Fermentative dyspepsia is a complex of symptoms associated with insufficient breakdown of carbohydrates in the small intestine. Undigested substances enter the large intestine and undergo fermentation under the influence of bacteria. The pathological condition reduces performance, impairs quality of life and, in severe cases, leads to deficiency of essential nutrients.
Symptoms
During fermentation, organic acids, carbon dioxide, and hydrogen are formed, which irritate the intestinal mucosa and increase motility. Feces attract water into the intestinal lumen and liquefy. Pathology occurs at any age. Characteristic symptoms appear after eating foods rich in carbohydrates.
Intestinal manifestations
Intestinal symptoms occur with dyspepsia of any severity.
- cramping pain in the abdomen, which decreases after the passage of gas and bowel movements;
- watery, foamy, light yellow stools more than 2 times a day;
- lumps in stool;
- sour smell of stool;
- feeling of fullness, bloating;
- The release of gases is practically odorless.
Extraintestinal manifestations
Insufficient digestion of carbohydrates reduces the absorption of glucose, galactose, and fructose. Fermentative dyspepsia without treatment leads to chronic inflammation in the intestines with disruption of all its functions. A deficiency of fats, proteins, vitamins, and microelements develops.
Symptoms:
- weakness;
- irritability;
- dizziness;
- weight loss in adults, insufficient weight gain in infants;
- dry skin;
- fragility and change in the shape of nails;
- hair loss.
Fermentative dyspepsia in children
Dyspepsia can also occur in children, who will experience and present the same complaints as adult patients. The exception is infants who cannot report their illness, so parents have to guess about the pathology that has arisen based on external signs.
- The main symptom of indigestion in an infant is green stool with white spots, as well as bloating.
- Discomfort makes the child restless and capricious.
- Like an adult, vomiting and diarrhea cause dehydration in an infant. This is easy to recognize by dry skin. But for a child’s body, dehydration is a much more dangerous phenomenon, which can lead to seizures.
When the first signs of dyspepsia appear in a child, you should immediately consult a doctor.
Causes
Fermentative dyspepsia is caused by two groups of reasons: enzyme deficiency and malnutrition.
Enzyme deficiency
Pancreatic amylase in the duodenum breaks down complex carbohydrates - polysaccharides into oligo- and disaccharides. Under the action of enzymes in the small intestine, monosaccharides are formed from them, which are then absorbed into the blood.
Intestinal enzymes have substrate specificity, each of them converts only a certain disaccharide: lactase breaks down lactose (milk sugar), maltase - maltose, invertase - sucrose, etc. Disruption of one enzyme leads to intolerance to a particular product. In Russia, lactase deficiency (milk intolerance) occurs in 15% of the adult population and 18% of children under one year of age. Against the background of intestinal diseases, intolerance to several carbohydrates develops.
Be sure to read: Diarrhea: possible causes and treatment (diet, rehydration, medications)
Causes of enzyme deficiency:
- heredity;
- pancreas pathology;
- bacterial and viral intestinal infections;
- helminthiases;
- chronic enteritis;
- Crohn's disease;
- food allergies;
- long-term parenteral nutrition.
Eating disorder
When the intake of carbohydrates from food exceeds the capabilities of the body's enzyme systems, some of the undigested components undergo fermentation. Dyspepsia occurs when eating large amounts of high-carbohydrate foods:
- whole milk;
- infant formula;
- dairy products;
- fresh vegetables and fruits;
- baking;
- sweets;
- mushrooms;
- potato;
- kvass, beer;
In older people, enzyme activity decreases, and even a small error in nutrition can lead to fermentative dyspepsia.
Reasons for development
The main cause of dyspepsia is poor nutrition. However, not every person knows what this definition includes.
First of all, we are talking about the consumption of low-quality products and an unbalanced diet. The term also includes:
- quick snacks on the run;
- eating during times of stress and emotional irritation;
- monotonous diet (mono-diet);
- binge eating.
All these factors increase the load on the digestive system, resulting in even healthy organs being unable to digest food properly.
Such disorders are called functional: that is, human organs are absolutely healthy, but their function is impaired under the influence of external factors.
The main cause of fermentative dyspepsia is an excess of carbohydrates in the diet: when a person eats a lot of foods rich in carbohydrates, especially fiber, the amount of fermentative microflora in his intestines increases. It is at this moment that a person experiences all the unpleasant symptoms of dyspepsia.
In some cases, disruption of the digestive process can occur under the influence of not only external, but also internal factors.
- For example, if a person has reduced secretion of gastric juice: in this case, even a moderate amount of fiber consumed cannot be digested correctly, which is why fermentation actively develops in the intestines.
- Similar reasons include a decrease in the volume of pancreatic amylase, a special enzyme that is produced by the pancreas and salivary glands to break down carbohydrates, and a decrease in the motor activity of the small intestine.
- Another reason why pathology may develop is insufficiently thorough chewing of food. Firstly, this increases the load on the digestive system, and secondly, the food bolus is not sufficiently treated with amylase from saliva.
Statistically, dyspepsia is more common in the hot season, when a person drinks large amounts of liquid. In this way, it dilutes the digestive secretions so that food cannot be digested completely and correctly. This is especially relevant if a person suppresses thirst not with water, but with cold carbonated drinks.
Diagnostics
Diagnosis of fermentative dyspepsia and its causes is carried out by pediatricians, therapists, and gastroenterologists.
Clinical and laboratory methods
- Anamnesis collection, examination . To make a preliminary diagnosis, typical complaints, indications of intolerance to specific foods, improvement in well-being after eliminating them from the diet, family history, acute and chronic diseases of the digestive system are important.
- Coprogram. With fermentative dyspepsia, the feces have an acidic reaction. The analysis results reveal unchanged fiber, starch grains, and lactic acid.
- Bacteriological examination of feces - the amount of iodophilic flora increases: yeast fungi, clostridia, cocci.
- Feces for worm eggs - vegetative forms and protozoan cysts, eggs of intestinal parasites are revealed.
- Stool analysis for carbohydrates is prescribed to diagnose lactose intolerance in children who do not receive complementary foods.
- Load test with disaccharides - after taking milk sugar or sucrose, the level of glucose in the blood is determined. An insufficient increase in the indicator indicates a decrease in lactase or invertase activity.
Instrumental methods
- Hydrogen test - measures the concentration of hydrogen in exhaled air. An increase in the rate is associated with bacterial fermentation in the colon.
- X-ray with contrast. The patient is given a drink of barium with lactose or sucrose and a series of photographs are taken. Accelerated movement of contrast through the intestines indicates enzyme deficiency.
- Biopsy of the mucous membrane of the small intestine - determine the content of enzymes in the resulting material. Using research, they find out which enzyme is missing.
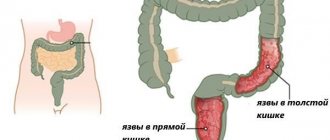
- Endoscopic diagnostic methods. FGS and colonoscopy reveal chronic intestinal diseases, which can lead to fermentative dyspepsia.
- Ultrasound – diagnosis of the causes of pathology; clarify the structure, size and pathological changes of the abdominal organs.
Be sure to read:
Does meat rot in the intestines?
Dyspepsia
Gastritis
Diabetes
Diarrhea
9032 12 November
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Dyspepsia: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
The term dyspepsia is understood as a complex of disorders that indicate disruption of the normal functioning of the stomach and are accompanied by various symptoms that persist for 3 months in a row. Dyspepsia is manifested by pain or a feeling of heaviness (fullness) in the upper abdomen. Such discomfort may not be associated with food intake, but may be accompanied by nausea, bloating, heartburn, and belching.
Dyspepsia can be a symptom of various functional and organic disorders of the gastrointestinal tract, and if it occurs, consultation with a specialist is necessary.
Types of dyspepsia
There are many types of dyspepsia.
- Nutritional dyspepsia is the result of prolonged non-compliance with food intake rules and unbalanced nutrition. Nutritional dyspepsia has three subtypes:
- fermentative subtype - caused by excessive consumption of simple carbohydrates (sugars, flour products, fruits, legumes, etc.), fermented vegetables and fermented drinks (kvass, beer), as a result of which the balance of the intestinal microbiota shifts towards the fermentable flora;
- putrefactive subtype - caused by excessive consumption of protein foods (meat products and semi-finished products that require a lot of time to digest);
- fatty subtype - caused by excessive consumption of foods saturated with refractory fats (pork, lamb, etc.).
Causes of dyspepsia
Dyspepsia is the result of many pathological mechanisms. The appearance of a complex of symptoms characteristic of dyspepsia is caused in a quarter of cases by slower gastric emptying. In this case, pain and a feeling of heaviness are accompanied by vomiting and a significant decrease in appetite.
Some patients have increased sensitivity of the gastric and duodenal mucosa to stretching by food masses, which causes spasm of smooth muscles and pain.
In about a third of cases, the nervous system dysregulates the contraction of the stomach muscles, resulting in spasms that cause pain during stomach contractions.
Mild infections and indolent inflammatory lesions of the stomach and duodenum lead to the development of functional changes in the functioning of the digestive system. Various genetic factors predispose to the development of such dyspepsia.
Among the diseases that are accompanied by symptoms of dyspepsia, chronic gastritis and gastroduodenitis should be highlighted.
These diseases often occur in adolescence and young adulthood, when there is not enough time for proper and, importantly, regular nutrition.
There is a disruption in the production of mucus, which protects the gastric mucosa from mechanical and chemical influences (especially from hydrochloric acid, which is part of the gastric juice).
Dyspepsia is a constant companion to peptic ulcers of the stomach and duodenum. The symptoms of an ulcer are very varied and depend on its location in the wall of the organ.
Pain can occur after eating or, conversely, “hunger pain.” Other symptoms of dyspepsia due to peptic ulcers are belching, nausea or even vomiting after eating.
In recent years, the medical community has given increasing importance to
Helicobacter pylori (H. pylori)
. Damage to the gastric mucosa occurs when the vital activity of this bacterium increases and upsets the balance between protective and damaging effects. The bacterium is very resistant to the acidic contents of the stomach and can significantly damage the mucous membrane, including the development of ulcerative defects. If instead of a special course of eradication therapy (to destroy this bacterium) only symptomatic treatment is carried out, then in the autumn-spring period exacerbations of gastroduodenitis and gastric ulcer occur.
Along with infectious causes of dyspepsia, there are psychosocial factors in the appearance of unpleasant symptoms. Stress, depression and anxiety lead to disruption of the regulation of the correct rhythm and adequate volume of secretion of gastric contents.
The secretion of hydrochloric acid increases and the gastric mucosa is damaged.
Gastroesophageal reflux disease (GERD) is one of the common causes of dyspepsia symptoms. Patients feel a burning sensation in the lower chest, especially after eating and when bending down in a lying position.
Painful sensations arise due to the reflux of acidic and aggressive gastric contents into the esophagus, and the esophageal mucosa suffers.
In some cases, symptoms of dyspepsia may indicate the development of certain heart diseases. One of the most common causes of pain is the abdominal form of myocardial infarction.
Low blood pressure may accompany the classic symptoms of dyspepsia.
Symptoms arise due to the special location of the heart attack - on the lower surface of the heart, directly above the diaphragm and stomach.
Long-term and uncontrolled use of certain medications (for example, non-steroidal anti-inflammatory drugs) leads to an imbalance of gastric protective factors and aggression factors. Acid damages the unprotected mucous membrane with the formation of erosions and ulcers.
Predisposing factors for the development of symptoms of dyspepsia and gastrointestinal diseases:
- violation of diet (long breaks between meals);
- food “on the run”, dry;
- abuse of spicy, sour, spicy, fried foods;
- very hot or very cold food;
- smoking and alcohol abuse (especially strong drinks), coffee;
- diabetes;
- kidney disease;
- burns, massive injuries and other causes of severe pain.
Which doctors should I contact?
The appearance of symptoms of dyspepsia requires contacting a general practitioner: a therapist or a pediatrician. After the examination, the doctor will prescribe a set of instrumental and laboratory tests and, if necessary, refer you to a specialist. You may need to consult a gastroenterologist, surgeon, or cardiologist.
Diagnosis and examination when symptoms of dyspepsia appear
During the examination, it is possible to use both laboratory and instrumental research methods.
- Clinical blood test;
Treatment
The goals of treatment measures are to reduce symptoms and normalize the functioning of the digestive tract.
Nutrition
Diet correction is a prerequisite for successful treatment of fermentative dyspepsia.
Basic principles
- The diet is prescribed individually; if a particular enzyme is deficient, carbohydrates that it should break down are excluded from the diet.
- For dyspepsia due to diseases of the digestive system, a diet is recommended in accordance with the diagnosis.
- All patients are prohibited from foods that increase gas formation and rough foods.
- In severe cases, carbohydrates are completely eliminated for 3-4 days and the proportion of protein products in the diet is increased.
- They recommend split meals: small portions up to 6 times a day.
- Cooking methods: boiling in water or steaming, baking in the oven.
Grocery list
| Recommended | Forbidden |
In the first days of treatment:
After 3-4 days:
|
|
Children under one year of age with lactose intolerance are prescribed low-lactose and lactose-free mixtures: NAN lactose-free, Nutrilak lactose-free plus, Nutrilon premium lactose-free, etc.
Medicines
- Enzyme preparations. If the functioning of the pancreas is disrupted, medications containing pancreatic enzymes are prescribed: Creon, Mezim forte. If fermentative dyspepsia is associated with lactase deficiency, Lactazar is recommended.
- Carminatives are a group of drugs that reduce flatulence and facilitate the passage of gases: Espumisan, Bobotik, Plantex.
- Antispasmodics - reduce the tone of intestinal smooth muscles, have an analgesic effect: Buscopan, No-shpa, Duspatalin.
- Enterosorbents - bind and remove toxic products and gases from the intestines that are formed during fermentation, fix the stool: Smecta, Neosmectin, Polysorb, activated carbon.
- Antidiarrheals - reduce peristalsis, reduce the frequency of bowel movements: Imodium.
Be sure to read:
List of enterosorbents and features of their administration
Treatment with traditional methods
Traditional methods effectively cope with the symptoms of dyspepsia, relieve stress, and calm the nervous system. To remove gases from the intestines, herbal decoctions are useful: chamomile, sage, yarrow. To relieve pain, it is recommended to take warm baths with a decoction of linden flowers at night. The water temperature should be no more than 38°C, the procedure duration should be 20 minutes (for adults).
Herbs for nausea ─ mint, lemon balm, St. John's wort, fennel, ginger. Green tea quickly relieves symptoms; you can add fresh lemon juice and honey to it.
An infusion of elecampane will help cope with pain and discomfort in the abdomen. The raw materials (1 tablespoon per 200 ml of water) are poured with mild boiling water and infused for 6-8 hours. Take 50 ml 30 minutes before meals.
Marjoram and cumin improve the digestion process. Take 1 tbsp. l. each type of raw material is poured with a glass of boiling water. Drink 100 ml 2 times a day after meals.
Prevention
Primary prevention of fermentative dyspepsia is the prevention of diseases of the digestive tract:
- proper balanced nutrition;
- adequate physical activity;
- stress management;
- quitting smoking and alcohol.
To prevent exacerbations of pathology, follow a diet and take medications prescribed by your doctor. If your health worsens, do not self-medicate; consult a therapist or gastroenterologist in a timely manner.
In continuation of the topic, be sure to read:
- Causes of bloating and increased gas formation, treatment methods
- Intestinal disorder and methods of its treatment: diet and medications
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- Rectal cancer: symptoms, stages, treatment and prognosis for life
- Rectal fissure: causes, symptoms and treatment of pathology
- Details about bowel cancer: stages, symptoms, treatment and prognosis
- Irritable bowel syndrome: symptoms and treatments
- More about hemorrhoids: causes, symptoms and treatment methods
- Sigmoiditis (inflammation of the sigmoid colon): symptoms and treatment methods
- Dyspepsia: how is the pathology manifested and treated?