinine 6. Determination of total protein 7. Determination of bilirubin 8. Determination of potassium/sodium 9. Determination of diastase 10. X-ray examination of organs abdominal cavity (irrigoscopy) 11. Determination of blood group and Rh factor 12. ECG 13. Histological examination of tissue 14. Microreaction 15. Blood test for HIV 16. Anti-HBS 17. Ultrasound of the abdominal organs 18. Computed tomography 19. Esophagogastroduodenoscopy 20. HbsAg, Anti-HCV.
Treatment tactics:
The optimal type of treatment for AP in the enzymatic phase is intensive conservative therapy. To treat mild pancreatitis, it is enough to carry out a basic treatment complex: – hunger; – probing and aspiration of gastric contents; – local hypothermia (cold on the stomach); – analgesics; – antispasmodics; – infusion therapy in a volume of 40 ml per 1 kg of patient’s body weight with forced diuresis for 24-48 hours.
It is advisable to enhance basic therapy with antisecretory and antienzyme therapy.
If there is no effect from basic therapy within 6 hours and there is at least one of the signs of severe pancreatitis, severe pancreatitis should be diagnosed and the patient should be transferred to the intensive care unit and treated according to severe acute pancreatitis.
Intensive therapy for severe pancreatitis:
The main type of treatment is intensive conservative therapy. The above basic treatment complex for severe AP is not effective enough and should be supplemented with a specialized treatment complex (see below). The effectiveness of the latter is maximum when treatment is started early (the first 12 hours from the onset of the disease).
Surgical intervention in the form of laparotomy is indicated only in the event of the development of surgical complications that cannot be eliminated by endoscopic methods (destructive cholecystitis, gastrointestinal bleeding, acute intestinal obstruction, etc.).
Specialized treatment:
1. Antisecretory therapy (the optimal period is the first three days of the disease): the drug of choice is sandostatin (octreotide) 100 mcgx3r subcutaneously; reserve drugs – quamatel (40mgx2r i.v.), 5-fluorouracil (5% 5ml i.v.). 2. Rheologically active therapy (heparin, rheopolyglucin, refortan, etc.). 3. Compensation for plasma loss (correction of water-electrolyte, protein losses, etc.: in total, at least 40 ml of appropriate infusions per 1 kg of body weight; the ratio of colloid and crystalloid solutions is 1:4). 4. Histoprotection: antienzyme therapy (contrical - no less than 50 thousand units, gordox - no less than 500 thousand units intravenously; the optimal period is the first 5 days of the disease); antioxidant and antihypoxic therapy. 5. Detoxification; 6. Broad-spectrum antibiotic therapy using two antibiotics (fluoroquinolones, metronidazole).
Laparoscopy is indicated:
– patients with peritoneal syndrome, including those with ultrasound signs of free fluid in the abdominal cavity; – if it is necessary to differentiate the diagnosis from other diseases of the abdominal organs.
Indications for surgery:
acute abdominal syndrome, and the presence of parapancreatic leaks, infection of the sequestra.
Main methods of surgical treatment:
– decompression and drainage of the bile ducts; – sanitation and drainage of the abdominal cavity, omental bursa, parapancreatic tissue; – performing peritoneal lavage; – drainage of purulent cavities, sequestrectomy, pancreatectomy, pancreatectomy.
List of essential medications:
1. Metronidazole tablet 250 mg solution for infusion 0.5 in a 100 ml bottle 2. Iodine + potassium chloride + glycerin + Water solution in 25 ml bottles 3. Prednisolone 5 mg, table 4. Sodium chloride single-component and combined solutions for infusions and injections 5. Glucose solution for infusion 5%, 10% in a bottle of 400 ml, 500 ml; solution 40% in an ampoule 5 ml, 10 ml 6. Dextran molecular weight about 60000 - 400 ml 7. Polyvidone 400 ml, fl 8. Albumin solution for infusion in a bottle 5%, 10%, 20% 9. Metoclopramide tablet 10 mg; solution in an ampoule 2 ml 10. Neostigmine solution for injection 0.05% in an ampoule 1 ml; tablet 15 mg 11. Drugs derived from blood, plasma substitutes and agents for parenteral nutrition 12. Famotidine tablet 40 mg injection solution 20 mg 13. Furosemide 40 mg tablet 14. Aminophylline injection solution 2.4% in 5 ml ampoule, 10 ml.
Criteria for transfer to the next stage:
achieving an aseptic pancreatic cyst with pancreatic necrosis.
International standards for the treatment of pancreatitis
Pancreatitis is a serious disease of the gastrointestinal tract, which necessarily requires immediate and highly qualified intervention by professional medical staff who specialize in the diagnosis and treatment of diseases of the digestive tract. It is based on an official document with a narrow purpose, the International Protocol for the Treatment of Pancreatitis. This is a list of specific data that lists in strict sequence all the important measures that should be taken in the process.
The international protocol for the treatment of the pancreas for pancreatitis provides for the following main stages:
- correct and timely diagnosis;
- therapy for mild forms of the disease;
- therapeutic measures to get rid of pancreatitis in severe form;
- surgical intervention to urgently improve the patient's condition.
In addition, the protocol prescribes basic recommendations for the treatment of pancreatitis in the following main phases:
- The enzymatic phase, which lasts in the first five days after the presence of the disease is detected.
- The reactive phase, which is part of the course of the acute form of the disease.
- An acute form in which serious purulent complications occur.
The official protocol for the treatment of pancreatitis provides for all possible and most effective methods of treating gastrointestinal diseases. Among them, experts give preference to the most gentle and natural ones. For example, hunger, application of cold, probing, etc.
In case of ineffectiveness of primary methods of treating the pancreas, the protocol offers more intensive methods of therapy.
This is a stay within the walls of a hospital (resuscitation), which is necessarily accompanied by the use of potent medications that can quickly relieve pain, restore the natural environment in the digestive organs, and reduce toxicity of the body.
In other cases, the international protocol for the treatment of pancreatitis offers patients a highly effective and surgically uncomplicated laparoscopic operation, which requires qualified recovery.
Thus, for effective and quick relief from the causes and symptoms of pancreatitis, highly qualified medical specialists are guided by the official protocol for the treatment of the pancreas.
Sources used: zhkt.guru
catalogue of articles
Modern methods of treatment of chronic pancreatitis Standards of treatment of chronic pancreatitis
Protocols for the treatment of chronic pancreatitis
Chronic pancreatitis and other diseases of the pancreas
Profile:
therapeutic.
Stage of treatment:
polyclinic (outpatient).
Purpose of the stage:
1. Ensuring remission.2. Prevention of complications.
Duration of treatment: 14 days.
ICD codes:
K86 Other diseases of the pancreas K86.0 Chronic pancreatitis of alcoholic etiology K86.1 Other chronic pancreatitis K86.2 Pancreatic cyst K86.3 False pancreatic cyst
K86.8 Other specified diseases of the pancreas.
Definition:
Chronic pancreatitis is an inflammatory and destructive process in the pancreas, characterized by focal necrosis in combination with diffuse or segmental fibrosis, the development of functional failure and progression after the cessation of exposure to etiological factors.
Classification of chronic pancreatitis
(Marseille-Rome, 1988)1. Chronic calcific2. Chronic obstructive3. Chronic fibrous-indurative
4. Chronic cysts and pseudocysts of the pancreas.
Classification of chronic pancreatitis
(A.L. Grebenev, 1982, M.N. Sakovich, 1999, as amended)I. According to etiology and pathogenesis: 1. Primary: alcoholic; nutritional; toxic, including medicinal; viral; idiopathic.2.
Secondary:• biliary-dependent• caused by diseases of the duodenum• dystrophic-metabolic (due to chronic liver diseases, ulcerative colitis, malabsorption and hypoxia syndrome, hypoxemia of any origin)• vascular origin• with obesity• caused by helminthiasis.
• caused by mumps and other viral diseases.
II. According to morphological characteristics: calcifying; obstructive; fibrosclerotic (indurative); retention cysts and pseudocysts.
III. According to clinical signs: 1. Recurrent: in the acute phase; in remission phase.2. Painful: with constant pain; with attacks of pancreatic colic.3. Pseudotumorous: with cholestasis; with impaired patency of the duodenum.4. Painless
5. Latent.
IV. Based on signs of pancreatic dysfunction: 1. With excretory insufficiency2. With endocrine deficiency
3. With excretory and endocrine insufficiency.
V. By degree of severity*: mild, moderate, severe. *Severity of chronic pancreatitis.
VI. Complications: 1. Early: obstructive jaundice; retention cysts; pseudocysts; gastrointestinal bleeding; hepatargia; portal hypertension.
2. Late: steatorrhea and other signs of maldigestion and malabsorption; duodenal stenosis; encephalopathy; arthropathy; vascular disorders; local infections.
A mild degree is characterized by the absence of signs of external and intrasecretory insufficiency. Clinical signs (pain, dyspepsia) are moderate. It is possible to increase the activity of pancreatic enzymes in the blood and urine. Exacerbations 1-3 times a year.
The moderate degree is characterized by distinct clinical and laboratory abnormalities, the presence of exocrine and intrasecretory functions of the pancreas, and concomitant lesions of other digestive organs. Possible weight loss Exacerbations 4-5 times a year.
A severe degree is characterized by pronounced clinical and laboratory manifestations, persistent “pancreatic” and pancreatogenic diarrhea, protein deficiency, polyhypovitaminosis, progressive exhaustion, and natural damage to other organs and systems.
Exacerbations 6-7 times a year or more often.
Risk factors:
Alcohol. Gallstone disease. Metabolic disorders (metabolic and hormonal disorders). Hereditary chronic pancreatitis.
Autoimmune pancreatitis associated with primary sclerosing cholangitis, primary biliary cirrhosis and Sjogren's syndrome. Surgeries, trauma to the pancreas. Viral infections. Acute circulatory disorders in the pancreas.
Allergic reactions, toxic effects (uremia during kidney transplantation), deficiency of antioxidants in food. Hyperparathyroidism - increased calcium in the blood.
Diagnostic criteria:
1. Recurrent abdominal pain syndrome (usually in the area of the anterior abdominal wall with radiation to the back, associated with dietary overload, alcohol intake). Ulcerative pain syndrome, reminiscent of left-sided renal colic with impaired motor skills.2.
Loss of body weight (malabsorption syndrome).3. Diarrhea.4. Insufficiency of exocrine function (steatorrhea, hypocalcemia, hypovitaminosis).5. Insufficiency of exocrine function (impaired glucose tolerance, diabetes mellitus).6.
Chronic fibrous-indurative pancreatitis is characterized by intermittent jaundice.7. X-ray signs: pancreatic calcifications, displacement, narrowing of the lumen and expanded contours of the loop 12 p.c. in a state of hypotension.8.
Ultrasound, CT and NMR signs: increased size, echo density, presence of calcifications, tumor or cyst.9. ERCP: deformation and diffuse dilatation of the duct, has an irregular, clear-cut appearance, identification of stones and strictures of the main duct and its lateral branches.10.
Laboratory signs: during a painful attack - an increase in serum amylase levels (more than 2000 units), leukocytosis with a shift in the leukocyte formula to the left. With obstruction of the biliary tract - increased levels of alkaline phosphatase, ALT and bilirubin.
Serum C-reactive protein concentration is a reliable indicator of the severity of pancreatitis. A significant increase (threefold) in ALT or AST speaks in favor of a biliary etiology of pancreatitis.
11. Hypoalbuminemia, changes in coagulogram parameters, hyperglycemia, steatorrhea, decreased lipase activity in duodenal contents.
Source: https://sarhive.ru/mezhdunarodnye-standarty-lechenija-pankreatita/