In a healthy body, all physiological functions are in harmony. Gastric secretions are important for proper digestion and absorption of nutrients. Many factors affecting the function of the secretion-producing glands suppress its production. In this case, symptoms of indigestion develop. Other factors, on the contrary, stimulate secretion, resulting in the concentration of enzymes and pancreatic juice in the stomach cavity. This condition can also cause gastrointestinal diseases, since overstimulated production of hydrochloric acid provokes the formation of ulcers in the gastrointestinal system.
How is everything going?
Gastric secretion is stimulated by a chewed bolus of food coming from the esophagus and moistened with saliva. It mechanically and chemically irritates the walls of the stomach, which provokes the release of enzymes and hydrochloric acid by the glands for the further breakdown of complex substances into simpler ones. The vagus nerve also influences their production. Internal secretion promotes parietal digestion. Enzymes and hydrochloric acid, released initially, promote the digestion of food in the lumen of the gastrointestinal tract.
Secrets functions
Enzymes contained in the glands help break down complex food molecules into simple ones.
Substances contained in the glands are capable of stimulating the breakdown of complex food molecules into simple ones. If we take each component of gastric juice separately, they perform the following functions:
- Pepsin. This enzyme is the main one, since it breaks down heavy proteins first into lighter ones (albumose and peptones), and eventually into small amino acids.
- Hydrochloric acid. It activates pepsin, converting it from its inactive form - pepsinogen. Bicarbonate also provides a more acidic or alkaline environment in the gastrointestinal tract. Hydrochloric acid destroys pathogenic microorganisms that enter the stomach with food.
- Renin. Helps digest breast milk in young children.
- Lipase. Works with fats, breaking them down into fatty acids and glycerol.
- Slime. Contains bicarbonates, which alkalize the gastric environment in case of excessive acidification. Mucus neutralizes hydrochloric acid when it is hypersecreted. It covers the gastric folds with a thin layer.
- Hormones and biologically active substances (gastrin, motelin, somatostatin, histamine, serotonin) provide regulation of the entire gastrointestinal system.
An anti-anemic factor is produced in the stomach. It stimulates the release of vitamin B12 from food, which is necessary for hematopoiesis.
Diet therapy
Diet is the first thing that is mandatory for a patient to treat gastritis with decreased secretory function of the stomach. It is aimed at activating the work of parietal cells of the gastric mucosa, which produce hydrochloric acid. An important point in treatment is not only following a diet, but also following certain rules in the diet:
- When the acidity of the stomach is low, it is necessary to eat in small portions, 5-6 times a day with an interval of 3-3.5 hours;
- It is recommended to drink a glass of warm boiled water half an hour before each meal;
- a single serving of food should not exceed 200-300 grams;
- products entering the stomach must be in crushed form;
- food processing should be carried out by stewing, boiling, steaming, baking;
- Salty, bitter, spicy, hot and cold foods are prohibited;
- In between meals, it is recommended to drink up to one liter of still mineral water.
Strict adherence to all nutritional rules will allow you to quickly restore the function of parietal cells, thereby increasing the secretory function of the stomach.
Products that increase acidity
The diet of a patient suffering from gastritis with low acidity should not only be complete, containing sufficient proteins, fats, and carbohydrates, but also help increase the pH of gastric juice. Products that increase stomach acidity are required in the daily menu of patients:
- dried white bread, biscuits, crackers;
- first courses in vegetable or weak meat broth from dietary varieties of chicken and turkey;
- low-fat fish;
- porridge from rice, oatmeal, buckwheat, semolina;
- fermented milk products in the form of kefir, cottage cheese, low-fat sour cream;
- vegetable oil in small quantities;
- boiled or stewed vegetables - carrots, beets, zucchini, potatoes;
- mandatory inclusion of juices from fresh berries and fruits to prevent the development of hypovitaminosis;
- baked ripe fruits;
- compote of dry or fresh fruits, weak green tea, still mineral water;
- chopped sauerkraut in small quantities;
- lemons, sour apples.
When does hydrochloric acid production begin?
The production of hydrochloric acid begins the moment food enters the digestive organ.
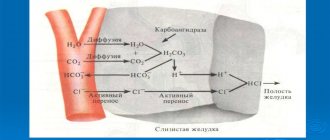
On an empty stomach, bicarbonate production occurs, but little of it is released. The release of hydrochloric acid starts in parallel with the entry of the food bolus into the stomach. It mechanically and chemically irritates surface cell receptors, signaling the need for the release of enzymes and bicarbonates. Hydrochloric acid is synthesized in order to convert inactive pepsinogen into the active form of the enzyme - pepsin.
What slows down or, on the contrary, stimulates the process?
If the production of enzymes and hydrochloric acid is reduced, symptoms of indigestion occur. The visceral nervous system, including the vagus nerve, stimulates an increase in the production of these substances. If its function is impaired, enzyme replacement therapy may be needed. The following factors slow down secretory function:
- the nature of the food consumed;
- increased acidity in the duodenum;
- disorders of the nervous system.
Some foods and inflammatory processes in the gastrointestinal tract stimulate the secretion of enzymes and hydrochloric acid. Helicobacter pylori is a bacterium that causes gastritis. When they are introduced, there is a high risk of the formation of an ulcer, therefore, if detected, it is recommended to take antacids. These agents reduce the pH of the stomach and restore damaged mucous membranes. In case of hyposecretion, on the contrary, drugs are used that stimulate the exocrine function of glandular cells.
What is hypersecretion?
Excessive consumption of acidic foods can lead to hypersecretion of the digestive organ.
This is increased secretion of gastric juice in response to external and internal factors. Gastric hypersecretion occurs when there is a high concentration of extractives in food. These include seasonings, sour foods, and alcohol. The cause of the pathology is a violation of the visceral innervation of the gastrointestinal system. Inflammatory pathologies of the gastrointestinal tract, for example, gastritis, also affect increased secretion production. Irregular nutrition and inconsistent daily routine often become provocateurs of hypersecretion.
What is hyposecretion?
This is a violation of the secretory function of the stomach in the direction of reducing the production of enzymes and hydrochloric acid. This condition causes symptoms of indigestion. It appears with certain types of gastritis, poor diet and lifestyle. With insufficient secretion of the gastric glands, part of the food passes into the underlying parts of the gastrointestinal tract undigested. This provokes fermentation processes. The breakdown products of undigested foods are absorbed into the intestinal wall and poison the body.
DRUGS USED FOR INCREASED SECRETION OF STOMACH GLANDS
With increased secretion of the gastric glands, a syndrome develops associated with an increase in the production of hydrochloric acid by the parietal cells, which results in an increase in the activity of pepsin, the excretion of the main cells of the gastric mucosa. An increase in the production of hydrochloric acid and an increase in pepsin activity leads to a decrease in the production of mucin, the main component of the mucus that covers the mucous membrane of the stomach and intestines. Hyperacidity, increased pepsin activity and lack of mucin predispose to damage to the mucous membrane of the stomach and duodenum (inflammation, erosion, ulcers) and contribute to the development of the syndrome of increased activity of the acid-peptic factor.
For pathogenetic therapy of patients with this syndrome, three subgroups of drugs are used:
1. Drugs that reduce the function of the gastric glands or inhibitors of gastric secretion:
a) M-anticholinergics;
b) ganglion blockers; c) tranquilizers;
d) H-2-histamine blockers;
e) proton pump blockers.
2. Antacids, that is, drugs that neutralize hydrochloric acid.
3. Agents that protect the mucous membrane of the stomach and duodenum from acid-peptic effects and improve reparative processes (film-forming agents).
Drugs that reduce the secretion of gastric glands include, first of all, M-anticholinergic agents. As a rule, these are non-selective drugs: ATROPINE and atropine-like drugs (PLATIFILLINE, METACIN). These drugs reduce the basal and nocturnal secretion of gastric juice and hydrochloric acid. However, it should be said that M-anticholinergic blockers of non-selective action reduce gastric contractions and tone to a greater extent than they affect the secretion of glands. The limitation of the use of M-anticholinergic drugs is also due to the wide range of effects that they cause, in addition to the effect on the gastrointestinal tract (tachycardia, dry mucous membranes, blurred vision). Therefore, M-anticholinergic blockers of non-selective action are currently assigned a secondary role in the treatment of patients with peptic ulcers, gastritis, and erosions; they are used only in combination with other drugs. At the same time, of great interest are the drugs created in the 80s that selectively block predominantly M-1-cholinergic receptors of the stomach, in particular PIRENZEPIN (GASTROCEPIN; Gastrocepinum; in tablets 0.25). It is a tricyclic compound that is a benzodiazepine derivative. All effects
pirenzepine have a peripheral effect, since the blood-brain barrier is impenetrable to it.
Pharmacodynamics of the drug: blocking M1-cholinergic receptors of the parasympathetic ganglia of the stomach. In addition, pirenzepine selectively blocks M1-cholinergic receptors of parietal cells (G-cells) that produce gastrin (the most powerful causative agent of hydrochloric acid secretion). Unlike atropine, pirenzepine (gastrocepin) does not have an atropine-like effect on the heart, smooth muscles of the stomach, gastrointestinal tract, gall bladder, and blood vessels; inhibits basal and stimulated by pentagastrin and insulin gastric secretion; has a cytoprotective effect on the gastric mucosa. The drug is prescribed 100-150 mg 2 times a day.
Ganglionic blockers (BENZOHEXONIUM, PYRYLENE, PENTAMINE) reduce both the total volume of gastric secretion and the content of hydrochloric acid in gastric juice, but the non-selectivity of their action on the autonomic ganglia creates a lot of side effects. Therefore, ganglion blockers are used only in extremely severe cases of peptic ulcer.
Tranquilizers (diazepam) can also reduce the nocturnal secretion of the gastric glands, however, this subgroup is rarely used for this purpose.
A new word in the treatment of peptic ulcer disease is the creation by English pharmacologists in the late 70s of new antisecretory drugs called H2-histamine blockers, that is, drugs that block histamine H2 receptors.
Histamine has recently been shown to play a key role in the production of hydrochloric acid. Under its influence, the secretion of hydrochloric acid sharply increases.
H2-histamine receptor blockers are among the most powerful known drugs that inhibit gastric secretory function. As is known, there are two types of histamine receptors: - H1-histamine receptors, which are localized in small arterial vessels, bronchi, smooth muscles of the intestine, and heart;
Agents that block these receptors (diphenhydramine, tavegil, etc.) eliminate the effects of histamine on the corresponding organs. — H2-histamine receptors are located in the parietal cells of the gastric mucosa, in the myometrium, and also in some vessels.
Drugs that block this type of receptor reduce the secretion of gastric juice. H2-histamine blockers most clearly suppress basal and nocturnal secretion.
There are three generations of H2-histamine blockers, the representative of the first generation is CIMETIDINE (Histodil, Gedeon Richter, Tagamet; Cimetidinum; in tablets of 0, 2 and in amps of 2 ml of 10% solution), a very effective drug, synthesized 10-15 years ago. Cimetidine reduces the motor function of the stomach, reduces the secretion of pepsin, the volume of gastric juice and the content of hydrochloric acid in it. At a dose of 400 mg, the drug inhibits acid secretion by 83%, 200 mg - by 70% (1 ml of atropine by 33.4%, 2 ml by 59%; metacin - by 30.24% and 60.34%, respectively). The duration of antisecretory action is 6-8 hours.
Cimetidine is more effective for duodenal ulcers than gastric ulcers.
Cimetidine is prescribed three times a day after meals and once at night. Side effects: headache, dizziness, weakness, nausea, diarrhea, constipation, rarely - loss of consciousness. Cimetidine has negative chrono- and inotropic effects and positive dromotropic effects; inhibits the activity of microsomal liver enzymes, and therefore prolongs the effect of sleeping pills, tranquilizers, anaprilin; promotes compensatory release of histamine, which can worsen the condition of patients with bronchial asthma. A big disadvantage of cimetidine is its ability to block androgen receptors, which leads to oligospermia, in boys - to delayed sexual development, in adults - to impotence, gynecomastia. In addition, this drug can cause neutropenia, thrombocytopenia, and anemia. If the drug is suddenly discontinued, a relapse of the disease is possible.
The drug is indicated for peptic ulcers of the stomach, intestines, reflux esophagitis, Zollinger-Ellison syndrome, erosions (when taking steroids).
Another drug of this class, belonging to the second generation of H2-histamine blockers, was released abroad - RANITIDINE (ZANTAC, RANISAN; Ranitidini hydrochloridum; in tablets of 0, 15 and 0, 3). The drug is similar in its pharmacological effects to cimetidine, but is free from antiandrogenic effects, and is also more active (5-10 times) and has higher blocking activity and selectivity for H2-histamine receptors than cimetidine. Ranitidine is also less toxic.
There are drugs H-2-histamine blockers of the third generation, in particular, famotidine (KVAMATEL "Gedeon Richter", GASTROSIDINE, ULFAMIDE).
It is advisable to combine H2-histamine blockers with M-anticholinergic blockers, in particular with gastrocepin.
Proton pump inhibitors, in particular OMEPRAZOLE (Omeprasolum; in the table 0.03) - an inhibitor of the proton pump of parietal cells, inhibits the production of hydrochloric acid in the stomach. Suppression of hydrochloric acid secretion occurs due to selective inhibition of the activity of H, K-adenosine triphosphatase of the proton pump of parietal cells, an enzyme that controls the last stage of the release of secreted acid into the stomach. The drug inhibits nocturnal and stimulated gastric secretion by 90-100%, that is, it is one of the most powerful inhibitors of gastric secretion. Omeprazole also has a prolonged action, a faster symptomatic effect and promotes faster healing of duodenal ulcers than ranitidine.
The drug is indicated for ulcers, erosions (due to taking NSAIDs, hormones), Zollinger-Ellison syndrome during maintenance therapy.
This drug has a therapeutic effect for duodenal ulcers of any size and regardless of whether the patient smokes or not. Prescribe 20 mg once a day in the morning. In the first two weeks of taking omeprazole, patients feel better, and the majority (77%) have pain disappearance.
Side effects: nausea, diarrhea, numbness of fingers.
ANTACIDS
This group includes agents that neutralize hydrochloric acid and reduce the acidity of gastric juice. These are anti-acid drugs. Usually these are chemical compounds with the properties of weak bases, and they neutralize hydrochloric acid in the lumen of the stomach. Reducing acidity is of great therapeutic importance, since the activity of pepsin and its digestive effect on the gastric mucosa depend on its amount. The optimal pH value for pepsin activity ranges from 1.5 to 4.0. At pH = 5.0, pepsin is inactive.
Therefore, it is desirable that antacids raise the pH no higher than 4.0 (it is optimal that when taking antacids, the pH of the gastric juice is 3.0-3.5), which does not interfere with the digestion of food. Typically, the pH of gastric contents normally fluctuates between 1.52.0. The pain syndrome begins to subside when the pH becomes more than 2. In this sense, the role of antacids is twofold.
There are systemic and non-systemic antacids. Systemic antacids are drugs that can be absorbed, and therefore not only produce effects in the stomach, but can also lead to the development of alkalosis in the body as a whole. Non-systemic antacids are not absorbed, and therefore are able to neutralize acidity only in the stomach, without affecting the acid-base state of the body.
Antacids include SODIUM HYDROCARBONATE (baking soda), CALCIUM CARBONATE, ALUMINUM and MAGNESIUM HYDROXIDE, magnesium oxide. Typically, these substances are used in different dosage forms and in different combinations.
Systemic antacids include sodium bicarbonate and sodium citrate, while the rest of the above drugs are non-systemic.
Sodium bicarbonate (baking soda) is a compound that is highly soluble in water and reacts quickly in the stomach with hydrochloric acid. The reaction proceeds with the formation of sodium chloride, water and carbon dioxide. The drug acts almost instantly. Although sodium carbonate acts quickly, its effect is short-lived and weaker than that of other antacids. The carbon dioxide formed during the reaction stretches the stomach, causing bloating and belching. In addition, taking this drug may be accompanied by “recoil” syndrome. The latter is that a rapid increase in pH in the stomach leads to the activation of parietal G cells in the central part of the stomach, which produce gastrin. Gastrin stimulates the secretion of hydrochloric acid, which leads to the development of hyperacidity after the cessation of the action of the antacid. Typically, the “recoil” syndrome develops after 20-25 minutes. Due to good absorption from the gastrointestinal tract, sodium bicarbonate can cause systemic alkalosis, which will be clinically manifested by decreased appetite, nausea, vomiting, weakness, abdominal pain, spasms and muscle cramps. This is a rather dangerous complication that requires immediate discontinuation of the drug and assistance to the patient. Due to the severity of these side effects, sodium bicarbonate is used extremely rarely as an antacid.
Non-systemic antacids, as a rule, are insoluble, act in the stomach for a long time, are not absorbed, and are more effective. When using them, the body does not lose either cations (hydrogen) or anions (chlorine), and there are no changes in the acid-base state. The effect of non-systemic antacids develops more slowly, but is longer lasting.
First of all, it should be mentioned:
1) aluminum hydroxide;
2) magnesium oxide.
ALUMINUM HYDROXIDE (aluminum hydroxide; Aluminii hydroxydum) is a drug with a moderate antacid effect, it acts quickly and effectively, and a significant effect appears after about 60 minutes.
The drug binds pepsin, reduces its activity, suppresses the formation of pepsinogen and increases mucus secretion. One gram of aluminum hydroxide neutralizes 250 ml of decinormal hydrochloric acid solution to pH = 4.0.
In addition, the drug has astringent, enveloping and adsorbing effects.
Side effects: not all patients tolerate the astringent effect of the drug well, which may result in nausea; Taking aluminum preparations is accompanied by constipation, so aluminum-containing preparations are combined with magnesium preparations. Aluminum hydroxide promotes the removal of phosphates from the body.
The drug is indicated for diseases with increased secretion of gastric juice (hydrochloric acid): ulcers, gastritis, gastroduodenitis, food poisoning, flatulence. Aluminum hydroxide is prescribed orally in the form of a 4% aqueous suspension, 1-2 teaspoons per dose (4-6 times a day).
Magnesium oxide (Magnesii oxydum; powder, gel, suspension) - burnt magnesia - is a strong antacid, more active than aluminum hydroxide, acts faster, lasts longer and has a laxative effect.
Each of the listed antacids has a certain range of advantages and disadvantages. In this regard, their combinations are used.
The combination of aluminum hydroxide in the form of a special balanced gel, magnesium oxide and D-sorbitol made it possible to obtain one of the most common and effective antacid drugs at present - ALMAGEL (Almagel; 170 ml; the drug was named from the words al-aluminum, ma-magnesium , gel-gel). The drug has an antacid, adsorbent and enveloping effect. The gel dosage form promotes uniform distribution of ingredients over the surface of the mucous membrane and prolongs the effect. D-sorbitol promotes bile secretion and laxation.
Indications for use: stomach and duodenal ulcers, acute and chronic hyperacid gastritis, gastroduodenitis, esophagitis, reflux esophagitis, Zollinger-Ellison syndrome, pregnancy heartburn, colitis, flatulence, etc.
There is a drug called Almagel-A, in which, in addition to the composition of Almagel, anasthesin is added, which has both a local anesthetic effect and suppresses gastrin secretion.
Almagel is usually used 30-60 minutes before meals, and also within an hour after meals. The drug is prescribed individually depending on the localization of the process, the acidity of gastric juice, etc.
Preparations similar to Almagel:
— gastrogel (Czechoslovakia);
— phosphalugel (Yugoslavia) contains aluminum phosphate and colloidal gels of pectin and agar-agar, which bind and absorb toxins and gases, as well as bacteria, reduce the activity of pepsin;
— Megalak (Germany);
— mylanta (USA) contains aluminum hydroxide, magnesium oxide and simethicone;
- Gastal (Yugoslavia) - tablets, which contain: 450 mg of aluminum hydroxide - magnesium carbonate gel, 300 mg of magnesium hydroxide.
Currently, the most popular drug from the group of antacids in many countries around the world is the drug MAALOX (Maalox) from the French company Rhone-Poulenc Rorer. The composition of the drug includes aluminum hydroxide and magnesium oxide. Maalox is available in the form of a suspension and tablets; 5 ml of Maalox suspension contains 225 mg of aluminum hydroxide, 200 mg of magnesium oxide and neutralizes 13.5 mmol of hydrochloric acid; The tablets contain 400 mg of aluminum hydroxide and magnesium oxide, so they have higher acid-neutralizing activity (up to 18 mmol of hydrochloric acid). Maalox-70 is even more active (up to 35 mmol of hydrochloric acid).
The drug is indicated for gastritis, duodenitis, peptic ulcer of the stomach and duodenum, reflux esophagitis.
There are practically no side effects. MEGALAK (Megalac) is a German drug, an analgesic antacid (hydrous aluminum-magnesium silicate). It contains 0.2 aluminum oxide, 0.3 magnesium oxide and 0.02 oxetain.
TOPALCAN is a French antacid drug. It contains alginic acid, colloidal aluminum hydroxide, magnesium bicarbonate, hydrated silicon in a precipitated shapeless state. The drug has a foaming effect, forms a gel on the surface of the liquid contents of the stomach, and covers the mucous membrane; acts quickly (6-14 minutes) and for a long time (2-4 hours). Beneficial for esophagitis, reflux esophagitis.
Symptoms of the disorder
Hypersecretion of gastric juice is manifested by heartburn, belching of acidic stomach contents or air. Sometimes there is pain in the epigastric region, a feeling of rapid satiety. Reduced secretion manifests itself as flatulence. It occurs due to the accumulation of insufficiently digested food in the intestines, fermentation and the release of gases. Reduced secretion prevents sufficient nutrients from entering cells and tissues. Anemia often develops with this pathology.
Symptoms
Laxatives
Clinical manifestations of increased gastric acidity usually differ little, given the reasons for its increase. So, the following are the main symptoms of high stomach acidity:
Heartburn. A mandatory sign of a change in acid level is heartburn. This clinical manifestation is not critical, but it causes a lot of discomfort. Considering the root cause of its occurrence, heartburn can occur immediately after eating or after some time. The appearance of regular attacks of heartburn is a sign that it is associated with an existing disease, and not with errors in the diet. Under such circumstances, it will be easiest to reduce stomach acidity at home.
- Pain in the left epigastric region. Excessive amounts of hydrochloric acid have a traumatic effect on the walls of the stomach, which leads to pain. How severe the pain is depends on the etiological factor. So, with gastritis, the pain will be moderate, and with a peptic ulcer, it will be significant. Sometimes, pain may require the use of analgesics.
- Dyspeptic disorders. A change in the normal digestive process results in a number of changes in the digestive system, such as diarrhea, nausea or vomiting. The latter may appear regardless of food intake. This is due to the fact that due to the inflammatory process, the stomach receptors are constantly irritated, perceiving an empty stomach as full. The appearance of such symptoms can also occur during the use of drugs that reduce gastric acidity, due to their side effects.
- Deterioration in general health. If the hyperacid state is caused by a disease, then a general reaction of the body may occur, in the form of an increase in body temperature to low-grade levels, decreased appetite, and general malaise.
Before choosing a way to get rid of high stomach acidity, you need to consult a doctor to determine the cause of this condition.