Consultation with a proctologist – 1,750 rubles.
- What is paraproctitis (rectal fistula)?
- Symptoms of paraproctitis
- Types and stages of the disease
- Diagnosis of rectal fistulas
- Treatment of paraproctitis
- Surgery
- Main risks
- Prevention
- Popular questions
Chronic paraproctitis (rectal fistula)
– a chronic inflammatory process in the anal crypt, intersphincteric space and pararectal tissue with the formation of a fistulous tract. The affected crypt is the internal opening of the fistula.
According to statistics, most patients with rectal fistulas associate the occurrence of the disease with acute paraproctitis. About a third of patients with acute paraproctitis consult a doctor after spontaneous opening of an abscess, after which in most cases a rectal fistula is formed. Approximately half of the patients with acute paraproctitis undergo radical surgery at the time of treatment, the other half only undergo opening and drainage of the abscess without eliminating the entrance gate of the infection, which can subsequently lead to the formation of a rectal fistula. In this case, constant infection occurs from the intestinal lumen, and a fistula tract is formed from scar tissue. The external opening of the fistula is most often localized on the skin of the perineum, its diameter is often no more than 1 mm. If the fistula tract is insufficiently emptied, purulent cavities may form along its length.
The prevalence of chronic paraproctitis reaches 23 cases per 100,000 population, the proportion among rectal diseases reaches 25-30%. Males are more susceptible to this disease than women; the disease more often manifests itself in young and middle age Source: Khomochkin V.V. Operation of ligation of the fistula tract in the intersphincteric layer in the treatment of chronic paraproctitis / V.V. Khomochkin [et al.] // News of surgery. - 2021. - T. 26. - No. 5. - P. 616-623. .
Symptoms of paraproctitis
Symptoms directly depend on where the fistula is located and the state of the patient’s immunity.
Usually, after an illness, a person experiences pain in the anus and a hole appears from which pus comes out. This causes itching, irritation, and bad odor. Sometimes ichor is released along with pus. This occurs when blood vessels are damaged. If the fistula has no outlet, then patients complain only of pain and/or discharge from the rectum or vagina.
An incomplete internal fistula provokes a sensation of the presence of a foreign body in the anal area. If the infiltrate does not leave the fistula cavity enough, the following symptoms appear:
- discomfort and pain in the anal area;
- retention of urination and defecation;
- discharge of mucus, infiltrate, pus from the rectum;
- increased body temperature, chills;
- redness and irritation of the skin around the anus and part of the buttocks.
Chronic paraproctitis during the period of exacerbation gives the following symptoms:
- fast fatiguability;
- sleep disturbance;
- nervous exhaustion;
- headache;
- regular increase in body temperature;
- intimate disorders;
- gas incontinence.
Physiological changes may occur:
- anal deformation;
- disruption of the anal sphincter;
- scars on the muscle tissue of the anal sphincter.
During periods of remission of chronic paraproctitis, the general condition is normal; with proper hygiene, the quality of life is almost not reduced. But with a long course of the pathology and frequent exacerbations, the following may occur:
- sleep disorders;
- powerlessness, weakness;
- headache;
- periodic changes in body temperature;
- nervousness;
- poor work ability;
- deterioration of potency.
Reviews and conclusions
Patient B.: “About a year ago, pain appeared in the anus and the temperature rose. The pain was severe enough that I could not sit. But he didn’t go to the doctor, he treated himself - suppositories for hemorrhoids, chamomile baths, painkillers. A week later the abscess opened, a lot of pus came out, I felt better, I was happy.
About a month later I began to notice that my perineum was constantly wet, there was discharge on my underwear, and an unpleasant odor. I waited another two months, hoping that everything would go away on its own. In the end I decided to see a doctor. A rectal fistula was diagnosed.
For a long time he did not agree to the operation; he was treated with various folk remedies. However, there was no effect; pain began to appear periodically.
The operation took about an hour. A few days in the hospital, then I did the dressings myself at home, it’s not difficult. After 10 days, practically nothing bothered me.”
The bulk of rectal fistulas are a consequence of untreated acute paraproctitis.
Rectal fistula is not a fatal disease. You can live with it, but the quality of life is significantly reduced.
Types and stages of the disease
Rectal fistulas can be complete, incomplete, or internal.
- Complete ones
have two openings - located inside and opening into the rectum, as well as external, usually located next to the anus. - An incomplete fistula
has only an internal opening that opens into the rectum. There is an opinion that this is a transitional phase, because sooner or later the external opening will open and the fistula will become complete. - An internal fistula
has two internal openings that extend into the lumen of the rectum.
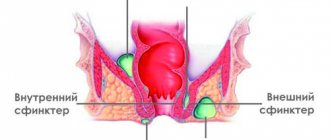
According to their location relative to the anal sphincter, fistulas are divided into:
- Intrasphincteric
, or marginal. The most common ones usually have a straight course without scars and an external opening near the anus. - Transsphincteric
- the course of such a fistula goes through the anal sphincter at different depths. The higher the course, the more it branches and the more often purulent streaks form, and scar tissue forms around the fistula itself. Scars can deform the anal sphincter and interfere with its function. - Extrasphincteric
- differ in the location of the internal opening - on the surface of the intestinal crypt. The stroke itself passes high and goes around without affecting the outer pulp. The incidence of such fistulas is 15-20% of the total incidence.
Extrasphincteric fistulas are usually tortuous and have a long course. With them, purulent leaks form and scars form around the fistula canals. With repeated exacerbations, new external openings appear. There is a classification that distinguishes four degrees of complexity of fistulas of this type:
- – there are no scars around the internal opening, the course is straight, infiltrates and purulent streaks do not form in the perirectal tissue.
- – scars appear around the internal opening, there are still no ulcers or infiltrates.
- – the entrance to the fistula canal is narrowed, there are no scars, there are ulcers and inflammatory infiltrates in the perirectal tissue.
- – the inlet is enlarged, surrounded by multiple scars, and there are ulcers and infiltrates in the tissue.
Why is excision of a fistula performed for paraproctitis?
The formation of a fistula tract is a passage that forms between the soft tissues of the anus and the rectum. As a rule, it appears during a purulent and infectious process. Externally, the fistula tract looks like a narrow canal, which is covered with epithelium. It has an exit and an entrance in the form of inflamed wounds. At the same time, the edges are compacted.
When the patient managed to eliminate the inflammatory process, the abnormal passage still remains open. The wound bleeds, mucus, pus and other discharge with an unpleasant odor are released from it. Soft tissues become irritated, inflamed, and pain appears. In some cases, an allergic process develops.
In the absence of timely diagnosis and treatment, the anus becomes deformed, anal fissures, scars and other changes appear. The pathology develops into malignant and poses a danger to the health and life of the patient. Drug treatment eliminates unpleasant symptoms, but does not eliminate the causes of the disease. For this purpose, surgery is performed. Excision of rectal fistula has extremely positive reviews. The risk of relapse is reduced to zero.
Methods for diagnosing rectal fistulas
In the vast majority of cases, the diagnosis is not difficult to make. The proctologist is based on the patient’s complaints, examination and palpation data. Usually, during a digital examination, the doctor discovers holes in the anal area, from which pus comes out when pressed.
When diagnosing and subsequent treatment of rectal fistulas, the determination of the fistula tract is of fundamental importance. For this purpose, digital and mirror examination of the rectum, probing and examination of the fistulous tract with a dye solution, anoscopy or sigmoidoscopy, fistulography, ultrasound, CT, MRI are used Source: Seidova K.R. Etiopathogenesis and diagnosis of pararectal fistulas. Literature review / K.R. Seidova // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. - P. 23-27. .
One of the main methods for studying pararectal fistulas is probing. With the help of probing, along with the internal opening of the fistula, it is possible to determine the depth of the fistula tract, its connection with the intestinal lumen, the relationship of the fistula to the anal sphincter, and by the movement of the tip of the probe in the canal, bay-shaped expansions and additional branches.
Examination of the rectum using a speculum and proctoscopy allows one to distinguish between altered crypts and the internal opening of the fistula. Injecting a dye into the external opening of the fistula allows you to more clearly distinguish the internal opening. For this purpose, a 1% aqueous solution of methylene blue, iodine, ink, manganese and other solutions are used.
Restoromanoscopy is an endoscopic technique that involves inserting a special tube equipped with optics into the anus. The doctor can assess the condition of the mucosa and do a biopsy to rule out a tumor if one is suspected.
Fistulography is a radiopaque technique. A contrast agent is injected into the anus, and then x-rays are taken. X-ray examination reveals the presence of pockets, cavities, extensive bays, additional branches and curved fistula tracts.
Transrectal ultrasound allows us to trace the fistula tract in the pararectal tissue, the presence of additional cavities along the course, the relationship of the fistula to the anal sphincter, determination of the internal opening of the fistula, differentiation from pararectal neoplasms. Ultrasound examination is also informative in determining anal sphincter insufficiency after surgery in patients with perirectal fistulas.
Women must receive a referral to a gynecologist for examination to rule out a vaginal fistula.
Treatment
Patients with diagnosed rectal fistula are prescribed surgical intervention. It is impossible to get rid of the pathology with the help of conservative therapy. During the operation, experienced proctological surgeons at the Yusupov Hospital excise the fistula and eliminate the internal opening.
For each patient, a unique treatment tactic is developed taking into account the localization of the fistula tracts, the nature of scarring, the presence of infiltrates and abscesses along the fistula in the cellular space and pararectal area, as well as many other individual factors.
When choosing a method of surgical treatment, the nature of the rectal fistula, the duration of its existence and the presence of inflammation are taken into account.
Patients in the proctology department of the Yusupov Hospital are primarily prescribed anti-inflammatory and antibacterial therapy; it is also necessary to rinse the fistula cavity. After the acute symptoms subside, they begin surgical intervention, during which the fistula tract is excised, the fistula is dissected, and the fistula opening is closed using various methods.
The use of an innovative technique is highly effective - sclerotherapy, during which solutions are introduced into the lumen of the fistula, thanks to which the walls of the fistula stick together and close.
Thanks to the use of basic and modern techniques, the availability of the latest medical diagnostic equipment and extensive practical experience, doctors at the proctology department of the Yusupov Hospital manage to achieve impressive results in the treatment of patients with incomplete rectal fistula. Each patient of the clinic undergoes high-quality diagnostics, an individual treatment regimen is developed, and the progress of the rehabilitation period is monitored.
When performing all medical procedures, painkillers are used; in difficult cases, anesthesia is used, so before visiting the doctor’s office, patients are devoid of fear and do not experience pain during the procedures. The clinic has all the necessary medical equipment, including the latest generation laser equipment.
The popularity of the Yusupov Hospital in Moscow is determined by its fair pricing policy, highly qualified doctors, and the sensitivity and friendliness of all medical staff.
Treatment methods for paraproctitis
Complete cure is only possible through surgery. Physical therapy, antibiotics, and ointments are used in preparation for or after surgery. Drug therapy can also relieve symptoms and speed recovery. Main recommended pharmacological groups:
- painkillers;
- systemic antibiotics;
- healing ointments.
A course of physiotherapy may include ultraviolet irradiation and electrophoresis.
SM-Clinic specialists diagnose and treat complex pathologies. To make a diagnosis, the doctor collects the patient’s complaints, medical history and objective examination. To clarify the diagnosis and carry out differential diagnosis, additional instrumental studies are performed, such as anoscopy and sigmoidoscopy. These studies are carried out after cleansing the intestines by performing cleansing enemas and taking laxatives.
Operation
Surgical treatment consists of excision of the fistula, as well as drainage of abscesses. During excision, it is important not to touch healthy tissue and be extremely clear - limit yourself to the affected area. The operation to remove a rectal fistula is performed under general anesthesia and is painless for the patient, which cannot be said about the postoperative period.
Video
This operation can also be performed with a laser. This will take less time and reduce the risk of infection; the patient will be able to return to their normal lifestyle in the very next few days. However, such an operation is more expensive.
The postoperative period is an important part in the recovery process and prevention of relapses.
At this moment you need to adhere to the rules:
- in the first three days there was no bowel movement, so the patient practically cannot eat, he can only drink decoctions and water, and glucose is administered intravenously. This is done to prevent injury to the closed canal with feces.
- food was then liquid and in small portions, so that the feces were soft and did not injure the intestines;
- the patient kept to bed rest and did not lift heavy objects;
- Dressings were performed regularly; you can use an ointment with an anesthetic effect to relieve pain after surgery.
Treatment takes about two weeks, to avoid relapse of the disease, you need to establish what causes the fistula in this case, and try to avoid this factor, or treat the existing disease that provokes this phenomenon.
Surgical treatment of pararectal fistulas
The only indication for surgery is the presence of a fistula.
Contraindications:
- general serious condition of the patient;
- liver and kidney failure;
- chronic diseases in the stage of decompensation;
- blood clotting disorder;
- acute infections in the body.
The operation is usually carried out as planned. In case of exacerbation, the abscess is opened, and the fistula itself is removed after 1-2 weeks.
Preparation for surgery includes standard preoperative examination: blood tests, urine tests, ECG, fluorography. Additionally, rectal examinations and/or ultrasound may be prescribed.
There are several types of operations. A specific type is selected depending on the complexity of the pathology:
- ligature technique;
- excision of the fistula along its entire length with or without subsequent suturing;
- plastic surgery of the internal opening of the fistula;
- laser cauterization of the fistula tract;
- filling the fistula tract.
The surgical intervention is performed in a hospital; from 3 to 10 days after it it is necessary to remain under the supervision of doctors. The effectiveness of the operation reaches 90%.
Postoperative period
In the first days in the hospital, a gas tube is installed, antibiotics are prescribed, and dressings are performed. The pain syndrome is relieved with analgesics. It is important that there are no stools in the first 2-3 days, so a liquid diet is prescribed.
From the second or third day you can eat pureed, easily digestible food, you need to drink a lot. It is necessary to prevent constipation, which can cause the seams to come apart. Sitz baths with antiseptic solutions are prescribed, and, if necessary, laxatives and analgesic ointments.
After discharge, the patient should listen sensitively to his body and, if the following symptoms occur, immediately consult a doctor:
- excessive gas formation;
- fecal incontinence;
- a sharp increase in body temperature;
- constant abdominal pain;
- discharge of blood and/or pus from the anus;
- pain when urinating or defecating.
Basic recommendations for the rehabilitation period:
- eat small portions 6 times a day;
- drink at least 2 liters of water per day;
- do not consume foods that irritate the intestines - carbonated drinks, alcohol, chocolate, hot spices, fatty foods, foods with flavoring additives, etc.;
- give preference to vegetables and fruits as sources of fiber, eat cereals, grain bread and dairy products.
Indications
You should immediately contact a proctologist if you suspect a rectal fistula. The patient develops the following symptoms that indicate the development of an infectious and inflammatory process:
- purulent and mucous discharge from the anus;
- the appearance of anal bleeding;
- unpleasant odor in the anus;
- the appearance of wounds that do not heal over a long period;
- digestive tract disorders;
- problems with bowel movements;
- constipation and diarrhea;
- problems with urination;
- pain syndrome, which increases with coughing, sneezing, and physical activity;
- sensation of a foreign body in the anus;
- increased temperature and blood pressure;
- general weakness;
Rectal fistula is a dangerous pathology that, if left untreated, leads to complications and becomes malignant.
The main risks associated with paraproctitis
Deep fistulas of the extra- and transsphincteric types often recur.
Long-term progressive fistulas, which are complicated by the process of scarring of the walls of the rectum and purulent leaks, can lead to secondary functional changes.
Periods of new exacerbations are dangerous due to the appearance of fresh foci of inflammation and the involvement of an increasingly larger array of the anal sphincter in the inflammatory process. All of the above inevitably affects the general condition of the patient. Often there are complaints of weakened immunity, headaches, sleep problems, decreased performance, and irritability.
In addition to the above complications, a long-existing fistula can lead to pectenosis, namely a cicatricial change in the wall of the anal canal with decreased elasticity and cicatricial stricture. With a long-term illness, in some cases, malignancy of the fistula tract is possible.
Description
Rectal fistula is a disease in which a fistula (canal) is formed with an internal opening in the rectal cavity and an external opening on the skin 1-3 cm from the edge of the anus. Rectal fistula is a consequence of untimely or irrational treatment of acute paraproctitis - inflammation of the fatty tissue located around the rectum. As a result of paraproctitis, purulent melting of the soft tissues occurs and the abscess opens outward. The cavity remaining in the soft tissues is constantly contaminated with infectious agents from the rectum, which is why a fistula tract is formed from inflammatory and scar tissue. The diameter of its outlet holes rarely exceeds 1 mm. If a non-radical operation is performed to open and drain an abscess in acute paraproctitis, a fistula tract can also form if the entrance gate of infection from the rectum has not been eliminated.
Fistula paraproctitis - classification
Fistula paraproctitis has its own characteristics; for this purpose, experts have created a classification:
- Intrasphincteric fistulas. The simplest type of illness. In this case, their course is somewhat slowed down, and the inflammation is mild.
- Transsphincteric fistulas. Quite a common species, found quite often. It is characterized by the fact that the passages are localized in the subcutaneous layers and have branching.
- Extrasphincteric fistulas. The most dangerous form of paraproctitis, which occurs in 20% of cases of rectal pathologies. The fistula is localized on the internal sphincter.
The greatest danger to human health are pathologies that have a wide internal exit, surrounded by purulent scars.