Characteristics of the disease
The abdominal cavity is divided into:
- parental,
- vasceral.
The surface of the abdominal cavity in humans is up to 2 m². In the male body, the structure of the peritoneum is closed. In a woman's body, the abdominal cavity has contact with the external environment through the openings of the fallopian tubes.
The epithelial tissue, called mesothelium, secretes fluid that helps ease the internal organs and allows them to slide freely in the abdominal space.
In addition, this liquid contains immune molecules, cells and antibodies that help maintain a healthy state of the entire body.
Functions performed by the abdominal cavity
The abdominal cavity performs the following functions:
- Exudative (releases fluid and fibrin)
- Barrier (protects the peritoneal organs from external influences and irritants, resists the entry of infectious bacteria, while producing special protective substances).
The main property of the abdominal cavity is absorption; liquid can actively penetrate through it.
The essence of pathology
Irritation of the abdominal cavity occurs, as a rule, due to edema, which disrupts metabolic processes in this organ. To understand the question of what is irritation, you should know that nerve cells and endings are located in the peritoneum.
The parietal region is affected by the nerve endings of the intercostal space, so it is very sensitive to any type of influence: mechanical, physical or chemical. The pain arising in such an area is clearly localized.
The visceral region is affected by the autonomic relationship of the organ with the central nervous system. Pain in the visceral area is not localized, making it difficult to determine the location of inflammation.
In the pelvic region the patient also feels pain of unknown location. The pelvic peritoneum is plastic and has high muscle tension, so it does not have an acute reaction to inflammation.
Abdominal pain can be classified into:
- visceral (acute pain around the navel)
- somatic (severe pain, the point of which is clearly localized by the patient)
- reflected (occurs due to inflammation in nearby organs or brain pathologies.
Characteristic signs
Symptoms of abdominal irritation in the medical literature are identified by the authors who worked on their establishment and description. The most famous include:
- Razdolsky's symptom (established using the “percussion” diagnostic method, which means examining the desired part of the body through pressing or tapping)
- Rosberg phenomenon (determined by pushing pressure on the pre-inhalational region on the left, with increased pain in the area of the cecum). Used in the diagnosis of appendicitis.
- Shchetkin-Blumberg symptom (diagnosed by applying intense pressure in the area of development of the inflammatory process and abruptly removing the hand by the doctor). Appendicitis is easily detected by this method, since it is expressed by acute pain.
The main symptom of peritoneal irritation is pain in the patient's abdomen. As a rule, many symptoms of a given disease appear at the same time. The disease begins with the occurrence of pain in the inflamed organ or its location.
It is not recommended to try to relieve pain with painkillers on your own, as this may mask the real symptoms of a serious illness. Inflammation can cause peritonitis.
At this moment, it is imperative to place the patient in a supine position in order to relieve tension from the abdominal cavity and urgently call an ambulance.
A comfortable and less painful position will be lying on your back or side with your legs bent at the knees pulled up to your stomach. As the disease develops, even the slightest movement can cause severe pain.
In case of acute tension of the peritoneal walls, in exceptional cases, contact exposure is used to determine symptoms.
If the muscles of the peritoneal walls are retracted in a scaphoid shape, the point of the inflammatory process is determined by palpation.
If the peritoneum is irritated, the patient may feel nausea and vomiting. They manifest themselves reflexively, the cause is intoxication of the body and impaired intestinal patency. When the appendix is inflamed, the patient feels symptoms inherent in the general inflammatory process in the body. These symptoms include:
- increased temperature in the body,
- severe tachycardia,
- increased breathing,
- flatulence and bloating in the abdomen.
What could be the consequences?
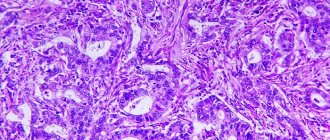
When an inflammatory process occurs in the organs of the abdominal cavity, swelling and thickening occur with clearly defined hyperemia of the serous membrane. A large amount of exudate changes the color of the shell, it becomes dull. Fibrin accumulates near the affected organ. During the disease, the presence of leukocyosis and an increase in ESR can be detected in the blood.
Blood biochemistry usually reveals an increase in C-reactive protein and fibrinogen.
If effective treatment is not started immediately, within 24 hours the entire human body becomes intoxicated, which provokes the release of blood plasma into the tissues.
Abnormal protein levels in the blood can impair blood flow. Blood can enter the intestinal and gastric cavities, causing vomiting containing blood.
Also, the patient will be unable to perform an act of defecation due to intestinal obstruction; it will fill with gases and swell, resulting in increased pain.
During the process of inflammation, a decrease in blood pressure occurs.
The patient changes in appearance, in particular, pallor of the skin appears, the pulse increases, the eye sockets deepen, the cheekbones recede and the facial features sharpen due to dehydration.
Changes also occur in the oral cavity; a yellow coating appears on the surface of the tongue and cheeks. On the third day of the disease, a complete disruption of the organic system in the human body occurs. If the inflammatory process is not stopped at this stage, it can result in death.
Symptoms of peritoneal irritation can occur in a woman with a serious pathology - an ectopic or frozen pregnancy. The first sign of the development of this pathology is heavy bleeding from the vagina after a long delay in menstruation with cramping pain.
If you notice any of these symptoms at any time, you should immediately seek medical help. You should not make independent attempts to treat acute and aching pain in the abdominal area, since it may be a signal of the presence of a serious inflammatory pathology in the abdominal cavity.
The essence of pathology
Irritation of the abdominal cavity occurs, as a rule, due to edema, which disrupts metabolic processes in this organ. To understand the question of what is irritation, you should know that nerve cells and endings are located in the peritoneum.
The parietal region is affected by the nerve endings of the intercostal space, so it is very sensitive to any type of influence: mechanical, physical or chemical. The pain arising in such an area is clearly localized.
ISSN 2618–7159 IF RSCI = 0.757
SYMPTOM OF PERITONEAL IRRITATION AND ITS VARIANTS
1 Olenko E.S. Papshitskaya N.Yu. Kolopkova T.A. Ponomareva O.A. Kurako M.M.
A symptom of peritoneal irritation, called the Shchetkin-Blumberg symptom, consists of careful, but as deep as possible pressing on the painful area of the abdomen, and then sharply withdrawing the hand.
The elastic abdominal wall quickly returns back to its original position, which causes sharp tension in the inflamed peritoneum and severe local pain. This symptom is very painful and does not need to be checked in patients with existing local protective muscle tension.
A less painful alternative test is light indirect percussion over the painful area.
This symptom was described by the German surgeon M. Blumberg in 1907. However, Russian obstetrician D.S.
Shchetkin used this technique in his clinical practice back in the late 80s of the 19th century, an official report of which he made in 1908.
A gentle version of the Shchetkin-Blumberg symptom is the symptom of distant rebound pain, the essence of which is that the doctor presses on the abdominal wall and then releases it in the quadrant opposite to where the patient feels pain.
A symptom is considered positive if pain occurs where the patient initially felt it. On the contrary, a symptom is considered negative if pain appears in the area of palpation.
A negative test result, however, does not exclude the diagnosis of peritonitis.
When determining the Shchetkin-Blumberg symptom, sometimes the patient exaggerates the intensity and severity of the pain syndrome. In these cases, in order to mislead the patient and distract his attention, the stethoscope symptom is used, which is rarely used today. The technique for performing it consists of repeated palpation of the abdomen: first with your hands, then with a stethoscope.
Determination of the symptom of peritoneal irritation (Shchetkin-Blumberg symptom)
It is carried out as follows: the doctor places the palpating hand flat on the stomach at the site of greatest pain.
Then, smoothly bending his fingers, he slowly plunges them deep into the abdominal cavity, after which he very quickly removes his hand from the stomach.
If the patient feels a sharp increase in pain at the moment the hand is removed from the abdomen, then a positive symptom of peritoneal irritation is stated (observed, as a rule, against the background of increased resistance of the abdominal wall).
Determination of the divergence of the rectus abdominis muscles
The doctor places the palpating right hand (with straightened and closed fingers) with its ulnar edge in the area above the navel on the midline of the abdomen of the person being examined. Then, lightly press the hand deep into the abdomen.
At the same time, the patient is asked to raise his head, bringing his chin to the sternum (at the same time, the rectus abdominis muscles tense) (Fig. 4.45). If, at the moment the patient lifts his head, the hand is pushed out of the abdomen, the absence of divergence of the rectus abdominis muscles is stated.
If the hand is not pushed out or a wide gap is felt between the tense ridges of the rectus abdominis muscles, then in this case the patient has a divergence of the rectus abdominis muscles.
Definition of hernial protrusions
It is performed with the patient standing. The doctor sits in front of the patient, facing him. The patient is given the command to strain and at the moment of straining, palpation is carried out with the tips of the fingers of the groin areas, the navel area, the area of postoperative scars, i.e. places where hernial protrusions may be located.
Superficial palpation of the abdomen in acute gastritis, duodenitis, or in exacerbation of chronic inflammatory or erosive-ulcerative processes in the gastroduodenal zone, as well as in inflammatory diseases of the biliary system, small and large intestines, often reveals local soreness and muscle tension over the projection of the affected organ. Especially often, pain and protective muscle tension are detected when the pathological process is localized on the anterior wall of the affected organ. Much less frequently, an area of extensive palpable pain is identified.
The traditional method of studying pain in the anterior abdominal wall by palpation makes it possible to determine the presence or absence of palpable pain syndrome. Determination of the degree of its intensity is possible only relatively. The question of quantitative assessment of the intensity of pain has always interested researchers.
Thus, Boas once proposed a kind of algesimeter, which allows one to study pain in the abdominal area using a graduated degree of pressure on certain local points of the abdominal wall. Currently, such research methods are rarely used, but they exist. So S.P. Golovkin and M.V.
Bitunov (2003) used a mechanical tensoalgesimeter of an original design to instrumentally assess the intensity of pain in patients with duodenal ulcer.
As a result of using this device, it is possible to determine the degree of pain experienced by patients in a wide range, depending on the sensitivity threshold (from 2 kg/cm2 to 15 kg/cm2).
Resistance of the muscles of the anterior abdominal wall during pathological processes localized in the duodenum, more often with peptic ulcer disease, is localized in the upper third of the right rectus abdominis muscle and is associated with the involvement of the parietal layer of the peritoneum in the process.
Severe muscle tension combined with severe pain is observed with periviscitis, penetration or perforation of an ulcerative defect of the duodenum. When penetrating an ulcer located on the anterior wall of the organ, the inflammatory infiltrate can sometimes be palpated.
In acute cholecystitis, palpation does not always reveal an enlarged gallbladder, but reveals positive palpation symptoms of peritoneal irritation.
It is important to detect zones of hyperesthesia (Zakharyin-Ged zone), most characteristic of peptic ulcer disease. Their location is usually determined on the anterior, posterior and lateral surface of the chest (see Fig. 5.12).
However, it should be said that these zones can show increased sensitivity not only with ulcerative lesions of the stomach or duodenum, but also with inflammation of the gallbladder or pancreas, which reduces the diagnostic value of this phenomenon for any specific localization of the process.
Causes and mechanism of development of abdominal disease
Signs of peritonitis are always the result of damage to the serous membrane lining the abdominal cavity, nonspecific and specific intestinal microflora. The following microorganisms can provoke the development of this pathological condition:
- coli,
- enterobacter,
- proteas,
- streptococci,
- staphylococci,
- fusobacteria,
- clostridia,
- eubacteria,
- gonococci,
- pneumococci,
- Mycobacterium tuberculosis, etc.
Depending on the etiology, inflammation of the peritoneum can be primary or secondary. In the primary form, pathogenic microflora is introduced into the area of the serous membrane of the peritoneum by hematogenous or lymphogenous route. Most often, the primary form develops with renal tuberculosis, enterocolitis and salpingitis.
In clinical practice, secondary peritonitis is the most common. It develops against the background of other pathologies of the gastrointestinal tract. The diseases against which the development of this pathological condition is most often observed include:
- appendicitis,
- intestinal obstruction,
- Crohn's disease,
- perforated stomach ulcer,
- diverticulitis,
- strangulated hernia,
- pancreatic necrosis,
- pancreatitis,
- cholecystitis,
- complicated cysts,
- pyosalpinx.
There is an increased risk of developing peritonitis due to blunt and acute abdominal injuries. The appearance of this pathology can occur as a complication in the postoperative period. Inflammation of the serous membrane can occur against the background of autoimmune processes, granulomatosis, parasitic infections, etc.
What is peritoneal irritation syndrome?
The human body is complex. There are many organs in the abdomen, each of which performs its own function. The breakdown of one threatens all the others: microbes, bleeding, tumors affect neighboring organs.
Knowing the symptoms of peritoneal irritation helps to understand what is happening inside the abdominal cavity, before using all instrumental methods.
The ability to identify them helps to recognize dangerous moments in life when a person urgently needs medical help.
Structure and function of the peritoneum
The peritoneum is a thin film that has 2 layers: one from the inside covers the walls of the abdominal cavity, the other covers all the internal organs in the abdomen. From above it covers the abdominal side of the diaphragm, below it passes to the pelvic organs and the walls of the pelvic cavity.
Treatment of peritonitis
The basis of treatment for peritonitis is surgical removal of the source of infection. But since the patients’ condition is usually severe, intensive infusion and antibiotic therapy is prescribed before surgery, aimed at stabilizing the function of internal organs. Abundant intravenous infusions of colloid and crystalloid solutions should restore circulating blood volume and electrolyte balance, antibiotics should somewhat reduce the activity of inflammation.
During the operation, the source of inflammation is eliminated: the appendix, gall bladder are removed, perforated ulcers, intestinal wounds are sutured, etc. The pathological contents are evacuated with an electric suction. The abdominal cavity is washed generously to remove toxins and microorganisms. Drainage tubes are inserted through special holes in the abdominal wall to ensure the drainage of inflammatory fluid. After surgery, intensive conservative therapy is continued, aimed at eliminating the infection and maintaining vital body functions.
At the end of the acute phase of peritonitis, restorative therapy of the gastrointestinal tract with the help of gastroenteroprotectors (rebagit, rebamipide) is recommended.