Acute catarrhal gastritis is a form of inflammation of the stomach that begins abruptly and proceeds with acute symptoms. The process can cover both the mucous membrane of the organ as a whole and its individual parts. Pathology is provoked by single factors of intense exposure (poisoning, infection, strong influence of temperature).
Causes of catarrhal gastritis
Inflammation in the gastric mucosa occurs due to many different factors:
- chemical;
- bacteriological;
- mechanical;
- medicinal.
The most common causes of catarrhal gastritis include:
- Dietary disorder;
- Infectious diseases;
- Exposure to medications;
- Allergic reactions to a number of foods.
Stress gastritis is often encountered in medical practice. The disease appears under the influence of causes: respiratory failure (carrying out artificial ventilation), diseases of the digestive and urinary system, surgical interventions, trauma and burns of the mucous membrane, septic complications, disorders of the central nervous system.
The reasons are divided into external and internal. Exogenous factors - for example, toxic substances coming from outside the body and causing erosive changes in the wall of the stomach. Endogenous factors are causes that arise within the body, as a result of a previously occurring disease that led to gastritis.
During infectious diseases, a large amount of toxins are formed in the body - derivatives of the breakdown of infected proteins. It is they, together with the inflammatory process, that affect the integrity of the mucous membrane.
Diagnostic measures
Diagnosis of catarrhal gastritis is carried out by a gastroenterologist. He can determine the presence of a disease by its distinctive symptoms, as well as determine the causes of its occurrence. The patient must tell what food he ate and whether he had any nervous shocks before the attack.
After first aid, blood, stool, urine tests and endoscopy can confirm the diagnosis. Typically, catarrhal lesions are accompanied by thickening and swelling of the gastric mucosa and the presence of a large amount of mucus on it. To prevent the disease from becoming chronic, it must be treated.
Types of catarrhal gastritis by localization
Signs of catarrhal gastritis are observed 4-10 hours after exposure to irritants. The nature of the disease determines rapid or gradual development. The degree and duration of exposure to irritants, as well as the sensitivity of the body, influence the course of the disease. Catarrhal gastritis is characterized by typical symptoms:
- soreness, heaviness, fullness in the pit of the stomach
- bowel dysfunction;
- gray-white coating on the tongue;
- pain in the epigastrium on palpation;
- increased heart rate, decreased blood pressure.
Patients prefer certain types of food - salty, sour, cold.
Total or diffuse catarrhal gastritis
The disease is one of the main causes of the development of stomach cancer. Inflammation spreads along the length of the mucous membrane, and the transition from acute to chronic is not difficult.
The disease manifests itself as ordinary gastritis - weakness, nausea, vomiting, unpleasant taste in the mouth. Subsequently, pain in the epigastric region occurs. Tissue damage impairs organ function. The larger the surface of the lesion, the more difficult it is for the organ to digest food. As a result, the patient's weight decreases. Poor digestion of food leads to its rotting inside the stomach. Stomach bloating, belching of rotten eggs and flatulence occur. In addition, symptoms of intoxication are added.
Focal catarrhal gastritis
Patients are most often diagnosed with focal catarrhal gastritis. This diagnosis means that the inflammation is located in a limited area and is characterized by focal atrophy of the gastric mucosa. Changes in stomach tissue, developing superficial catarrhal gastritis are aggravated and develop into ulcers from the lesions. Before ulcers occur, erosions first form on the surface of the stomach walls. Therefore, doctors diagnose “catarrhal-erosive gastritis.”
Antral gastritis
Catarrhal gastritis of the antrum of the stomach is formed due to massive infection with Helicobacter pylori bacteria. Due to low acidity, bacteria multiply quickly and penetrate the mucous membrane. The activity of Helicobacter pylori causes irritation and the formation of an inflammatory process.
Everyone has bacteria in a single quantity in the body, but it is risk factors - stress, food poisoning, chemicals, bad habits, and dietary disorders that provoke their proliferation.
Catarrhal gastritis of the antrum is manifested by the following feature: abdominal pain occurs after food intake and lasts about 2 hours. This is due to the time of food processing and the effect of hydrochloric acid on the affected organ wall. Antrum gastritis is constantly accompanied by a feeling of heartburn. Black blood streaks appear in the stool. Sour belching, constant feeling of nausea, vomiting interspersed with blood. In the absence of timely treatment, the patient's condition worsens.
Treatment of focal antral gastritis
When answering the question, focal antral gastritis, what is it, you need to understand that this is a dangerous disease that requires timely initiation of treatment. Therapy helps destroy infectious agents, restore the mucous membranes of the lower stomach, and prevent the re-development of the inflammatory process.
Proper nutrition, combined with taking medications, helps normalize stomach acidity during gastritis. Additionally, agents are used that restore the number of beneficial intestinal bacteria. Surgical interventions for focal superficial gastritis are not used.
What do doctors usually prescribe?
The drug treatment regimen for the disease includes:
- Antibiotics. To eliminate Helicobacter pylori, Metronidazole is used, which is supplemented with Amoxicillin, which increases the sensitivity of bacteria. The drugs are taken in doses prescribed by the doctor for 14 days.
- Antispasmodics (Buscopan, Trimedat). These drugs help relieve an attack of severe pain caused by spasm of the gastric walls.
- Proton pump inhibitors (Omez, Ranitidine). The drugs normalize the production of hydrochloric acid, preventing further damage to the walls of the stomach.
- Enzymes (Pancreatin, Panzinorm). Prescribed when the inflammatory process spreads to the pancreas. The drugs compensate for the deficiency of pancreatic enzymes, normalizing digestion.
- Antacids (De-Nol). Used to urgently reduce the acidity of gastric contents and eliminate heartburn.
- Probiotics (Bifiform). Restore intestinal microflora after taking antibiotics.
- Vitamin products (Ferrum Lek, vitamin B12). Used to restore the body after stomach bleeding.
Folk remedies
To treat mild forms of antral gastritis, the following folk remedies are used:
- Plantain decoction. 100 g of fresh leaves are poured into 0.5 liters of grape vodka and boiled in an enamel pan for 5 minutes. The finished product is filtered and stored in a glass container. The decoction is taken 1 tbsp. l. half an hour before eating.
- Burdock root infusion. 1 tsp. raw materials are poured into 0.5 liters of boiling water and left in a thermos for 12 hours. The finished infusion is filtered and taken 100 ml in the morning and evening.
- Potato juice. The product has an enveloping and protective effect. The potatoes are grated and the juice is squeezed out of the resulting mass. It must be drunk within 5 minutes after preparation. Food can be consumed after half an hour. The course of treatment lasts 10 days.
Forms of gastritis by causes
The origin of gastritis is divided into 2 groups: microbial and non-microbial. When microbial damage to the stomach is caused by gastritis, Helicobacter pylori predominates. Non-microbial gastritis has nothing to do with bacteria. Other reasons predominate in this group:
- Alcohol damage. Alcohol abuse changes the acidity of the stomach, increasing the susceptibility of the walls to acid, as the mucous membrane becomes thinner.
- Non-steroidal anti-inflammatory drugs. The anti-inflammatory effect of NSAIDs affects the gastric wall - enzymes cease to be released from it.
- After surgical interventions. Resection of part of the stomach can affect the condition of the gastric mucosa.
- Exposure to aggressive chemicals. Chemicals destroy the stomach lining.
- Group of unknown causes. Cases where the occurrence of gastritis cannot be attributed to any of the previously described ones.
Atrophic gastritis
Catarrhal-atrophic gastritis is a slowly developing disease. A prolonged course disrupts the functioning of the stomach lining and its restoration. This gastritis predominates in men aged 30-50 years. One of the dangerous types of gastritis, tissues undergo changes taking on the appearance of precancer. A long course leads to the depletion of defense and recovery mechanisms, so this form of the disease does not have a clear clinical picture.
Acute catarrhal gastritis
Acute gastritis is formed under the influence of factors that act simultaneously.
The following types of acute catarrhal gastritis are distinguished:
- Simple.
- Phlegmonous.
- Necrotic.
- Fibrinous.
Most often, the disease occurs in the form of phlegmonous gastritis. The infection enters directly into the stomach wall. Sometimes phlegmonous gastritis is a complication of other diseases.
The disease is characterized by heartburn, high fever, shortness of breath and other criteria. The patient's condition is serious. Due to pain, patients refuse to eat and drink.
Chronic catarrhal gastritis
Chronic gastritis could previously have an acute form. But if measures to treat this disease are not followed, it leads to chronic inflammation of the stomach wall. In another variant, the disease proceeds for a long time and unnoticed, so the patient has no complaints about the symptoms for a long time, considering them a reaction to food that is not fresh or poorly prepared. Over time, the symptoms of the disease worsen and the stomach becomes sensitive. The patient is accompanied by constant heartburn and flatulence. Chronic gastritis is the cause of precancerous and cancerous conditions of the organ.
Chronic catarrhal gastritis is different for each patient. In some people it is accompanied by increased acidity, in some cases the acidity remains normal. The secretion of hydrochloric acid may also change - increase or decrease until it becomes insufficient.
Catarrhal reflux gastritis
This disease depends on the incompetence of the pylorus of the stomach. The sphincter does not perform its contractile function. Therefore, gastric juice, which contains hydrochloric acid, is thrown from the stomach into the esophagus when the walls contract. Stomach acid destroys the protective layer of the esophagus, deeply affecting the tissue. Catarrhal reflux gastritis is called the first cause in the occurrence of dysplastic changes in esophageal tissues leading to the development of precancer, and subsequently esophageal cancer.
Symptoms of the disorder
Antral, diffuse, focal catarrhal gastritis always appears acutely and suddenly:
- Strong pain. Occurs 4-6 hours after poisoning or the action of another factor.
- Heartburn. The burning sensation occurs due to the penetration of gastric juice into the esophagus, and the acidity level increases.
- Vomiting and nausea. Develops due to dysfunction of the stomach.
- Belching. Appears due to the penetration of stomach contents into the mouth.
- Tachycardia, arrhythmia. Due to irritation of nerve fibers, the heart rhythm changes, and organ functions may be impaired.
- Intoxication. Digestion slows down and toxins and other harmful substances cannot leave the body normally.
- Fever. Observed with increasing intoxication and in the case of viruses.
- Malaise and general weakness. The symptoms are typical for any form of gastritis, be it pathology with duodenitis or bulbitis.
- Stool disorders. Most often, patients experience diarrhea, but this may not occur. Constipation with catarrhal form of the disease is rare.
It is impossible to determine the form of catarrhal gastritis by symptoms alone; the patient requires serious diagnostics.
Diagnosis of gastritis
A set of diagnostic measures is used to identify gastritis in a patient. Diagnostics consists of:
- Questioning and inspection. Complaints and results of palpation, percussion, and auscultation characterize the most common signs of the disease.
- Comparison of lifestyle and identification of the main risk factors that can lead to the development of the disease.
- Analyzes and instrumental diagnostics.
Analyzes
To clarify the diagnosis, doctors prescribe laboratory diagnostics - blood, urine, and stool tests. It is also mandatory to identify Helicobacter pylori in the patient.
Bacteria Helicobacter pylori
Instrumental diagnostics
If catarrhal gastritis is suspected, the patient is advised to undergo the following instrumental studies:
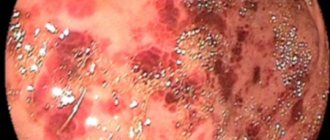
- FGDS - fibrogastroduodenoscopy, using this method, the doctor can visually examine the surface of the gastrointestinal tract. This research method allows us to examine changes in the condition of the wall, ulcers and erosion.
- Radiography with contrast is a preparation with special elements that color the surface of the gastrointestinal tract and reveals on the x-ray image all violations of the integrity and changes in the condition of the organ.
- Ultrasound is an ultrasound examination of an organ. An accurate method based on the reflection of an ultrasonic wave from an organ; in the place where there is damage, the ultrasound is reflected differently.
- Biopsy. Simultaneously with FGDS, a biopsy of stomach tissue is most often taken from 5 different places.
- Unfortunately, the final result in which one can accurately say about the form of gastritis and changes in the tissues of the stomach of a malignant nature is only when examining a macroscopic specimen and collecting material (micropreparations) from it during a pathological examination.
Symptoms and diagnosis of the disease
Acute catarrhal gastritis is characterized by the appearance of symptoms within a few hours after the onset of inflammation. The patient feels:
- stabbing and cutting pain in the navel and upper abdomen;
- heaviness;
- burping;
- nausea;
- heartburn;
- unpleasant taste in the mouth.
GALINA SAVINA: “How easy it is to cure gastritis at home in 1 month. A proven method is to write down the recipe. » Read more >>
In some cases, when acute gastritis occurs, patients develop a fever and nausea is accompanied by vomiting. When vomiting, bile is released. Patients experience:
- weakness;
- dizziness;
- chills;
- increased fatigue;
- heavy sweating.
While examining the patient, the doctor observes a gray coating on the tongue and a sour smell from the mouth.
Acute gastritis, if left untreated, will develop and become chronic.
The symptoms of catarrhal gastritis in the chronic form are slightly different from those in the acute form. Patients have stool disorder (tendency to constipation), appetite decreases, and the person almost completely refuses to eat, since eating makes him feel painful. Chronic gastritis is characterized by periods of exacerbation and remission. Chronic gastritis cannot be cured forever.
Diagnosis of catarrhal gastritis does not require numerous tests and expensive examinations. It is often enough for an experienced doctor to conduct a thorough visual examination of the patient and find out what circumstances led to the attack of the disease.
To determine the extent of damage to the mucous membrane, gastroscopy is prescribed. This examination involves inserting a special probe into the stomach cavity and displaying a picture on the monitor. With its help, the doctor examines the inner surface of the stomach walls and, if necessary, can take samples for histological examination.
Only after examining the patient and gastroscopy, the doctor prescribes treatment appropriate to the severity of the disease.
If the disease is not treated in time, the symptoms worsen, and catarrhal gastritis becomes diffuse.
How to treat catarrhal gastritis
First of all, it is worth determining the cause of gastritis, this will provide the most effective treatment. You must adhere to your doctor's orders. Therapy depends on the type and severity of the patient's condition.
Thus, in case of acute gastritis, actions are taken to cleanse the stomach and intestines of food debris using rinsing. Afterwards, the patient is on a medicinal fast for a couple of days, but is sure to receive a sufficient amount of fluid.
During attacks, therapy is carried out with medications or folk remedies, if the form and severity of the disease allows.
Drug treatment
In case of reduced acidity, medications that stimulate the production of gastric juice are prescribed. The mechanism of action of drugs in this group is to reduce painful symptoms. Examples of drugs are: Cytochrome C, Limontar, Pentagastrin and others.
Normal and high acidity increases the need for the use of drugs that reduce the concentration of stomach acid and also eliminate heartburn. The drugs are offered in the form of tablets, powders, suspensions, and solutions.
Adsorbents are used in the first stages of the disease. These medications help collect excess stomach acid. By enveloping the walls of the stomach, distributed over the surface of the gastric contents, antacids prevent the acidic contents of the stomach from being thrown into the esophagus. Preparations: Enterosgel, Polyphepan.
Antacids are used in case of excessive sour belching, heartburn and increased pH of gastric juice. Drugs in this group neutralize acid, reducing the feeling of heartburn. Preparations: Rennie, Phosphalugel.
Medicines that restore the gastric mucosa. The mechanism of action of such drugs is as follows. The substance acts on proteins that settle on the walls of the stomach, forming a protective film. Drug: De-Nol.
Treatment with folk remedies
This therapy uses natural substances of plant origin that eliminate the inflammatory process in the stomach.
An infusion of plantain leaves, potato juice, sea buckthorn oil, an infusion of crushed celandine leaves with honey have a beneficial effect on the surface of the stomach.
Folk remedies should be taken every day for 20-30 days. But you should not abuse this, as some substances lead to exacerbations of the disease. Herbal treatment will alleviate the patient’s condition, but complete recovery will occur only after full-fledged medicinal procedures.
Treatment methods
If after diagnosis gastropathy is confirmed, then appropriate therapy is carried out. Treatment of catarrhal gastritis is prescribed by a gastroenterologist.
To stop attacks of the disease, medications are used. Medicines relieve spasms, relieve heartburn, nausea, vomiting, and other pathological symptoms.
In adults, treatment is accompanied by cessation of smoking and alcohol. In addition, a diet is indicated that includes foods that do not irritate the stomach. The focus is on prevention to prevent inflammation from developing.
In addition to traditional methods, most patients use folk remedies for gastritis. This type of therapy involves the use of natural medicinal ingredients.
Inflammation of the mucous membrane is effectively eliminated with potatoes, linseed oil, honey, plantain, and celandine.
Before using traditional methods, you should consult a doctor, because some remedies can cause an exacerbation of the disease.
Diet for catarrhal gastritis
For this disease, a special diet is recommended. The menu for catarrhal gastritis includes avoiding the following products:
- Fried, smoked, spicy, pickled, salted.
- Alcohol, sausage, legumes, cabbage, carbonated drinks.
- Excessively hot or cold food.
Eat food 5-6 times a day. Food must be chewed thoroughly. During an exacerbation, the diet is observed more strictly. The diet includes fruits, dairy products, vegetable purees, poultry and steamed fish. The menu for the week is selected individually.
What precedes the disease
The disease can go from a sluggish stage to an active phase with the manifestation of the most aggressive symptoms: nausea, acute pain, diarrhea or nausea. In most clinical cases this is preceded by either severe stress, and most often by poor nutrition. Thus, an emerging disease may not clearly manifest itself for a long time, consisting only of minor symptoms, which the patient, as a rule, attributes to other existing diseases or does not attach importance to them at all.
Acute pain forces patients to pay attention to the disease. The reason in these cases is the consumed “wrong product”: a large amount of alcohol or carbonated drinks, spicy, smoked-salty or sweet
These products act as irritants to the mucous membrane, which causes pain, nausea and other symptoms of the disease.
Less often, stress becomes a catalyst for illness. In this case, indigestion and stomach dysfunction occur, which provokes intoxication, and it is this process that causes nausea, heaviness or acute pain.
Prevention
Basic recommendations:
- Refusal of foods that irritate the stomach. Preference for dietary meat, steamed.
- Compliance with diet. Avoid overeating and completely avoid fasting.
- Prohibition of alcohol and tobacco products.
- Timely consultation with a doctor in case of gastrointestinal diseases.
- Sports and active recreation.
- Do not overuse medications, especially antibiotics.
Recommendations should be followed even if there are no signs of stomach disease. Get regular checkups with your doctor. Early detection of the disease will help avoid complications in the future.