Diseases of the small intestine occur in all segments of the population. The mechanisms of disease are varied, there are acute and chronic lesions, infectious and autoimmune. Hence the approaches to therapy. Treatment of the small intestine is a labor-intensive process aimed at correcting numerous pathogenic factors.
To enlarge the picture, click on it.
The small intestine consists of three parts: duodenum, ileum and jejunum. Their main function is to digest food and absorb nutrients and water. As soon as absorption dysfunction occurs, the entire body suffers. Protein deficiency, hypovitaminosis, stool disorders, gas formation occur, and periodic pain syndrome is possible. Due to the wide range of symptoms, the arsenal of drugs used in the treatment of diseases of the small intestine is quite large.
Symptoms of intestinal diseases
The most common is indigestion. It manifests itself as follows:
- stool disorder. The frequency of defecation reaches 5-6 times a day, the volume of stool is increased, and remnants of undigested food can be seen in it. With serious damage to the intestines, blood and mucus are present in the stool;
- the occurrence of rumbling intestines, bloating;
- pain. Painful sensations are located in the umbilical region, or slightly to the right. The pain is not acute, it is constant, dull, and decreases after the passage of gas. If intestinal motility is increased, the pain becomes stabbing in nature.
In addition to intestinal symptoms, there are also general signs of the disease. As a result of chronic malabsorption of substances, their artificial deficiency occurs. Food enters the body, but is not absorbed. This causes the patient to lose weight against the background of normal nutrition, the occurrence of hypovitaminosis, and anemia. Deficiency of fat-soluble vitamins K, A, E, D leads to poor vision, increased bone fragility, disruption of the menstrual cycle in women and sperm count in men. Dry skin occurs, microcracks appear on it, and jams appear in the corners of the lips. With a deficiency of microelements, iron and calcium are not supplied. The hematopoietic system suffers and osteoporosis occurs.
If the intestinal disease is acute, the patient experiences only intestinal disorders. Due to the short duration of symptoms, deficiency of vitamins, nutrients and macroelements does not have time to occur.
There are many chronic diseases of the small intestine.
Human jejunum
The unusual name of this organ of the digestive system comes from the fact that when a pathologist examines a corpse, the internal contents of this section of the small intestine are always empty. The anatomical location of the jejunum is the middle section of the small intestine, located after the duodenum and before the ileum. The jejunum and ileum do not have a clear line of demarcation between each other, however, they have a well-defined mesentery - an anatomical organ of the digestive system, thanks to which the hollow organs of the abdominal cavity are attached to the posterior wall of the abdomen.
The human jejunum is a smooth muscle hollow structure, the walls of which have two muscle layers: longitudinal and circular. The length of the anatomical organ in an adult is about 2 m, and in women the jejunum is slightly shorter than in men. After a person's death, the muscle tissue weakens, and the length of the jejunum reaches 2.5 meters.
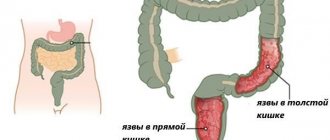
Foci of inflammation of the jejunum
What is the jejunum needed for and what is its significance in the anatomical structure? There is still no consensus on this question. Medical experts suggest that this organ of the digestive system functions as a filtrate in systemic digestion, however, this has not been scientifically proven.
Chronic enteritis
It is a sluggish long-term inflammation of the intestines. It may occur as a result of exposure to intestinal pathogens after the acute phase of the disease has subsided. Untreated acute enteritis can become chronic. In addition to microorganisms, worms and parasites can cause inflammation.
There are frequent cases where intestinal lesions are provoked by ionizing inflammation, heavy metal salts and certain medications.
The mechanism of the disease includes four types of pathological processes:
- infection of the intestines with bacteria;
- violation of the protective mechanisms of the small intestine;
- decreased production of intestinal enzymes;
- disruption of proper intestinal motility.
Vascular lesions of the small intestine
With atherosclerosis, all the vessels of the patient are affected by plaques. Their lumen noticeably narrows, which means much less blood flows. The intestines are in a state of constant oxygen starvation. The disease manifests itself as abdominal pain. They start in the central region and then spread to the entire abdomen. Occurs after eating for 30 minutes to one and a half hours. During this period, the intestines work at their maximum, and the need for oxygen increases. The pain in this condition is severe. Patients are afraid of their recurrence and refuse to eat. In addition to pain, intestinal disorders occur. This disease is very dangerous, since as atherosclerosis of the arteries progresses, their complete blockage can occur with further death of part of the intestine.
Allergic lesions of the small intestine
An excessive reaction of the body to foreign substances is called an allergy. On the skin, manifestations appear as itchy blisters, redness, or a small red rash.
The small intestine is also affected by allergies, especially food allergies. This is manifested by the occurrence of enteropathy. In simple words, the intestine “goes bald” due to the death of the suction villi. Nutrients are not absorbed properly and stool upset occurs. The most common causes of allergies are food products, medications, vaccine serums and pollen.
Celiac disease
Otherwise the disease is called celiac enteropathy. It is caused by a hereditary deficiency of the enzyme that breaks down one of the protein components of cereals - gluten. In the absence of an appropriate diet, intestinal damage is persistent and severe.
Due to incomplete breakdown of proteins, toxic products are formed that harm the small intestine. The mucous membrane becomes thinner due to the destruction of the upper layers. The intestines become unable to fully cope with their function. The disease manifests itself as recurrent diarrhea. Patients are often underweight. In addition to intestinal disorders, general somatic symptoms are pronounced. There is anemia, which is difficult to treat, bruising of the skin, excessive bleeding, mental disorders and bone pain. Under the guise of all these manifestations, gluten enteropathy may be hidden. Due to the abundance of symptoms, the disease is diagnosed late.
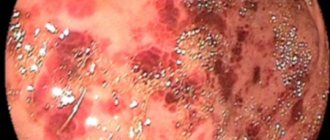
Diagnosis of inflammation of the jejunum
Isolated lesions of the jejunum are extremely rare, which complicates the diagnosis of the disease. However, the disease can be verified using histological and bacteriological laboratory tests. However, before starting diagnostic procedures, the gastroenterologist conducts an objective examination based on the patient’s medical history and complaints.
Mebeverine® – antispasmodic agent for jejunitis
Deep palpation to the left and above the navel can reveal pain, medically defined as Pogres and Störberg syndrome, when a sensation of pain occurs when the abdomen is deeply palpated in the area of the mesentery of the jejunum. The final confirmation of the diagnosis is a biopsy of the mucous membrane of the jejunum, which, after examining the biomaterial, will determine the degree of damage to the villous lining and determine the nature of the swelling of the tissue surface.
Neoplasms of the small intestine
Benign formations predominate. They grow slowly, without disturbing the anatomy of the intestine, and have little effect on intestinal patency and human well-being.
Malignant neoplasms of the intestine grow rapidly and contribute to intoxication of the body. Cause intestinal and general manifestations. They can grow into neighboring organs. If cancer grows into the wall of the intestine, its lumen may narrow. Intestinal obstruction occurs with severe symptoms of poisoning of the body. The condition requires immediate medical attention.
Prognosis for life and prevention of jeunitis
The form of the pathological condition plays a very important role in determining the prognosis. In most cases, acute or chronic jejunitis responds well to therapeutic treatment, provided that you consult a doctor in a timely manner.
Prevention of inflammation of the jejunum will be compliance with sanitary and hygienic standards of the hostel, rational nutrition and timely diagnosis of the disease.
If you notice unpleasant symptoms in the gastrointestinal tract, you should immediately seek medical help from a gastroenterologist. Take care of yourself and always be healthy!
Treatment of diseases of the small intestine
In case of allergic damage to the intestines, you should adhere to a hypoallergenic diet. The attack is relieved with the help of antihistamines, such as suprastin, tavegil, fenkarol, loratadine, cetrin. If the allergy is accompanied by angioedema or anaphylactic shock, you need to urgently administer adrenaline or glucocorticosteroids.
For celiac disease and other enzyme deficiencies, you need to stick to a diet and avoid foods that are not digested in the body. Following correct nutritional recommendations makes the life and health of patients complete. The intestines are not exposed to pathological effects and remain healthy.
Whipple's disease is treated with long-term antibiotics. Therapy continues for years. The choice of antibiotics should be selected by the attending physician, taking into account sensitivity to them.
Disease of the vessels supplying the small intestine is treated with vasodilator drugs. The choice is given to long-acting nitrates. To stop the formation of cholesterol plaques in the lumen of blood vessels, you need to take statins. These medications not only lower cholesterol levels, but also stabilize existing plaques.
Most often people suffer from chronic enteritis. Its treatment requires regularity and combination with proper nutrition. Chronic intestinal diseases take a long time to be treated, patients need to be prepared for this.
Drug treatment of chronic enteritis
Suppressing the progression of dysbiosis and normalizing intestinal microflora is one of the most important aspects of therapy. The question of how to treat such microflora disorders is not urgent. Bacterial drugs are prescribed. They contain beneficial microorganisms. Normally, they live in large numbers in the intestinal lumen. The following drugs are used: enterozermina, bactisubtil, lactobacterin, bificol, bifidubacterin. It is worth taking probiotics in courses. The first lasts three weeks. The drugs should be taken before meals twice a day, 3-4 standard doses. Then you need to stop taking the drug for a week and repeat the shortened course. The treatment regimen should be taken once a quarter to avoid exacerbation of dysbiosis.
The use of enzyme preparations helps to eliminate excessive gas formation, rumbling and frequent bowel movements. Pancreatic enzymes normalize absorption and digestion in the small intestine. The most common are pancreatin, mezim forte, creon, festal, panzinorm, pancitrate. In case of severe enzyme deficiency, medications are taken for a long time. Due to the lack of toxicity, they can be used for years. In people with mild forms of chronic enteritis, the drugs are used in a monthly course. The drugs are taken with or immediately after meals at each meal. The dosage depends on the severity of the disease.
If there is excessive intestinal motility, you need to use drugs that normalize stool. These include enveloping and astringent agents. You can use bismuth preparations in powders 1 g 4 times a day, tannalbin 0.5 g 4 times a day, kaopectate 1 tbsp. l. Up to 6 times a day.
Imodium fights diarrhea well. A contraindication to taking the drug is acute infection.
Diet
It is recommended to consume the following products:
- yesterday's bread, only dry biscuits;
- soups with cereals and vegetables. Cooking in low-fat broth is allowed;
- fish and lean meat, steamed or boiled;
- Vegetable dishes that do not increase gas formation in the intestines. You can eat potatoes, carrots, pumpkin, cauliflower, zucchini in the form of puree, casseroles, or baked. Ripe tomatoes can be eaten raw;
- cereals and pasta are not prohibited. It is undesirable to eat millet and pearl barley porridge;
- eggs;
- sweets;
- dairy products, including butter, cottage cheese and cheese;
- Recommended drinks include tea and weak coffee.
Causes
- Intestinal infections. Intestinal infections most often cause acute inflammation of the jejunum. The leading role belongs to rotaviruses, enteroviruses, salmonella, and campylobacteria. In some cases, after suffering an acute intestinal infection, jejunitis becomes chronic. Chronicity of the process can be facilitated by helminthic infestation (giardiasis, ascariasis, strongyloidiasis).
- Nutritional factor. Errors in nutrition in themselves are not the cause of jeunitis, but they predispose to the onset of the disease. The development of jeunitis is facilitated by the predominance of high-carbohydrate foods in the diet, abuse of spicy seasonings, and dry food.
- Alcohol abuse. The toxic effect of alcohol on the mucous membrane causes functional disorders, thereby leading to the development of chronic jeunitis.
- Food allergies. The most allergenic are cow's milk, nuts, fish, and chocolate.
- Exposure to certain drugs and toxins. Mercury, phosphorus, lead, arsenic, and zinc have a toxic effect on the small intestine. The development of chronic jejunitis is facilitated by long-term treatment with non-steroidal anti-inflammatory drugs, cytostatics, and glucocorticosteroids.
- Ionizing radiation. Radiation enteritis, in most cases, develops during radiation therapy for malignant diseases of the pelvic and abdominal organs.
- Insufficiency of the major duodenal papilla. Due to insufficiency of the duodenal papilla, bile constantly leaks into the intestine, which contributes to the development of jeunitis.
- Previous operations on the gastrointestinal tract. In the development of jejunitis, operations on the stomach (resection, vagotomy, gastrostomy) are of greatest importance.
- Ischemia of the wall of the small intestine. Chronic ischemia disrupts the ability of the mucous membrane to regenerate and contributes to the occurrence of dystrophic changes in the jejunum.
- Concomitant pathology. Secondary jeunitis can develop against the background of other gastrointestinal diseases (with gastroduodenal ulcers, hepatitis, cirrhosis of the liver, diseases of the biliary tract, pancreas), with severe renal failure with the development of uremia; for eczema; psoriasis; endocrine pathology (diabetes mellitus, thyrotoxicosis); systemic connective tissue diseases; cardiovascular diseases; immunodeficiencies.