Intestinal candidiasis is a fungal infection of the mucous membrane of the digestive tract. Due to the global distribution of fungi of the genus Candida, there are difficulties in diagnosing and determining the criteria for the disease. Fungi are normally present in the microflora, but it is not always clear at what levels it can be considered that they are the causative agent of inflammation.
Note that candidiasis of the gastrointestinal tract is based on the “spreading” of fungi throughout the digestive tract. However, the majority of diagnosed cases of candidiasis occur in the intestines. Other areas of the gastrointestinal tract are susceptible to inflammation, but to a lesser extent.
There is a nuance in diagnosing and subsequently prescribing a course of treatment - the tactic of prescribing antimycotics at the first detection of Candida fungi in crops, without further examination, is erroneous.
This means that to establish a correct diagnosis, three diagnostic criteria must be present:
- – identification of one or more risk factors,
- – endoscopic signs of intestinal candidiasis,
- – positive culture result.
If the criteria are not fully collected, then it is impossible to say about the localization of candidiasis in the intestines. Perhaps the thrush has “spread” throughout the digestive tract.
What is intestinal candidiasis
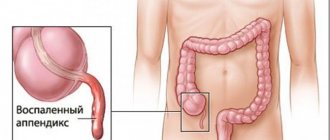
The digestive tract is a rather complex system of the human body. Since the structure of the tract has a large area of mucous membrane, it is preferable to place fungal colonies in it. Naturally, under certain conditions, fungal colonies strike in the form of candidiasis. The mucous membrane becomes inflamed.
Candidiasis of the gastrointestinal tract is an infectious and inflammatory lesion of the gastrointestinal tract by fungi of the genus Candida. Gastrointestinal thrush may be accompanied by candidiasis of the esophagus, stomach or intestines.
For reference. Gastrointestinal candidiasis, manifested by fungal infection of the stomach and esophagus, most often occurs in patients with various immunodeficiencies.
Intestinal candidiasis refers to a variety of severe forms of dysbiosis, accompanied by toxic damage to the intestine and the development of secondary immunodeficiency .
The main symptoms of intestinal candidiasis are:
- bloating due to increased gas formation,
- stomach ache,
- diarrhea mixed with white flakes.
Pathogenesis of intestinal candidiasis
Candida fungus normally coexists next to the normal intestinal microflora. Under certain conditions, it begins to multiply and cause a disease - candidiasis.
The fungus loves high humidity, temperatures 21-40 ºС, and pH 6-6.5. Candida can exist in the form of blastospores - these are young round or oval cells.
When exposed to favorable conditions, the fungus begins to budding intensively, forming a chain - pseudomycelium.
After candida enters the intestines or oral cavity, the fungus attaches to the epithelium - adhesion. This occurs due to special fungal adhesion factors.
For reference. Candida prefers stratified squamous epithelium for attachment. Therefore, the favorite localization of the fungus is the oral cavity and esophagus. But candidiasis of the stomach and intestines occurs, where single-row columnar epithelium is located.
After Candida adheres to the epithelium, it begins to actively multiply. A fungal mass accumulates. But this process is normally hampered by the protective factors of the body in general and the intestines in particular. If the defense mechanisms are strong, then the body does not allow the fungal colonies to exceed a critical mass.
The fungus can coexist with normal microflora for some time and be present in small quantities. At the same time, do not cause painful manifestations. This situation is bacterial carriage.
If the protection is compromised, candida multiplies in the intestines and fungal mass accumulates. At the same time, toxins, waste products of the fungus, are actively absorbed into the blood, causing intoxication and allergization of the body, and oligosaccharides, which are part of the cell wall of the pathogen, disrupt the functioning of the protective factors of the immune system. This form of the existence of fungus in the intestines is called non-invasive candidiasis.
With significant suppression of immunity, invasion (penetration) of candida occurs into the thickness of the epithelium, as well as into the lamina propria of the mucosa. This releases enzymes that destroy host tissue. Invasive intestinal candidiasis develops.
Then the fungus spreads through the blood vessels throughout the body and penetrates into the internal organs: liver, heart, lungs, pancreas, where it begins to multiply. This is visceral candidiasis.
Important. The intestines always serve as a source of spread of fungi to other organs.
Non-invasive intestinal candidiasis
Non-invasive forms of intestinal candidiasis are much more common than invasive ones. Non-invasive intestinal candidiasis develops against the background of a disturbance in the natural balance of intestinal microflora and active reproduction of candida in the intestinal lumen.
At the same time, candida does not penetrate into the thickness of the intestinal mucosa, causing only superficial inflammation of the mucosa. Toxic substances secreted by candida provoke further progression of intestinal dysbiosis and lead to the development of secondary immunodeficiency states.
For reference. Against the background of progressive dysbiosis, inflammation and decreased immunity, activation of other opportunistic and pathogenic microorganisms is often observed, provoking the development of fungal-bacterial, fungal-protozoal, mixed-fungal and other infections.
Invasive intestinal candidiasis
Invasive forms are practically never found in people with normal immunity. In most cases, this form of the disease occurs in immunodeficient patients.
Factors contributing to the development of intestinal candidiasis
Since Candida fungi are part of the normal intestinal microflora, the development of candidiasis occurs when the natural balance of microorganisms is disrupted, the number of beneficial lactobacilli is reduced and the increased proliferation of Candida fungi occurs.
For reference. Activation of candida reproduction against the background of microflora disturbance leads to the development of an inflammatory process and intestinal candidiasis.
Risk factors contributing to the development of intestinal candidiasis are:
- long-term use of antibacterial agents (inhibit the natural intestinal microflora and can provoke the development of dysbacteriosis);
- taking glucocorticosteroids or drugs that have an immunosuppressive or cytostatic effect (they reduce immunity and promote increased growth of Candida and other opportunistic microflora);
- pregnancy (mild intestinal candidiasis in women often develops against the background of decreased immunity during pregnancy);
- alcohol abuse;
- protein deficiency in food (low protein diets);
- oncological diseases;
- chemotherapy or radiation therapy;
- severe obesity;
- diabetes.
For reference. In newborns, the main risk factor for the development of gastrointestinal candidiasis is the mother's taking antibacterial drugs that are incompatible with natural feeding without temporarily stopping breastfeeding.
In this case, the antibiotic taken by the mother penetrates into breast milk and leads to inhibition of the gastrointestinal microflora in the child, provoking the development of dysbiosis and intestinal candidiasis.
Causes and routes of transmission
Gastric thrush is a common type of fungal pathology. There is only one reason for the pathology - the negative impact of the Candida fungus on the body. But the disease develops only when the body’s defenses are weakened. Neither at the initial stage, nor during the further course of the disease, the properties of the pathogen itself do not change, it does not become more aggressive. The immune system is simply weakened.
Sources of fungal infection
Quite often, candidiasis of any localization gets the opportunity to develop due to severe infections, all kinds of immunodeficiencies, and the presence of diabetes mellitus. The likelihood of pathology occurring is increased by malignant tumors, their treatment with aggressive drugs, and uncontrolled use of corticosteroids or antibiotics.
These same reasons become the impetus for the occurrence of candidiasis. So, most often the following factors become provocateurs for the development of the disease:
- Presence of peptic ulcer or gastritis. Any chronic disease accompanied by long-term relapses contributes to a decrease in immunity.
- Necrotic changes in some areas of the gastrointestinal tract.
Prolonged and excessive use of corticosteroids or antibiotics.- Malignant neoplasms in the intestinal or stomach area.
- Damage to the mucous membranes of both the oral cavity and internal organs.
- Chronic pathologies of the respiratory and urinary systems.
- Low acidity of gastric juice.
The development of candidiasis can also be provoked by prolonged excessive use of alcohol or drugs, or smoking. The fact of age should also be taken into account - the risk of infection is higher in people of the older age group.
To exclude the possibility of infection from a sick person, you need to know how thrush is transmitted. You can get infected from a sick person in the same ways as with other types of pathology:
- through saliva (through dishes, when sharing any food product or during a kiss);
- through household items, especially hygiene products;
- sexually.
Intestinal candidiasis - classification
According to the official classification, the following types of intestinal candidiasis are distinguished:
- invasive diffuse;
- focal (complicating duodenal ulcers, developing as a complication of ulcers in nonspecific ulcerative colitis);
- non-invasive (accompanied by excessive proliferation of candidal fungi in the intestinal lumen against the background of disruption of the natural microflora).
Also, intestinal candidiasis can be combined with anorectal candidiasis:
- invasive candidiasis of the rectum;
- perianal candidal dermatitis.
Causes of the disease
A fungus in the stomach is always a consequence of a weakening of the body’s defense system. Immunodeficiency can occur against the background of:
- taking antibacterial drugs;
- course of cytostatics, glucocorticosteroids;
- restoration of the body after serious illnesses, long-term colds, surgical interventions;
- hormonal fluctuations;
- pregnancy;
- endocrine disorders;
- hypothermia;
- stress.
The more factors that reduce immunity are observed, the higher the likelihood of encountering candidiasis.
Fungus in the stomach rarely occurs as an independent disease. It usually accompanies candidiasis in other parts of the digestive system, such as the intestines. Sometimes it occurs against the background of ulcerative colitis, chronic gastritis, or Helicobacter pylori infection.
Intestinal candidiasis - symptoms
Symptoms of candidiasis do not differ between men and women. The main manifestations of the disease are:
- bloating;
- stomach ache;
- nausea;
- diarrhea mixed with white flakes or lumps;
- a large amount of mucus in the stool;
- weakness, irritability, loss of appetite due to intoxication;
- increased body temperature;
- flatulence.
Mild forms of the disease can only manifest as flatulence and periodic diarrhea.
With the development of invasive intestinal candidiasis, erosions, ulcers and cracks in the intestinal mucosa develop. In this case, the patient is worried about intense abdominal pain, the release of streaks of blood in the stool, high body temperature and severe intoxication. Patients are lethargic, irritable, complain of nausea, chills, muscle and joint pain.
Mesenteric lymph nodes may also enlarge and acute mesadenitis may develop.
Focal forms of intestinal candidiasis complicate ulcerative lesions of the duodenum in peptic ulcer disease, ulcers in ulcerative colitis or Crohn's disease. With focal forms of candidiasis, the patient experiences abdominal pain, blood in the stool, weakness, nausea, diarrhea, and bloating.
Also, intestinal candidiasis (in any form) is often combined with candidiasis of the perianal area. Patients are concerned about itching, burning in the anal area, and the appearance of anal fissures. Also characteristic is redness of the skin in the perianal area, the appearance of a white coating and a rash on the skin.
Diagnosis of gastrointestinal candidiasis
The diagnosis process is, of course, based on all the symptoms that the doctor identifies during a conversation with the patient and during the initial examination. However, such a disease requires additional examinations and tests.
It is quite difficult to determine candidiasis of the stomach, because it is usually accompanied by problems with the intestines and other digestive organs. This gives a blurry picture of the symptoms.
In this case, you cannot do without the unpleasant but effective procedure of gastroendoscopy. This method of examination allows you to see the condition of the internal organs and take tissue samples for study.
The procedure is carried out with an empty stomach. This can be achieved if a person does not eat for about 20 hours.
Typically, gastroendoscopy is performed in the morning, so the patient is prohibited from eating food from 6 pm the previous day. Sometimes it is recommended to do an enema the day before.
Since a diseased stomach usually produces a lot of mucus, the patient must take a special drug before endoscopy. This is done 10–15 minutes before the start of the examination.
The condition of the stomach lining is visually assessed, areas of erosion, ulceration, and the appearance of neoplasms are identified. In this case, the doctor must pinch off a piece of stomach tissue to conduct cytological and bacterial tests.
If candidiasis is suspected, the polymerase chain reaction method is also used. It gives quick results because it is based on laboratory analysis of the patient's stool and vomit. In this case, endoscopy is resorted to only if the formation of erosion, ulcers and perforation is suspected.
Treatment can be prescribed only after a complete examination, since an incorrect diagnosis leads to serious consequences.
Intestinal candidiasis in a child
Intestinal candidiasis is especially common in children under three years of age and infants. The child’s immune system is just developing and the fragile body cannot resist the onslaught of pathogenic bacteria and various infections.
In newborns, the condition is complicated by intestinal dysfunction, which is manifested by bloating, increased gas formation and stool disorder.
Small moist formations may appear around the anus, causing discomfort to the baby.
The main manifestations of intestinal candidiasis in children and adults are similar. The disease is manifested by bloating, pain, weakness, diarrhea mixed with white lumps.
The temperature in children with intestinal candidiasis increases more often than in adults.
Infants often become whiny, lethargic or restless, refuse to eat, and often burp.
It should also be noted that in children, diarrhea quickly leads to dehydration and electrolyte imbalance.
For reference. In protracted, mild forms of the disease in young children, progressive intestinal dysbiosis and periodic diarrhea lead to vitamin deficiency, impaired absorption of micro- and macroelements in the intestines, as well as developmental delays, weight gain and growth.
Generalized forms
In patients with severe immunodeficiencies or decompensated forms of diabetes mellitus, a generalized form of intestinal candidiasis may develop.
For reference. As a rule, generalization of fungal infection is observed with invasive candidiasis. After filamentous forms of candida penetrate into the blood, they spread throughout the body, leading to damage to the kidneys, liver, spleen, and pancreas.
Generalization of the infection is manifested by a sharp deterioration in the patient’s condition, the appearance of severe weakness, high fever, lethargy, lethargy, nausea and vomiting, intense abdominal pain, blood clotting disorders and the appearance of bleeding.
Intestinal candidiasis - diagnostic scheme
The main difficulty in diagnosing intestinal candidiasis lies in the differential diagnosis between simple candidiasis (which is a physiological condition that does not require treatment) and intestinal candidiasis.
For reference. The absolute diagnostic sign of candidiasis is the identification of candidal fungi in sterile fluids (cerebrospinal, prostate, peritoneal) or tissues.
Difficulties in diagnosis lie in the fact that pseudomycelium of fungi cannot be detected in all samples of material, therefore false negative results are quite common.
With invasive intestinal lesions, signs of ulcerative-necrotic intestinal lesions and filamentous forms of fungus in biopsy specimens due to ulcers on the intestinal mucosa are revealed.
For reference. To increase the information content of histological examination, biopsy samples are taken from different areas of the mucosa (at least 3-5 samples).
The diagnostic criterion for invasive intestinal candidiasis is the presence of candidal pseudomycelium in biopsies and prints of the intestinal mucosa.
Microscopy of samples is carried out using the PAS reaction (chromic acid treatments) or Gridley staining. This test allows you to detect candida in smears or tissue samples by staining the polysaccharides of the fungal cell wall. However, these techniques are used to identify invasive forms of Candida fungus.
To diagnose non-invasive forms of intestinal candidiasis, smears are colored using hematoxylin and eosin staining. Romanovsky-Giemsa stain also allows the identification of pseudomycelia in smears and impressions from the mucous membranes or the bottom of intestinal ulcers.
Cultures on Sabouraud nutrient media or methods for rapid identification of fungi can also be used. Additionally, culture is carried out for sensitivity to antibacterial drugs.
Serological tests can also be used to diagnose invasive forms of intestinal candidiasis. However, serological tests may give false-positive results in patients with candida carriage or sensitization to fungi. In immunodeficiencies, false-negative serological reactions may occur.
Modern laboratories can also use special diagnostic kits aimed at identifying antibodies and antigens of fungal metabolites (Pastorex Candida, based on latex agglutination reactions).
Diagnostics
To make a diagnosis, contact a gastroenterologist. Special examinations are carried out in the clinic:
- Analysis of the symptoms described by the patient.
- Blood test for antibodies to the genus Candida. Lack of immunoglobulin in the blood is the main sign of the active influence of pathogenic microflora. The lack of antibodies does not allow blocking the growth of fungus in the gastrointestinal mucosa, so the disease begins.
- Taking smears with a cytological brush or balloon catheter from the mouth and esophagus. The materials are subjected to microscopic examination and inoculation in a nutrient medium. The objective of the study is to determine the type of microorganism for the selection of an antimycotic drug.
- Study of vomit and feces. Spores and mycelium of the fungus in these materials confirm the diagnosis.
The most informative diagnostic method is endoscopic examination of the esophagus and stomach. Examination with an endoscope allows you to assess the condition of the mucous membrane, take tissue for histological analysis, and materials for culture.
During this examination, the doctor may begin treatment by cauterizing the bleeding and removing the polyp.
IMPORTANT! Sowing gastric juice helps determine the type of fungus, as well as determine the body’s immunological reaction: determine whether antibodies are produced to it.
How to treat intestinal candidiasis
Treatment of gastrointestinal candidiasis depends on the severity and form of the disease. Non-drug treatment of intestinal candidiasis includes diet and increased drinking regimen.
It is necessary to exclude the intake of alcoholic drinks, soda, salty, fried, fatty and spicy foods, sweets, and flour.
Treatment of intestinal candidiasis is carried out in three different areas:
- destruction of the pathogenic bacterium;
- normalization of healthy intestinal microflora and restoration of organ functions;
- strengthening the immune system (treatment of pathological conditions that led to its decrease).
Drug treatment is based on the prescription of antifungal drugs that are not adsorbed from the intestinal lumen. When treating intestinal candidiasis, natamycin (Pimafucin) is considered the drug of choice. Pimafucin tablets are practically not absorbed from the gastrointestinal tract and are well tolerated by patients (however, vomiting, nausea, and diarrhea are possible in the first days).
Attention! The use of other antimycotic drugs (levorin, nystatin, fluconazole) for intestinal candidiasis often leads to the development of severe side effects, including drug-induced hepatitis.
The only contraindication to the use of Pimafucin is the presence of individual intolerance to natamycin. The drug can be prescribed even to newborns and pregnant women.
The duration of treatment and dosage are selected individually.
Diet during treatment
The diet must be structured in such a way that it contains protein and high-fiber foods. Dishes are prepared boiled, stewed, steamed or baked.
The list of permitted products includes:
- protein lean meat, poultry and fish;
- non-starchy or moderately starchy vegetables, most of which should be eaten raw;
- seasonings that have an antifungicidal effect - garlic, bay, oregano, pepper, cinnamon, cloves;
- sauerkraut, seaweed and sprouted grains;
- natural yoghurts, starter cultures, biokefir;
- lingonberries, grapefruit, cranberries, viburnum, currants, other fruits and berries high in nutrients, vitamins, antioxidants;
- among drinks, it is better to give preference to decoctions of herbs, black currants, rose hips, and rowan;
- Green tea, carrot and pomegranate juices, clean water with lemon are allowed.
What not to eat if you have intestinal candidiasis
It is necessary to remove simple carbohydrates, honey, sugar, sweet syrups and chocolate from the diet. Yeast bread, artificial additives and sweeteners will not benefit a weakened body. The recommended daily dose of carbohydrates should not exceed 60 grams.
A diet for candidiasis involves avoiding:
- Sahara;
- baked goods, bread;
- dried fruits, jam, honey;
- sweets, chocolate;
- milk;
- potatoes, white rice and foods high in starch;
- carbonated drinks;
- sweet fruits.
Treatment of the disease
To treat the fungus, patients are prescribed special medications, but folk remedies can also be used as additional therapy. Advanced stages of candidiasis usually require hospitalization.
Drug therapy
To combat fungus in the stomach, approximately the following drugs are recommended for patients. Antimycotics are antifungal drugs used in the early and middle stages of the disease. These include:
- Nystatin is a highly effective remedy in the fight against fungi of the genus Candida. Can be used for preventive purposes. The average daily dose is 3–4 tablets. The course of treatment is about 2 weeks. The drug can be purchased at a cost of 135 rubles per package (100 pieces).
- Fluconazole is an antifungal agent used in the early stages. Adults are prescribed 4 capsules per day. The drug is produced individually, the average price is for 1 piece. is 33 rubles (150 mg). Price for 7 capsules of 50 mg - from 60 rubles.
- Lamisil is a broad-spectrum antifungal agent that inhibits the activity of fungi and prevents their reproduction. Daily dose - 1-2 tablets. The average price is from 2200 for 14 pieces.
Important!
Antibiotics for the treatment of candidiasis are not recommended, because they can further weaken the immune system and thereby cause the proliferation of fungi.
Products for restoring and normalizing intestinal microflora contain live cultures and are prescribed after a course of antifungal drugs. These include:
- Linex - adults are recommended to take 2 capsules 3 times a day (mainly after meals), with plenty of water. The average price is 280 rubles (16 pcs.).
- Lactofiltrum is a plant-based drug with an immunostimulating effect. It is recommended to take 2-3 tablets 1-1.5 hours before meals three times a day. The product can be purchased at a cost of 270 rubles (30 pcs.).
Drugs for intravenous injection - prescribed for severe stages of the disease. These include:
- Amphotericin - dosage is determined by the attending physician. The average cost is 37 rubles (10 ml).
- Ampholip - quickly distributed in organs and tissues, destroying the fungus. Patients are usually prescribed 1–3 ml per day. The average price is from 10,300 rubles (10 ml).
Important!
Before using this or that product, you must consult a specialist; self-medication is unacceptable. Otherwise, complications and irreversible consequences are possible.
Folk remedies
Folk remedies are applicable only in the early stages of the disease (as part of complex therapy). Here are some of them.
Herbal decoction with antifungal effect
Ingredients: sage, wormwood, oak bark powder, black poplar bud powder, goldenrod (1 tablespoon each).
Preparation: mix the ingredients and pour a glass of boiling water, heat in a water bath (15 minutes), drain and strain.
Application: consume 30–40 ml on an empty stomach. It is also recommended to treat the oral cavity: take it into your mouth and spit it out after a while (the duration of the procedure is 30–40 minutes). Use for 10 days, then take a 7-10 day break. In case of allergic reactions and deterioration of health, treatment should be stopped.
Freshly squeezed carrot juice
Squeeze the juice from fresh carrots and take 1 glass on an empty stomach. Use until the condition improves.
Oatmeal jelly
Preparation: pour 10 glasses of oats with water (7 liters). Cook for 3 hours over low heat, cool and strain.
Application: take 100 grams 3 times a day.
It is also recommended to eat garlic (2-3 cloves per day). But this method is strictly contraindicated for gastritis and stomach ulcers.