Despite the widespread prevalence of gastritis, a single generally accepted classification of the disease still does not exist.
This is primarily due to the variety of clinical forms of gastritis, which do not always correlate with morphological changes in the inner lining of the stomach detected during endoscopic examination. Let us consider the most relevant classification models today in the order of their development.
Flow options
All researchers recognize the division of gastritis into acute and chronic forms. Acute gastritis occurs against the background of an infectious process, food toxic infection when consuming poor-quality food, exposure to aggressive substances on the stomach - alcohol, large doses of medications, substances not intended for food. It develops quickly, its symptoms are pronounced: epigastric pain, vomiting, nausea, bowel dysfunction, fever, general malaise.
If gastritis is not treated properly, it becomes chronic. In the chronic course of the disease, the symptoms are more smoothed out, but disturbances in the gastric mucosa gradually progress. Chronic inflammation is associated with a disorder in the production of gastric juice, the bacterium Helicobacter pylori, and prolonged exposure to toxic substances on the gastrointestinal tract.
General classification
There are two main types of gastritis of the stomach. We are talking about acute and chronic. The first is divided into subspecies:
- catarrhal;
- phlegmonous;
- toxic-chemical;
- fibrinous.
Let's look at some of them separately below in the article.
Chronic gastritis is divided into the following forms:
- associated;
- autoimmune;
- chemically mediated;
- eosinophilic;
- idiopathic;
- granulomatous.
In addition to general divisions, there is a classification based on the formation of gastric juice. There are two types: with high and low acidity levels.
Chronic gastritis, in addition to the forms listed above, can acquire one of the following three: non-atrophic, subatrophic, mixed.
In addition, these types of illness easily turn into ulcers if the patient neglects treatment. If this happens, then the patient should be prepared for the formation of tumors. There is an additional classification of chronic disease. It is divided into three types: A (aka autoimmune), B, C (reflux gastritis).
Acute forms
A unified classification of acute gastritis has not yet been developed, so we will focus on the individual, most common types:
- Catarrhal is a shallow inflammation of the mucous membrane under the influence of poor diet, food poisoning, medication, and the development of allergies. The clinical picture is variable and depends on the cause of inflammation and the initial state of the gastrointestinal tract.
- Corrosive gastritis develops against the background of toxic chemicals entering the stomach - heavy metals, acids, alkalis. It is characterized by a rapid course, intense pain, a general serious condition, and the development of complications - bleeding, peritonitis.
- Acute stress inflammation is associated with the development of severe general illness: extensive burns, sepsis, traumatic brain or skeletal trauma, acute respiratory failure. In most cases, deep erosions appear in the gastric mucosa, which are complicated by bleeding.
New classification
According to the new classification developed by German scientists, the following forms of this disease are distinguished:
- autoimmune;
- Helicobacter;
- mixed;
- chemical-toxic;
- lymphocytic;
- special types.
At the present stage of medicine, an accurate diagnosis can be made thanks to a complete examination, correct test results and a detailed description of the disease. Most often in practice, doctors use the detailed classification of Ryss, and the other types of gastritis presented remain its addition.
Types of stomach inflammation according to Strickland and Mackay
This model was proposed in 1973. It takes into account the causes of the disease - etiology.
- Type A. This is an autoimmune inflammation triggered by the production of antibodies to the body’s own tissues, in this case to the epithelial cells of the stomach.
- Type B. The inflammatory reaction is caused by H. pylori, which mainly affects the antrum of the stomach.
- Type C. “Chemical” gastritis associated with exposure to alkaline duodenal contents (reflux gastritis) or with the damaging effect on the mucous membrane of certain medications (nonsteroidal anti-inflammatory drugs, hormonal medications).
Initial classification of the disease
The types of disease were first systematized in 1973. They were divided into three groups:
- A – autoimmune, in which the mucous membrane was affected in the stomach area.
- B – infectious, caused by the microorganism Helicobacter pylori.
- C – toxic-chemical, which occurs when the contents of the duodenum are transfused into the stomach or as a result of taking medications that corrode the mucous membrane.
A general classification of different forms (chronic, delayed) was created, defining the types of pathology, the causes of its occurrence, symptoms, and the course of the disease.
Sydney classification
This classification model dates back to 1990. It is considered expanded and takes into account not only the etiology of the disease, but also morphological changes.
By type of gastritis there are:
- spicy;
- chronic;
- special forms are a separate group of diseases caused by rare causes and having characteristic development mechanisms and course features.
“Special” forms include:
- lymphocytic;
- radiation;
- granulomatous;
- eosinophilic;
- hypertrophic;
- reactive;
- chemical;
- infectious lesions not associated with Helicobacter.
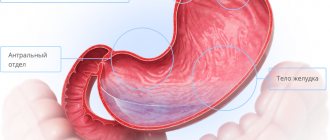
According to the localization of the inflammatory process, they are distinguished:
- antral gastritis (inflammation of the lower third of the stomach);
- inflammation of the body (middle part) of the stomach;
- pangastritis (the entire mucous membrane of the organ is involved in the process).
Morphological changes involve assessment of the following parameters:
- activity of the inflammatory process;
- degree of inflammation;
- atrophy of the glands of the mucous membrane;
- their metaplasia;
- detection of H. pylori bacteria in stomach tissues.
According to etiology, gastritis is of 2 types:
- infectious nature associated with H. pylori;
- non-infectious, caused by exposure to alcohol, chemical agents, consequences of surgery on the stomach, development of an autoimmune reaction.
Morphological gradation of atrophic gastritis
Within the framework of the Sydney classification, 2 fundamentally different forms of atrophic inflammation are considered separately: metaplastic and non-metaplastic. Atrophy is the irreversible loss of gastric glands. When the inflammation is non-metaplastic, connective tissue takes the place of the glandular tissue. The metaplastic variant is considered more dangerous due to the risk of developing cancer. In this case, the gastric glands are replaced by similar structures of the intestinal mucosa or pylorus.
If atrophy is present, it is assessed on a three-point scale:
- Minor - less than 30% of glandular tissue is lost.
- Moderate – loss of glands is 30-60%.
- Severe – more than 60% of the glands are missing.
Such severity criteria are similar for metaplastic and non-metaplastic atrophic gastritis.
Peculiarities. There are known cases of false atrophy, when islands of intestinal epithelium “push apart” the gastric glands and are embedded between them. At the same time, the amount of glandular tissue does not decrease. Such a diagnosis can only be made by taking biopsy material from the stomach over time several times and monitoring its changes during treatment.
Gastritis according to ICD-10
Duodenitis and gastritis in this classification are under diagnosis code 29 or simply K29. Here are the main diagnosis codes for most types of gastritis in ICD-10:
- ICD-10 code 29.0 – Acute hemorrhagic;
- K29.1 – Other types of gastritis (acute);
- K29.2 – Alcoholic;
- K29.3 – Superficial chronic;
- K29.4 – Chronic atrophic (atrophy of the gastric mucosa occurs);
- K29.5 – Unspecified chronic (fundic, antral);
- K29.6 - Other chronic types (hypertensive, Giant granulomatous, Menetrier's disease);
- K29.7 – Unspecified gastritis;
- K29.8 – Duodenitis;
- K29.9 – Unspecified gastroduodenitis.
In addition to ICD-10, several more classifications of gastritis can be distinguished. Let's look at the two most modern of them.
Sydney classification of gastritis
It was created in the 1990s with the participation of gastroenterologists, pathologists, microbiologists, histopathologists and immunologists. The Sydney classification is itself divided into two sections:
- Histological . Consists of etiology, morphology and topography. According to etiology, there are different forms of protracted gastritis, such as autoimmune, Helicobacter, reactive and special forms of the disease. According to the typography of the inflammatory process in the stomach itself, types such as pangastritis, a disease of the body of the stomach and antrum, are distinguished. Regarding the morphological part of the diagnosis, we can say that it is always associated with specific parts of the stomach. There are three main types of morphological changes, which include chronic, acute gastritis, as well as special forms of the disease.
- Endoscopic . This section is characterized by swelling and severe hyperemia of the gastric mucosa. In addition, there are erosions and hemorrhages, hyperplasia of the folds.
Classification of gastritis OLGA
This is a completely new system that was proposed by a group of experts from renowned pathologists and several clinical gastroenterologists in 2008. The OLGA gastritis classification uses an assessment of the histological severity of necrosis of the mucous membrane, inflammation in the body of the stomach, as well as in the antrum, with further determination of the stage and degree of chronic gastritis.
Note that the OLGA system has two big advantages:
- determination of the stage of atrophy, which makes it possible to objectively determine the presence and severity of the spread of inflammation;
- determination of the stage of atrophy based on the results of treatment.
Houston classification of chronic gastritis
This is a kind of addition to the 1996 Sydney system that further details it.
- Non-atrophic gastritis , similar to type B. Can be caused by any factors, including H. pylori. The only condition is a normal amount of glandular epithelium.
- Atrophic autoimmune process corresponding to type A.
- Atrophic multifocal , which develops under the influence of several pathological factors at once.
- “Special” forms of gastritis.
The disadvantage of this gradation was considered to be ignoring the level of acidity of gastric juice and the characteristics of the clinical picture of the disease.
Third degree gastritis
Atrophic gastritis – the most severe stage 3. Deep damage occurs to the superficial tissues down to the muscle plate layer. As you know, muscles contain blood vessels, veins, and nerve endings. This stage, which is extremely painful for the patient, is dangerous because as a result, the atrophied cells of the mucosal surface begin to be replaced by the thick intestinal layer. Many ulcers, cysts, and adenomas form, taking a malignant form. The stomach ceases to fulfill its main purpose - digesting food.
The patient experiences:
- constant pain;
- food obstruction;
- sudden loss of body weight;
- chronic heartburn and belching;
- weakness to the point of dizziness;
- diarrhea and vomiting.
Due to disruption of the digestion process of stage 3, food stagnates. The bacteria Helicobacter pylori in disturbed acidity begin to develop actively, producing alkali and toxins that can disable the body.
Urgent measures are required: antibacterial therapy, a strict diet, medications that help restore the functioning of organs and maintain the health of other body systems, resorption therapy. Urgent surgery is possible.
Kyoto classification
The Kyoto system of dividing diseases into types (2014), which is based on the etiological principle, is considered the most extensive and universal.
- Helicobacter-induced gastritis.
- Drug-induced.
- Autoimmune.
- Stressful.
- Special forms:
- allergic;
- reflux gastritis;
- lymphocytic;
- eosinophilic;
- Ménétrier's disease.
- Infectious gastritis:
- viral (entero- or cytomegalovirus);
- fungal (candidiasis, mucormycosis, histoplasmosis);
- bacterial (infection with H. pylori, enterococci, Treponema pallidum, mycobacteria);
- gastric phlegmon (purulent melting of the organ wall);
- parasitic (anisakiasis, strongyloidiasis, cryptosporidiosis).
- Gastritis caused by other diseases - ulcerative colitis, Crohn's disease, vasculitis, sarcoidosis.
- Gastritis due to physical and chemical factors:
- radiation;
- alcoholic;
- chemical;
- other.
According to modern ideas, it is the Kyoto classification that should be included in ICD-11.
Types and groups of gastritis in the stomach
Gastritis is a chronic disease with characteristic periods of exacerbations and remissions. Characterized by damage to the gastric mucosa. There are many types of gastritis of the stomach; treatment tactics for each type differ.
A lot of ideas have been proposed to divide gastritis into groups. The division is still highly controversial. The classification of inflammation of the mucous layer is now based on the criteria of origin, location of the defect in the stomach, and morphology. With each new discovery, more species are added to the classification, and the scheme is updated. The most common classification that doctors use in practice to formulate a diagnosis is the working classification of gastritis. Treatment is based on the data of this classification.
The very first classification of chronic gastritis
The first systematization of chronic gastritis represented a group of three types of gastritis, proposed in 1973. Included types of stomach diseases:
- Autoimmune (Type A) - characterized by damage to the mucous membrane within the body of the stomach.
- Infectious (Type B) – characterized by damage to the mucous membrane due to infection by Helicobacter pylori.
- Toxic-chemical (Type C) - characterized by damage to the gastric mucosa, the causes of which lie, firstly, in the formation of reflux of contents from the duodenum into the stomach, and secondly, by taking medications that have a detrimental effect on the mucous membrane of the gastric wall.
Sydney classification
The second in origin and first in importance is the classification of chronic gastritis, adopted in Sydney in 1990. This includes the following headings: classification according to the volume of the lesion, the speed of clinical development, the morphological structure of the defect, and its origin.
Each section includes many subsections. In order to correctly and completely make a diagnosis and prescribe treatment, it is necessary to take into account all the headings. Let's sort it out in order.
Speed of development of the clinical picture
This classification represented the division of gastritis into main types according to the severity of symptoms and clinical picture. Diseases were divided into acute (suddenly appearing complaints in the form of epigastric pain, nausea, forcing a person to take a forced position, the causes were in diet errors), chronic (developing over years, when the clinical picture is not expressed or the person is not bothered by pain at all) and other forms. Other, or special, forms included types: granulomatous, reactive, lymphocytic and others.
Volume of lesion
The Sydney classification included a division according to the anatomical region in which the lesion occurred: gastritis of the body of the stomach, antrum, or pangastritis (when the entire hollow organ is involved).
Morphology
According to changes in morphology, the classification of chronic gastritis included: atrophy, metaplasia. The degree of inflammation was described. If this is a superficial form (within the mucous membrane of the gastrointestinal tract), it is indicated: when exudate is released - exudative. If there is no exudate, only hyperemia, the erythematous form is evident. The shape of the erosions is also described: whether they are flat or raised, whether hemorrhages or hyperplastic cells are present. Is gastroesophageal reflux associated? All of the above can be described using endoscope visualization.
Etiology
According to the factor of origin of the disease: H. pylori positive (infectious) and non-infectious causes: conditions caused by excessive use of non-steroidal anti-inflammatory drugs, alcohol. Autoimmune aggression against stomach cells. Exposure to chemicals.
The diagnosis of chronic gastritis is based on all four signs: the presumed cause of the disease, the location of the defect, histo- and macroscopic changes in the membrane.
Visual scale
The advantage of the Sydney classification is the presence of a visual analogue scale, which includes the degree of severity of morphological and histological changes in the mucosa. Signs are assessed using a point system. 0 – no changes, 1 – minimal manifestation, 2 – moderate manifestation of the symptom, 3 – significantly expressed manifestation.
Houston classification of chronic gastritis
A little later in 1994, the Sydney classification was changed. The results of the changes were published two years later. They concerned a targeted study of the results of a biopsy of the obtained material. One is from the corner of the stomach, two others are from different parts of the body of the stomach, and two more are from the antrum.
The classification is considered more advanced, but many critics point out that it lacks an important criterion: an indication of the presence of high or low acidity. Although the prevention of acidity disorders is the basis for the treatment of hyperacid and hypoacid conditions.
Types of disease
The varieties of chronic gastritis of the latest classification include the species listed in the first Sydney classification. The difference lies in the completeness of information and the inclusion of a number of new types of pathology.
- Non-atrophic type - the etiological factor is primarily considered to be infection of the mucous membrane by the bacterium Helicobacter pylori. In previous classifications, the type was called superficial, antral chronic, with increased secretory activity, type B.
- Atrophic autoimmune type - the occurrence of the type is associated with immune mechanisms of action on the gastric mucosa. Previous classifications were called: type A, diffuse gastritis of the body.
- Atrophic multifocal chronic type - the cause of the pathology lies in infection with Helicobacter pylori, errors in diet, pagnum exposure to the environment. In the first classifications it was called a mixed type (A+B).
Special forms of gastritis
- Chemical type - occurs as a result of irritation of the gastric mucosa due to the action of bile on it (with reflux from the duodenum) or the action of drugs, for example: nimesulide from the NSAID group and their effect manifests itself after long-term use of drugs in a large dose. In the first classification, type C gastritis is called.
- Radiation type - occurs when exposed to radiation damage.
- Lymphocytic type - the causes of the occurrence are completely unknown, but the culprits are considered to be Helicobacter pylori, the influence of immune mechanisms directed against the cells of one’s own body, and gluten intolerance.
- Granulomatous type - occurs against the background of Crohn's disease, sarcoidosis, Wegener's disease, long-term presence of foreign bodies in the gastric mucosa.
- Eosinophilic or allergic occurs against the background of food allergies.
- The giant hypertrophic appearance is manifested by Ménétrier's disease. The causes of the disease have not been fully elucidated. For unknown reasons, the gastric mucosa is transformed into cysts and adenomas located on the entire surface of the mucous layer. The disease manifests itself in adulthood. Patients are concerned about sudden weight loss, vomiting, loose stools with bloody feces, pain in the area of the xiphoid process of the sternum. As a rule, the disease progresses slowly. There are rare cases of pathology occurring in childhood.
Working classification
Taking into account the shortcomings of all the listed classifications, new types of chronic gastritis have been introduced. Classification imperfections were taken into account:
- Lack of description of the course and occurrence of the disease: acute, chronic;
- The classification does not include complications of gastritis;
- There are no indications of deviations in the secretory activity of gastric juice, which affects the occurrence of gastritis, erosions and ulcers, or the preference of treatment.
Atrophic gastritis
Atrophic gastritis is one of the extremely unfavorable types and is considered a precancerous disease. With this type, cells lose the ability to adequately perform functions, gradually losing their normal structure and becoming flattened. Dangerous due to probable degeneration into cancer, sluggish course, poor clinical picture, which prevents timely diagnosis of the pathology. Why does this happen?
Stage 1 of pathogenesis is the same for the disease: all types of inflammatory process on the mucous membrane begin from this stage. Cells of the gastric mucosa are exposed to Helicobacter pylori, and under their influence, the environment changes to a more acidic side in a certain place in the stomach. The basis is created for further progression of the disease.
Stage 2 involves the body's autoimmune action against its own lining cells of the stomach, they stop functioning. Cells with an altered structure can no longer regenerate. The function is leveled, hydrochloric acid for gastric juice is not produced. Only mucus is produced, which, in turn, covering the walls of the stomach, protects it for some time from harmful influences. When examined with a fibrogastroscope, an inexperienced eye may miss areas of atrophy under a thick layer of mucus. With subsequent growth, atrophic cells develop, completely filling the gastric mucosa, and become unable to perform the main function of digesting food. The cells hypertrophy and turn into cancer cells.
The atrophic subtype is divided into: superficial; antral; focal; acute and chronic atrophic gastritis; moderately atrophic gastritis.
Non-atrophic gastritis
As stated above, a common cause of the disease is Helicobacter pylori infection. Sources include: gastric surgery, immune system disorders, bacterial contamination, alcohol abuse. It is noted that this is the most common and “harmless” type of gastritis.
The disease manifests itself with complaints of heartburn, taste in the mouth, pain and heaviness in the epigastric region after the next meal. With timely diagnosis, the disease can be quickly cured without residual effects.
For prevention, it is possible to use bifiform capsules, which normalize the balance of microflora.
Special forms
Includes a list of species that did not find a place in other sections: eosinophilic, reactive, radiation and others.
Localization of gastritis
Location in the area of the body of the stomach, antrum or both parts, covering both curvatures of the stomach. Prevention of gastritis and timely treatment is necessary so that the lesion does not spread over the entire surface of the stomach.
Cause of the disease:
- Infectious lesion of the mucous membrane caused by Helicobacter pylori;
- Other factors of a non-infectious nature: exposure to alcohol, chemicals (medicines), radiation injuries, allergic reactions to food, gross disturbances in diet, frequent reflux of intestinal contents into the stomach;
- Autoimmune aggression against the body's own cells;
- Other unknown factors.
Endoscopic picture of the lesion
- Exudative or superficial is a common option;
- Erosive;
- With atrophy of the mucous membrane;
- Chronic with hemorrhages;
- With areas of metaplastic epithelium;
- Hyperplasia of the gastric mucosa;
- The presence of the picture and consequences of reflux disease.
According to clinical manifestations
According to the clinic, chronic gastritis is divided into 2 phases: exacerbation and remission. In turn, the classification of the acute variant includes the following types: catarrhal gastritis, characterized by an abundant amount of mucus covering the walls of the stomach, swelling and congestion of the lining cells of the stomach. If there are small hemorrhages against this background, it speaks of another type of acute gastritis - erosive.
Fibrinous gastritis is manifested by the presence of purulent discharge on the surface of the mucosa with small fibrous connective tissue strands. Types of inflammation of the mucous layer include 2 types: superficial, or croupous, gastritis, which is distributed within only the superficial layer. Deep, or diphtheritic, in which strands of connective tissue invade the other linings of the stomach, leaving deep scars.
Acute phlegmonous type - characterized by the involvement of all layers of the stomach with the formation of necrosis and deep ulcers. Prevention of the disease and timely treatment will help avoid severe manifestations.
Gastritis? Ulcer? To prevent a stomach ulcer from turning into cancer, drink a glass...
The best FOLK remedy for GASTRITIS and stomach ulcers!
By stomach function
- Gastritis with normal secretory activity;
- Hyposecretory type;
- Hypersecretory type.
According to the morphological picture
The section includes a description of the gastric wall according to what was seen during FGS. Treatment and further tactics, to a large extent, depend on the description. The degree of inflammation, its activity are described, areas of atrophy of the gastric glands, if any, are indicated. Metaplasia and its type. The degree of Helicobacter pylori contamination of the gastric mucosa.
According to the presence of complications
Complications occur in advanced cases, with untreated gastritis, and are of two types:
- Bleeding from erosions, ulcers of the gastric mucosa.
- Malignization.
Formation of diagnosis
The diagnosis includes all points of the classification. Therefore, after the word gastritis, the patient sees many unfamiliar words. Chronic gastritis, the classification of which is reflected in the diagnosis, helps the doctor decide on further treatment and observation tactics. If there are manifestations of precancer or stomach cancer, a decision is made on surgical intervention.
Treatment for gastritis should only be prescribed by a doctor; if the treatment is incorrectly prescribed, there is a high risk of aggravating the course of the disease. If treatment is not stopped in a timely manner or the measures recommended by the doctor are not followed, the cells of the gastric mucosa reduce their functional activity and gradually atrophy, leading to malignancy. The causes of gastritis, as stated above, are multifaceted; only a doctor has the right to prescribe the correct etiotropic and pathogenetic therapy. Treatment includes diet, prescription of antibacterial drugs to destroy Helicobacter pylori, and proton pump inhibitors. You can also use the probiotic bifiform to normalize the intestinal microflora after taking antibiotics.
Other forms of stomach inflammation
All of the listed classification systems do not take into account the clinical picture of the disease and the variants of hydrochloric acid secretion. Therefore, additional gradations appear in the working classification of gastritis.
According to the type of secretion of hydrochloric acid:
- normoacid gastritis – medium acidity;
- hyperacid – excessive production of HCl;
- hypoacid – lack of hydrochloric acid;
- anacid - complete cessation of its secretion.
According to the severity of symptoms:
- exacerbation phase;
- remission phase.
According to the presence of complications:
- bleeding;
- malignancy – malignant degeneration.
Thus, the diagnosis of gastritis is formulated taking into account the etiology, mechanism of disease development, endoscopic and clinical picture.
Note. The classification of gastritis for adults and children is the same. Only the prevalence of one form or another of the disease differs. For example, atrophic inflammation and hypoacid gastritis are much less common in children. But hyperacid gastritis, reflux gastritis, and erosions of the mucous membrane are characteristic of childhood and adolescence.
Hyperacid and normoacid gastritis
With preserved or increased secretory function, the disease can be divided into dyspeptic, mixed and painful forms. Disorders of other digestive organs are rarely detected during hyperacid and normoacid inflammation. If reduced secretion is observed more often in older people, then the contingent of increased and normal secretion is different - these are people of working age, from 30 to 40 years.
Clinical manifestations
Patients do not develop an aversion to food. Rather, there is a good or even increased appetite. The main complaints are related to dyspepsia - patients complain of sour belching, frequent heartburn, and a burning sensation in the stomach. The pain syndrome is not as intense as with an ulcer, but is still present. Pain of varying intensity occurs 30–40 minutes after eating, less often on an empty stomach.
Pain and dyspeptic symptoms can occur simultaneously or in isolation. The disease is characterized by alternating remission and exacerbations. In remission, pain and dyspeptic symptoms occur only with dietary violations and are mild. During an exacerbation, the clinical picture is very expressive: severe pain, persistent heartburn, nausea and heaviness are present daily. Manifestations of the disease must be differentiated from peptic ulcer disease.
Often, patients with high acidity develop neurasthenic syndrome. Exhausted by illness, the patient becomes moody, irritable, gets tired quickly, and suffers from headaches.
Hyperacid gastritis with regular diet violations can transform into peptic ulcer disease. To prevent this from happening, you must carefully follow all medical recommendations.
Treatment
Comprehensive treatment of hyperacid and normoacid gastritis begins with nutritional recommendations. The diet includes serious restrictions that must be observed to prevent exacerbations. During an exacerbation, the patient is prescribed fasting, and the diet is gradually expanded. Restrictions are removed gradually so as not to injure the inflamed mucosa. The diet during an exacerbation should be as gentle as possible.
Drug treatment is selected by a gastroenterologist. Prescribed drugs to reduce acidity, enzymes, antacids, antispasmodics. When Helicobacter is detected, eradication therapy is used.
Low-carbon mineral water is recommended an hour and a half before meals, warm. The course of treatment with mineral water lasts from 21 to 24 days.
Balneotherapy, therapeutic exercises, physiotherapy, herbal medicine are prescribed outside of exacerbation.
How to determine the type of gastritis
You won't be able to make a diagnosis yourself. Even an experienced doctor, therapist or gastroenterologist will not be able to determine the type of gastritis by eye. The problem is that many types of inflammation clinically occur in the same way, and sometimes even occur in a latent form.
For this reason, to clarify the diagnosis, an additional examination is always prescribed: fibrogastroduodenoscopy (FGDS) with collection of gastric contents and biopsy material for analysis.
This is how the type of hydrochloric acid secretion, structural changes in the inner membrane and the presence of H. pylori are determined. The choice of treatment tactics directly depends on the type of pathological process.
The main types of chronic gastritis according to ICD 10
Acute hemorrhagic (erosive) Code 29.0
Pathology is a type of inflammatory process on the surface of the stomach cavity. The peculiarity of the disease is that the beginning is not the formation of an inflamed area, but microcirculatory disorders in the vessels of the submucosal surface. Next, they provoke hemorrhages, gradually permeating the upper layer of the cavity. As a result of disturbances in the vessels of the stomach wall, blood clots can occur, which causes acute gastritis, inflammatory processes and erosion. This disease is also called hemorrhagic erosive gastritis.
Other types of gastritis (acute type) Code 29.1
This type of pathology is caused by short-term exposure to an aggressive environment, which can be poor quality food, medications, etc.
Depending on the type of damage to the mucosa, as well as the characteristics of the clinical signs, gastritis can be:
- catarrhal;
- fibrinous;
- corrosive;
- phlegmonous.
Alcohol Code 29.2
In accordance with ICD10, such gastritis does not occur against the background of an inflammatory process. Acute gastritis, in which there is damage to the inner lining of the stomach, is formed as a result of prolonged alcohol intake and is often accompanied by erosions.
Under the influence of ethanol, the production of hydrochloric acid increases, which gradually corrodes the walls of the stomach, thus disrupting their structure and making it impossible to fully carry out their functions.
In this case, the blood circulation process is completely disrupted, the production of protective mucus is inhibited, which prevents the restoration of cells in the gastric mucosa.
Superficial chronic Code 29.3
Pathology is considered the most easily form, which is often diagnosed among patients. Untimely or poor quality treatment threatens this form to develop into a more complex pathology. The superficial type occurs only in the outer lining layer, without destroying the deeper levels of the gastric mucosa.
Chronic atrophic Code 29.4
Chronic gastritis according to ICD 10 is an inflammatory process in the mucous layer of the stomach, which provokes its thinning. As a result of such destruction, the production of gastric secretions decreases, and there are also significantly fewer epithelial cells involved in the regeneration of the mucosa. Against this background, secretory insufficiency of the gastric cavity is formed.
Unspecified chronic Code 29.5
According to the ICD 10 classification, this type of gastritis has two forms:
The antral type is characterized by localization of the inflammatory process in the lower part of the stomach, called the antrum. This part contains glands that produce the digestive hormone gastrin. Through it there is a powerful effect on hydrochloric acid. In case of its deficiency, increased acidity occurs, which causes an inflammatory process on the walls of the stomach. The disease in most cases becomes chronic.
Acute gastritis of the antral type most often occurs as a result of food intoxication, severe malnutrition and food or drug allergies.
Fundal gastritis develops in the upper and middle zone of the gastric cavity. It is in this part that the digestive glands are located, the purpose of which is to produce hydrochloric acid. In case of partial loss of the digestive glands of their functions, the antrum retains its structure.
Useful video
Is poor nutrition always the cause of gastritis? We invite you to watch the video and find out what factors can provoke the development of the disease.
The classification of gastritis is complex and multifaceted. In most cases, there is no need for the patient to thoroughly understand all variants of the course of the disease. It is important to find out what reason provoked the development of gastritis in his case, and direct all efforts to combat this factor. Therefore, you need to promptly seek medical help and follow all doctor’s instructions.