Distal erosive reflux esophagitis (EDE) is an inflammatory disease of the inner lining of the lower part of the esophagus. The inflammatory reaction is manifested by superficial epithelial destruction, without involving the deeper layers of the esophageal wall in the process. The clinical picture is expressed in heartburn, epigastric pain, belching, dysphagia. The uncomplicated form is treated conservatively, using diet therapy, medication, and physiotherapeutic methods. Traditional medicine methods are often used. Let's take a closer look at what erosive esophagitis is and how to treat the pathology.
ICD 10 code K21.0
What is erosive esophagitis
Erosive reflux esophagitis is an inflammatory disease of the esophagus, the pathological basis of which is a violation of the integrity of the organ mucosa by gastric reflux. This is one of the most pressing issues in gastroenterology.
The following factors play a major role in the development of reflux esophagitis:
- Insufficiency of the lower esophageal sphincter (LES). Sphincter weakness can be absolute or relative. Relative failure includes cases of increased intragastric pressure. Intense contraction of the antrum of the stomach can cause reflux of gastric contents even with a normally functioning gastrointestinal tract. More often there are cases of absolute insufficiency of NSP, which is the result of: disruption of coherence in the work of smooth muscles;
- presence of hiatal hernia;
- transesophageal prolapse;
- abuse of certain drugs that relax smooth muscles (sedatives, beta blockers, nitrates).
- Impaired rate of emptying and cleansing of the esophagus (esophageal clearance). Cleansing the esophagus from harmful reflux is carried out due to peristalsis and the alkalizing effect of saliva and mucus. A decrease in esophageal clearance occurs as a result of smoking, drinking alcohol, and fatty foods.
- Disruption of mechanisms that protect the mucosa from damage (disruption of the pre-epithelial aqueous-mucosal layer containing bicarbonates).
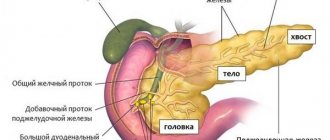
- Violation of all these functions leads to the development of GERD - this is a spontaneous, repeatedly repeated reflux from the stomach and duodenum into the cavity of the esophagus, as a result of which severe inflammation of varying degrees develops in the esophagus, accompanied by a typical clinical picture.
Violation of all these functions leads to the development of GERD - this is a spontaneous, repeatedly repeated reflux from the stomach and duodenum into the cavity of the esophagus, as a result of which severe inflammation of varying degrees develops in the esophagus, accompanied by a typical clinical picture.
Causes of the disease
The main cause of the disease is the poor development of the neuromuscular part of the esophagus. Most often, young children suffer from this disease.
- Due to the strong pressure inside the stomach, the activity of the gastrointestinal tract decreases. The consequence is stomach ulcers and gastritis.
- Weak intestinal motility occurs during stressful situations. Poor nutrition is a frequent accompaniment of the disease. Abuse of sweets, spicy foods, and alcohol leads to symptoms of esophageal disease.
- Excessive use of medications containing nitrites and prostaglandins. Smoking also contributes to the occurrence of reflux esophagitis of the first degree.
Erosive reflux esophagitis: symptoms
Sometimes terminal reflux esophagitis occurs with a minimal clinical picture, patients complain of mild discomfort in the epigastric region. And sometimes these symptoms are absent.
But more often ERE occurs with a clear clinical picture. There are complaints from the esophagus and from other internal organs.
Esophageal symptoms of erosive esophagitis:
- heartburn, more often after an error in diet, but sometimes heartburn occurs regardless of the food eaten;
- pain in the stomach and retrosternal region may be of a pressing nature, radiating to the left arm, but unlike cardiac pain, it goes away with taking antacids and is often preceded by eating;
- dysphagia of varying severity, but unlike esophageal cancer, they are transient;
- belching;
- if the disease is severe, vomiting with blood may occur.
Extraesophageal symptoms of distal erosive reflux esophagitis include:
- from the cardiovascular system - arrhythmias, tachycardia, conduction disturbances, cardialgia;
- from the bronchopulmonary side - night apnea, hacking cough;
- from the otorhinolaryngological organs - chronic laryngitis, pharyngitis;
- from the oral cavity – chronic stomatitis, damage to tooth enamel, periodontitis;
- from the blood side - anemia.
Signs of the disease
The main symptoms of inflammation of the esophageal mucosa are:
- pain in the stomach area associated with damage and inflammation of the surface epithelium;
- hiatal hernia in the diaphragm and displacement of the stomach into the chest cavity.
- First of all, one manifestation that is constantly present is heartburn. Heartburn occurs during meals and is accompanied by belching and sometimes hiccups.
- Painful sensations behind the chest, similar to pain in the heart.
- Swallowing reflex disturbances without signs of hiccups and heartburn, which indicate the onset of complications associated with scar formation of the esophagus and its narrowing.
Classification of the disease. Medical classification of reflux esophagitis:
- Stage A. Erosive lesion of the mucous membrane, consisting of several erosions that are interconnected. Typically the affected area is 5 mm. This is peptic reflux esophagitis.
- Stage B. Lesion zones exceeding 5 mm in size, connecting with each other, but not spreading over the entire surface of the mucosa.
- Stage C. The spread of ulcerative lesions occurs over a large area of the esophageal mucosa, and thus grade 2 reflux esophagitis develops.
Treatment of the disease The main recommendations of the attending physician are:
- adjustments in lifestyle: smoking, alcohol, excess weight - you need to get rid of this. All this is the main reason for the manifestation of reflux esophagitis of the first and second degrees.
- Avoid heavy physical activity associated with frequent bending and tension in the abdominal muscles. Avoid wearing compressive clothing.
Treatment for narrowing of the esophagus must begin at an early stage of development. After endoscopic examination, antisecretory drugs are prescribed that reduce acidity in the esophagus.
Why does heartburn occur?
Based on the diagnostic results, medications are prescribed that improve intestinal motility. To diagnose the disease, daily PH is measured, which allows you to find out the acidity of the esophagus. The higher the acidity, the more severe the reflux esophagitis.
An additional diagnostic test is esophagomanometry. Based on the results of the study, it becomes possible to evaluate the contractile function of the lower esophageal sphincter. During a disease of the esophagus, the sphincter is relaxed, and in this state the manifestations of reflux intensify.
Therapeutic diet for reflux esophagitis:
The basis of the diet for esophageal disease is avoidance of the following foods:
- chocolate, sweets, coffee;
- alcohol, smoking;
- fat-containing products;
- hot spices;
- fast food products.
Priority in nutrition is given to the following products:
- low-fat dairy and fermented milk products;
- boiled eggs, porridge;
- baked apples;
- dried fruit drinks.
Vegetable stews should be consumed with lean boiled meat, vegetable soups, and drinks that reduce acidity should be in the daily diet. It is important to follow a temporary diet. It is recommended to eat food at least four times a day.
Classification of ERE
| Table 1. Classification of ERE | |||||||
| Classification name | Intensity of erosive lesion | ||||||
| Classification by Grigoriev P.Ya. | Degree 0 | Grade I | Grade II | Grade III | Grade IV | Grade V | |
| Slight redness of the tunica mucosa (mucosa) in the terminal part of the organ, its continuity is preserved. | No more than two erosions of tunica mucosa, not extending beyond one fold | Interconnected defects of the tunica mucosa, covered with blood and dead tissue. The area of destruction is no more than half of the distal part of the organ. | Necrotic and hemorrhagic destructions located along the entire circumference of the esophageal opening, interconnected, occupy the entire tunica mucosa of the lower esophagus. | Deep defects of various localization, narrowing of the esophagus, cicatricial changes in its walls. | |||
| Classification of Okorokov A.N. | Exudation and erythema of tunica mucosa, on its surface there is a thick secretion of goblet cells. | Against the background of hyperemia and exudation, individual surface defects of the epithelium appear that do not affect the basement membrane. | Multiple destructions and hemorrhages of the tunica mucosa, in conditions of overflow of its vessels with blood and significant swelling. | Superficial defects of the tunica mucosa are localized along the entire esophagus, the membrane itself is easily wounded, covered with a fibrinous grayish coating. | X | ||
| Savary-Miller classification | Isolated redness of the tunica mucosa with or without leakage of fluid through the vascular wall. | Against the background of hyperemia and exudation, individual surface defects of the epithelium appear that do not affect the basement membrane. | Destructions of tunica mucosa occupying the entire circumference of the lumen of the esophagus are covered with blood and a grayish fibrin film. | Severe complications: narrowing of the esophagus, persistent replacement of the squamous epithelium of the esophagus with columnar epithelium, ulcers. | X | ||
| Hetzel-Dent classification | The esophageal mucosa is not changed | Excessive blood filling and swelling of the tunica mucosa, without visible tissue defects. | Well-defined destruction of the surface epithelium occupies a small area of the tunica mucosa of the lower esophagus. | Superficial and deep destruction of tunica mucosa occupy up to half of its area in the lower esophagus. | Deep tunica mucosa defects in any part of the esophagus, or superficial, interconnected defects occupying the entire lower part of the esophagus | X | |
| Los Angeles classification | Grade A | Grade B | Grade C | Grade D | X | ||
| No more than two erosions of the tunica mucosa, not extending beyond one fold. | Presence of large erosion within the boundaries of one tunica mucosa fold | Destructive processes extend to several folds of the tunica mucosa, but not to the entire circumference of the esophageal opening. | The destructions merge and occupy almost the entire circumference of the lumen of the esophagus. | ||||
Erosive reflux esophagitis 1st degree
Chronic distal catarrhal reflux esophagitis is an easily treatable stage 1 of a non-erosive disease. The patients do not make any complaints. Endoscopically, the picture of catarrhal esophagitis is determined in the distal part of the esophagus - pronounced hyperemia against the background of tissue edema. There are single, small erosions on the mucous membrane. Stage 1 disease does not require special drug therapy; usually it is enough:
- follow a diet;
- establish regular, small portions, multiple meals;
- do not wear tight clothing or tight belts;
- eliminate smoking and alcohol;
- eliminate stress on the abdominals.
Herbal medicine is welcome.
Erosive reflux esophagitis 2 degrees
If the disease progresses, the disease enters stage 2. Stage 2 erosive esophagitis is characterized by the appearance of typical complaints in the patient that arise after errors in the diet. There are both complaints from the esophagus and from other organs.
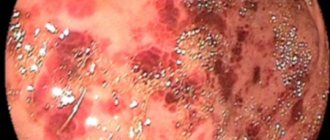
Endoscopically, it is possible to detect the most common form of esophagitis - terminal esophagitis - in the distal esophagus against the background of pronounced edema and hyperemia of the mucous membrane, multiple pinpoint hemorrhages.
As the process progresses, multiple, sometimes merging erosions appear, but the erosions do not spread to the entire mucosa, interspersed with areas of intact tissue; the inner lining of the esophagus is covered in the distal section with purulent-bloody exudate. Sometimes linear erosions are detected.
Stage 2 ERE, in addition to general measures, requires serious drug therapy. Here, H2 receptor antagonists (Famotidine) + prokinetics are more often prescribed; it is possible to add PPIs (proton pump inhibitors), for example, Omeprazole, to the treatment regimen.
Erosive esophagitis grade 3
This is already a serious lesion of the esophagus. The patient has constant complaints. Almost the entire gastrointestinal tract is involved in the process (gastritis, duodenitis, bulbitis). At endoscopy: multiple erosions and ulcers, covered with hemorrhagic and pseudomembranous (fibrinous) exudate, circularly affecting the distal esophagus. The patient's serious condition requires massive therapy with large doses of drugs - INR + PPI + prokinetics + antacid drugs. Therapy is prescribed for the organs involved in the process.
ERE grade 4
This is the most severe stage of the disease, the stage of complications. Endoscopically, deep ulcers of peptic etiology, cicatricial narrowing of the esophagus, hemorrhages, replacement of the squamous cell epithelium of the esophagus with a cylindrical epithelium characteristic of the intestine (Barrett's esophagus) are determined. Treatment at this stage is mainly surgical.
Types, degrees
Distal esophagitis can be characterized by morphological damage to the esophageal mucosa of varying severity. According to this criterion, the following types of illness are distinguished:
Rare types of the disease include dysmetabolic and granulomatous esophagitis.
THIS IS REALLY IMPORTANT! Cheap product No. 1 for the stomach and esophagus. FIND OUT >>
More often, distal reflux esophagitis develops with repeated cycles of cardia insufficiency and appears against the background of exposure to acidic contents from the stomach on the esophagus. According to the nature of the lesions, this disease can be:
- superficial, non-erosive;
- ulcerative with foci of necrosis throughout the entire thickness of the mucosa;
- with damage to the submucosal layers to deep defects, causing thinning of tissues and perforation of the esophageal wall with bleeding.
According to the severity of morphological changes, distal reflux esophagitis develops with the following degrees of severity:
- 1st degree - mild focal redness of the mucous membrane. The structure of the mucosa at the junction with the stomach is loose, with smoothed folds.
- 2nd - single or multiple erosions of an elongated shape with the possible formation of exudate. Wounds appear predominantly in the folds of the mucosa and affect no more than 10% of the entire distal esophagus.
- 3rd - numerous merged erosions, covered with exudate and necrotic tissue. The affected area is more than 50%.
- 4th - merged erosions are located in a circle, severe exudative-necrotic damage is noted. Severe fibrinous lesion covers the entire area 5 cm above the cardia.
GERD in children
The pathogenetic causes of erosive esophagitis in children are the same as in adults. The main points that trigger the process in a child are:
- ANS dysfunction;
- excess nutrition;
- sliding hiatal hernia;
- connective tissue dysplasia.
Treatment tactics depend on the age of the child and the severity of the inflammatory process. In young children, the correction of the process occurs mainly through the establishment of a nutritional regime. In older children, medications may be used:
- PPI (Rabeprazole);
- prokinetics (Domperidone);
- antacids.
If conservative therapy fails, a Nissen fundoplication is performed.
Diagnostics
If erosive esophagitis is suspected, all patients are examined:
- Endoscopic examination - allows you to determine the location, severity and nature of the damage. If necessary, during endoscopic examination, a biopsy of suspicious tissue is taken for further histological and cytological examination.
- X-ray examination is used to determine strictures of the esophagus; in addition, the method allows us to detect the presence of a hiatal hernia of the hiatal hernia and pathological changes in the diaphragm.
- Esophageal manometry - allows you to study the peristalsis of the esophagus, the coherence in the work of the esophageal sphincters and the motility of the organ.
- Determining the amount of acid entering the esophagus during the day - the method reveals how often and for how long the patient has reflux episodes during the day and what contributes to this. The rate of acid neutralization in the esophagus is also determined.
Laboratory diagnostics include:
- peripheral blood analysis;
- stool test for the presence of blood;
- coagulogram.
Differential diagnosis of reflux esophagitis is carried out:
- with coronary pathology (angina pectoris, myocardial infarction), myocarditis, cardiopathy, valvular heart disease.
- in case of violations from the otorhinolaryngological organs, it is necessary to exclude tumors of the larynx;
- with severe hacking cough, it is necessary to exclude chronic diseases and lung tumors;
- Stomach cancer must be excluded.
Tips and tricks
At the initial stage of reflux esophagitis, hoarseness sometimes occurs, a person often has a cough, and is susceptible to bronchitis or laryngitis. Other symptoms characteristic of reflux may not be observed at all.
Treatment in such a situation is selected carefully, trying to eliminate the signs of both diseases at once. Active medication use and diet therapy are the main areas of therapy. People who suffer from reflux of food into the esophagus must definitely give up smoking forever.
Treatment of erosive esophagitis
Treatment for ERE includes:
- methods aimed at changing the living conditions that caused the disease;
- drug therapy;
- treatment with alternative means.
The basis for the treatment of any pathology of the digestive system should be a correct, scientifically based diet. For erosive reflux esophagitis, it involves, first of all, excluding from the menu foods that irritate the parietal cells of the stomach and relax the esophageal sphincter (coffee, chocolate, carbonated drinks). Food should be boiled or steamed. It is necessary to eat regularly and often, taking food in small portions. The diet for ERE is selected individually.
Why heartburn happens after coffee: reasons and recommendations
A patient with erosive esophagitis must avoid physical and emotional stress. You need to sleep with the head of the bed raised.
It is necessary to give up alcohol and smoking.
Drug therapy
Drug therapy largely depends on the severity of the inflammatory process. The duration of treatment and the number of medications taken is determined by the severity of the disease.
Antacids and alginates
Drugs of these groups increase the pH of gastric juice, thereby reducing acid aggression on the esophageal mucosa. Envelop the mucous membrane, providing protection to epithelial cells. The most used antacids are Gastal, Phosphalugel, Maalox. These drugs cannot be used for a long time; micronutrient metabolism may be disrupted. Recently, combination drugs – alginates – have been increasingly used. Once in the stomach, alginates form a thick foamy mass on the surface of its contents. During reflux, this mass enters the esophagus, having a beneficial effect on its mucosa, promoting epithelization of erosive lesions. The most effective alginates are Topalcan and Gaviscon.
Antisecretory drugs
- IGR - drugs inhibit the action of histamine, which is an intermediary in the synthesis and release of hydrochloric acid. These drugs are prescribed for the treatment of mild catarrhal forms of esophagitis, since their effect is insufficient in the treatment of erosive esophagitis. The most commonly used tablets are Cimetidine, Ranitidine, Famotidine, Roxatidine.
- PPIs - drugs in this group block the synthesis of hydrochloric acid at the ionic level, thereby long-term and effectively increasing the pH of the gastric contents. Esomeprazole (Etanera, Ezokar) is considered the most effective, although other PPIs (Omeprazole, Pantoprazole, Rabeprazole) are widely used in the clinic.
Prokinetics
Drugs that accelerate the movement of food contents of the stomach into the intestines by enhancing peristalsis. As a result, congestion in the stomach is eliminated and the tone of the esophageal sphincters increases. Ganaton and Domperidone are considered the most effective.
Surgical treatment of erosive esophagitis
The failure of conservative therapy, the presence of complications and bleeding are indications for surgical treatment. The most common procedure is a Nissen fundoplication.
Treatment and prevention
Treatment of esophagitis is complex, complex and lengthy. It is used to eliminate the root cause of the disease and reduce symptoms.
General recommendations
- timely treatment of concomitant gastrointestinal pathologies, for example, gastritis;
- giving up bad habits: drinking alcohol, tobacco;
- refusal to self-medicate any pathologies, even a simple headache;
- wearing loose clothing without tight belts;
- rest after eating in an upright position or sitting;
- avoid frequent bending of the body forward and carrying heavy objects;
- sleep with the headboard raised 15 cm.
Diet therapy and regimen
A balanced diet is the main component of effective treatment of any gastrointestinal pathology, especially distal catarrhal or fibrinous esophagitis.
Basic principles:
- small, frequent meals - up to 7 times a day every 2-3 hours;
- small portions - up to 350 ml;
- chewing thoroughly;
- slow walks after meals;
- enriching the menu with liquid cereals, low-fat soups, sweet fruits;
- refusal of solid, irritating foods, chemically and thermally aggressive products;
- maintaining the temperature of the dish - no higher/lower than 22 °C;
- abundant drinking regime. Water - slightly alkaline, without gas;
- last meal 3 hours before bedtime.
Medicines
For drug treatment of catarrh or another type of GERD, medications are required in accordance with the main causes of the pathology:
- for a bacterial infection, antibiotics are prescribed;
- in case of viral infection - antiviral and immunostimulants;
- when acidity decreases - antacids;
- to stabilize the production of acids in the gastrointestinal tract - histamine blockers and
- proton inhibitors;
- for chronic pathology - alginates to protect the mucosa.
- for severe pain - antispasmodics.
To reduce the factors causing superficial distal esophagitis, a number of antibiotics, hormonal, and anti-inflammatory drugs should be abandoned. GERD can be treated with the following effective drugs:
- "Omeprazole" is an antacid;
- "Motillium" is a prokinetic agent of the second generation.
Treatment regimens for ERE
There are two main treatment regimens for erosive esophagitis with GERD:
- when using the step up scheme, treatment begins with the weakest measures - lifestyle changes + antacids; if ineffective, PPIs are added, then prokinetics and only then PPIs.
- When using the step-down regimen, PPIs are immediately prescribed in full dose, symptoms are relieved, and then they are switched to weaker drugs.
Treatment of the disease for at least 6 weeks.
To prevent relapses, maintenance therapy is prescribed. Today, the most rational option is to prescribe PPIs in small doses.
Therapy methods
Treatment should begin only after the exact cause of the disease has been established. If you eliminate the root cause, then therapy will not be difficult . Sometimes the development factor cannot be determined, then doctors follow the usual treatment regimen. The following drugs are prescribed:
- Antifungal action.
- Enveloping the stomach and esophagus.
- Antispasmodics.
- Antacids.
In addition to drug therapy, there are techniques such as electrotherapy (amplipulse therapy) and mud therapy (peloid therapy). The main condition for effective treatment is strict adherence to therapeutic nutrition.
Diet
Therapy for this disease requires a complete change in diet. It is necessary to strictly exclude foods that irritate the esophageal mucosa and add dishes containing useful substances to the menu.
- cabbage;
- citrus;
- alcoholic drinks, sparkling water;
- tomatoes, various sauces;
- chocolate;
- various spices, herbs;
- smoked, vinegar, garlic;
- Tea coffee;
- fast food.
Anemia with reflux esophagitis
There are several causes of anemia in erosive reflux esophagitis:
- As a result of the inflammatory reaction in the process of reflux esophagitis, tissues are damaged, and therefore the vessels that feed them.
- Ulcers are deep defects in the esophageal mucosa, at first the bleeding from them is moderate, blood enters the lumen of the esophagus and then into the stomach, but without proper treatment, the ulcerative process tends to expand and deepen. By violating the integrity of a large vessel, an ulcerative defect can cause massive bleeding. Deepening of the ulcer can cause perforation of the esophagus and massive intra-abdominal bleeding and peritonitis.
- After healing, the ulcerative defect scars, being replaced by rough connective tissue. The wall of the esophagus ceases to be elastic and is easily injured when solid food passes, causing bleeding.
Chronic blood loss and developing anemia sharply reduce the body's regenerative potential and its protective properties.
Treatment of posthemorrhagic anemia is determined by the amount of blood loss and the state of the red blood (changes in the number of red blood cells, their size, the amount of hemoglobin they contain). For small and moderate blood loss, hemostatic agents, iron supplements, and vitamin complexes are prescribed. In case of massive blood loss, urgent resuscitation measures are required.
Treatment of ERE with traditional medicine (herbal medicine)
Herbal treatments are widely used in the treatment of GERD. This is especially justified in grade 1 erosive esophagitis, when the inflammation is catarrhal in nature and there are no gross organic and functional disorders. Herbal medicine presupposes the following rules:
- herbal treatment cannot replace full-fledged drug therapy, but can be used as an addition to the main treatment;
- herbal medicine has its own indications and contraindications;
- treatment with folk remedies can cause severe allergies; before you start using this or that herb, you need to make sure that you are not allergic to it;
- It is better to use familiar plants so as not to harm yourself.
For erosive esophagitis the following are used:
- Soothing herbs – valerian root, passionflower, spring adonis, lemon balm and mint.
- Enveloping agents – aloe juice, flax, plantain seeds, potato juice, propolis.
- Anti-inflammatory plants - St. John's wort, elecampane, bird cherry.