The prevalence of HCC in the global community is very high. According to M. Prokop, HCC accounts for up to 90% of all cases of liver tumors. Hepatocellular cancer is characterized by prevalence in certain regions of the world. Where the incidence of hepatitis B or C is high, the incidence of malignant liver tumors is also high. Most often, liver cancer, which, as a rule, can be detected in the early stages, occurs in residents of China, residents of the African continent and Asia (up to 150 cases per 100,000 people). Intermediate incidence rates are in South America (Argentina, Chile) - up to 10 cases per 100,000 population, low - in the USA (up to 3 cases per 100,000 people). Men get sick much more often – up to 8 times. The first signs of liver cancer in women are detected in risk groups (in people taking medications that have a toxic effect on the liver, as well as in people exposed to constant intoxication due to their work). The age peak of incidence occurs in the period 40-70 years.
Liver examination in St. Petersburg
Factors for the development of HCC
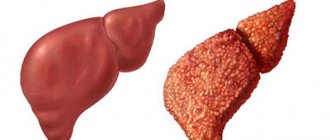
Most often, the onset of cancer is preceded by cirrhosis of the liver (up to 90% of all cases). What is the difference between these two concepts? Cirrhosis is the replacement of normal liver parenchyma with atypical connective tissue, which in itself is not an oncopathology, but is considered a significant predisposing factor in its development. Cirrhosis can be either alcoholic or caused by hepatitis B or C. Exposure to carcinogenic factors and chemicals is important: sicasin (a toxic substance contained in some types of palm oil), aflatoxin (a toxin produced by fungi - aspergillus), thorotrast (a contrast agent, used at the dawn of x-ray diagnostics). Patients with hereditary pathology (Wilson-Konovalov disease, hemochromatosis, tyrosinosis) are also at risk for the incidence of HCC. It is also possible for liver tumors to occur in patients exposed to radiation (including after the accident at the Chernobyl nuclear power plant and other facilities).
Diagnostics
Tool-free inspection
When the patient complains, palpation (feeling with fingers) and percussion (tapping with fingers) are used; during such studies, the structure and size of the liver are studied.
Blood and urine tests
There is an increased level of bilirubin in the blood, urine tests show the presence of urobilin (see transcript of the biochemical blood test). Such changes may indicate pathologies of the organ and disruption in its functioning. A specific test is to determine the level of alpha-fetoprotein (AFP) in the blood. Its increase is due to an increase in the number of immature liver cells.
Ultrasound
On the monitor of the device, disturbances in the size of the liver, its structure and density can be seen. Often the doctor sees the malignant tumor itself.
CT scan
Used to clarify the diagnosis. A special contrast agent can be used (injected intravenously), which allows a more detailed examination of the structure of the organ and the location of the vessels. It is possible to perform a CT scan without the use of a contrast agent.
Magnetic resonance imaging
Currently, the most effective way to diagnose a patient’s liver. Allows you to study the organ from different angles.
Biopsy
Examination of suspicious tissues for malignancy. For analysis, it is necessary to obtain a small part of the tissue that has raised doubts among the doctor. For these purposes, the abdominal cavity is punctured with a special needle under ultrasound control.
Laparoscopy
Special micro-instruments are inserted through small incisions in the peritoneum, making it possible to examine the diseased organ and at the same time take suspicious tissue for subsequent examination for malignancy.
Other techniques
You can see liver pathologies when examining it with X-rays or radioisotope scanning.
Is liver cancer curable?
Currently, several types of successful treatment for liver cancer are used. For small nodes (up to 2 cm), identified by CT or MRI, surgeons use radical tumor removal. For large nodes, as well as for multiple lesions, radiofrequency ablation is used - destruction of the tumor with special high-frequency waves, as well as liver transplantation. Liver transplantation for cancer is a complex operation that is increasingly being used successfully in Russia in large surgical centers. For large tumors, palliative treatment methods are used, such as transarterial chemoembolization (CEPA), as well as drug methods (Nexavar, sorafenib).
Risk factors
Regardless of whether liver cancer has metastasized or not, it is still necessary to resort to urgent treatment. It is important to diagnose a malignant tumor on time. Therefore, a routine medical examination never hurts. There is a group of people who are more predisposed to developing this cancer. The most common form of liver cancer is a consequence of cirrhosis. Other risk factors include:
- excess weight.
- diabetes mellitus (type 2).
- use of anabolic steroids.
- exposure to toxic substances (aflatoxin, vinyl chloride, arsenic).
- smoking addiction.
- certain rare diseases (tyrosinemia, alpha-1-antitrypsin deficiency, porphyria cutanea tarda, etc.)
Classification of HCC according to the TNM system
TNM is an international system for classifying tumors, which is based on determining the size of the primary node (Tumor), the degree of invasion of nearby tissues, the presence of pathologically altered nearby and distant lymph nodes (Nodus) by the tumor, as well as the presence or absence of metastasis to distant organs (bones, liver , lungs, etc.) – Metastasis.
We would like to introduce you to the TNM classification of liver cancer, modified in 1997 by the Union for International Cancer Control (UICC).
| Stage T | Characteristics of the tumor node at this stage |
| T1 | The formation is less than 2 cm in largest size, with no signs of germination into surrounding tissues. |
| T2 | Tumor less than 2 cm in greatest dimension, with vascular invasion. Either more than 2 cm without vascular invasion, or multiple space-occupying lesions no more than 2 cm in diameter in one lobe of the liver, without vascular invasion. |
| T3 | Nodule larger than 2 cm of any size with vascular invasion. |
| T4 | Multiple space-occupying lesions in at least 2 lobes of the liver, or a tumor with invasion into the portal (or hepatic) vein, or tumors with invasion into surrounding tissues. |
| Stage N | Characteristics of lymph nodes at this stage |
| N0 | There are no pathologically changed lymph nodes near the formation (including at the gates of the liver, spleen). |
| N1 | Regional pathologically changed lymph nodes were identified. |
| N2 | Regional and distant (para-aortic, inguinal and other) lymph nodes with signs of tumor invasion were identified. |
| Stage M | Characteristics of secondary lesions |
| M0 | There are no distant metastases (for example, to the lungs). |
| M1 | Disintegrated metastases (at least one) were detected. |
Computed tomography technique for diagnosing liver cancer
The standard for imaging liver cancer with CT is to perform a study with contrast in the arterial and venous phases, since the tumor is often difficult to distinguish with conventional (native, without contrast) scans. For this purpose, non-ionic contrast agents are used - ultravist, iodhexol, omnipaque, etc., injected into the vein of the elbow or another vein using an injector. Typically, to “stain” a tumor, 1.0-1.2 ml of a contrast agent containing 300 mg of iodine per 1 ml is required per 1 kg of patient weight, or 0.8-1.0 ml of a contrast agent containing 370 mg of iodine per 1 ml (for example, Ultravist-370). Thus, a patient weighing 60 kg on average needs to administer about 60 ml of solution. The injection rate is 3-4 ml/sec, provided that the injection occurs through a wide-bore catheter (with a pink or green cannula marking). The use of narrow catheters with yellow markings is unacceptable, since it can damage the vein and provoke extravasation of contrast - infiltration of the subcutaneous tissue and the occurrence of a painful compaction upon injection.
First, a regular spiral scan is performed without contrast, the size, structure, and location of the tumor node are assessed. Then a contrast agent is injected and after 10-20 seconds a second series of scans is performed in a spiral mode - in the arterial phase. After another 30-40 seconds, the scan is repeated again - this is the venous phase. In some cases, it is also useful to perform a delayed scan after 5-10 minutes in order to monitor the “washing out” of the contrast from the tumor tissue. There is also a special research protocol that allows you to evaluate the parameters of blood flow in the formation - CT perfusion. CT with lipiodol has proven itself well, but due to its complexity and invasiveness (contrast must be injected directly into the lymphatic vessel), as well as the possibility of multiple side effects, including vascular fat embolism, this study is not widely used. Liver cancer is also successfully diagnosed using MRI.
Get a CT and MRI of the liver in St. Petersburg
Liver cancer - symptoms and manifestations
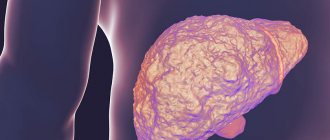
On CT scans, liver cancer has extremely variable appearances and symptoms. CT signs of liver cancer are as follows. Before contrast, one or several lesions in the liver can be identified, which can be isodense (of the same density as the liver parenchyma), hypodense (low density). Dense calcifications, as well as local inclusions of adipose tissue, necrosis, areas of fibrosis, and “tangles” of blood vessels can be found in the lesions.
CT allows you to reliably
diagnose liver cancer: as can be seen on the scan in the arterial-parenchymal phase, the tumor node, which has invasive growth, grows into the right and left lobes of the liver, as well as into the wall of the gallbladder in the fundus and body.
Often HCC, especially small nodes, against the background of fatty involution is not detected on native CT. Small nodes that can be identified are 5-15 mm in diameter. They are clearly defined, separated from surrounding tissues. Sometimes it is possible to identify a denser part of the tumor along the periphery; in the center there is usually a zone of necrosis and decay.
Example of primary multiple liver cancer, image with artificial high contrast (native study).
A larger central node is visible, around which smaller nodes are grouped - intrahepatic metastases. In this case, differential diagnosis with cancer metastases of another location, for example, intestines, is extremely difficult. TNM - T system , such liver cannot be treated , only chemotherapy is indicated for the purpose of temporarily stabilizing the process.
Large HCC nodules have a typical structure due to the alternation of a solid component, cysts, calcifications, areas of necrosis, as well as the presence of arterial vessels. In most cases, such nodes have a capsule. Liver cancer can have expansive growth (pushing aside and squeezing nearby tissues) or infiltrative growth (growing into tissues and destroying them). Often large tumor nodes grow into any branch of the hepatic vein or portal vein. They are also characterized by the presence of small secondary foci in the liver tissue, which represent hematogenous screenings.
Large tumor node.
An example of liver cancer on a CT scan of a liquidator of the Chernobyl accident.
Hyperdense (hypervascular) cancers look like a dense formation of a heterogeneous structure, in the arterial phase they intensify significantly, and the arteries feeding them become clearly visible. Differential diagnosis of such tumors should be carried out with adenomas, hemangiomas, as well as FNH (fibrous nodular hyperplasia). Such cancers tend to rupture, and as a result of the bleeding that occurs, the patient may die.
In the images: an example of hypervascular liver cancer (left), marked with red arrows; on the right, yellow arrows indicate blood along the edge of the liver as a result of HCC rupture.
Differential diagnosis of liver cancer
When analyzing CT data, you should always keep in mind that some liver lesions may resemble liver cancer. An inexperienced doctor may confuse different conditions and make an incorrect diagnosis. The pathology with which it is necessary to differentiate HCC is:
1) Liver hemangioma. To clarify the conclusion, delayed scanning (10-20 minutes after contrast administration) and visualization of vascular lacunae help.
2) Hepatocellular adenoma. Large adenomas may have the same structure as HCC and contain fat inclusions, necrosis, cystic cavities, and calcifications. However, adenomas are characterized by slow growth of the expansive type (without invasion) and the absence of intrahepatic metastases.
3) FNG. With focal nodular hyperplasia, the CT picture may be similar to that of liver cancer. Sometimes it is impossible to distinguish these diseases only from CT examination data - a biopsy is necessary.
4) Metastases. In some cases, the idea of secondary tumors may be suggested by the multiplicity of organ damage and the identification of the primary focus. However, an experienced radiologist with extensive experience in diagnosing liver disease can usually reliably distinguish between primary cancer and secondary metastatic lesions.
Causes of formation of a malignant tumor in the liver
Doctors have not yet compiled an accurate list of possible provocateurs of the disease. Therefore, at present we can name only possible reasons why liver cancer develops. Among them:
- Hereditary predisposition. This is one of the reasons that is one of those that doctors talk about with more or less confidence. A person - both men and women - has a higher risk of developing the disease if one of his close blood relatives has or has had cancer;
- Coincidence. This is a whole list of circumstances that have been “layered” on top of each other. The list includes poor nutrition, bad habits (addiction to alcohol, smoking), chronic liver diseases, living in unfavorable environmental conditions;
- Hard work, including interaction with harmful substances and chemicals. According to medical data, the appearance and growth of tumors is promoted by organic chlorine-containing pesticides, polychlorinated biphenyls, and chlorinated hydrocarbon solvents;
- Severe liver diseases. These include, for example, cirrhosis. With this disease, various complications develop, in particular, hepatorenal syndrome. Such complications can also contribute to the development of cancer;
- Damage by parasites. The presence of some of them in the body significantly increases the risk of disease, weakening the organ, disrupting its functions, contaminating it with waste products;
- Excess iron in the body;
- Products of plant origin grown with the use of growth stimulants and pesticides increase the risk of oncology, including liver cancer.
Even organic compounds consumed in large quantities with food can provoke disease. An example of such compounds are those found in peanuts.
Other malignant neoplasms of the liver
Fibrolamellar cancer (FLC) is usually detected in young men with complete well-being, in a cirrhotic liver, without concomitant hepatitis B or C. Computed tomography for fibrolamellar cancer is performed to assess the resectability of the formation and determine the TNM stage. In a native study, LPR looks like an intrahepatic lesion, large in size - 5 cm or more, and with clear edges. This lesion has a density lower than the density of normal hepatic parenchyma, a lobular structure and - a peculiarity - a central area of fibrosis of a “star-shaped” shape. During the arterial phase, the tumor slightly intensifies in the peripheral parts, while the central part does not change its density.
Cholangiocarcinoma (CAC) is a malignant neoplasm of the bile duct epithelium. With CT, you can see uneven thickening of the wall of the duct against the background of its significant expansion. The formation accumulates contrast and remains hyperdense for a long time - this is a hallmark of cholangiocarcinoma.
Example of cholangiocarcinoma on computed tomography. Arrows highlight areas of the tumor that accumulate contrast agent in the delayed phase.
Hepatoblastoma is most often detected in childhood (3-5 years). On CT examination, it appears as a large hypodense lesion, occupying most of the section area. Approximately 1/5 of all hepatoblastomas are characterized by the presence of multiple foci. The structure of hepatoblastoma is heterogeneous - it may include areas of necrosis, calcifications, and connective tissue. Differential diagnosis is carried out with HCC, LPR, metastases.
Angiosarcoma of the liver is a rare tumor of the walls of the hepatic vessels. Its potential for malignancy is extremely low. It occurs more often in young women under 40 years of age; on CT it appears in the form of multiple cystic foci with clear boundaries, prone to fusion and the formation of polymorphic pseudocysts. It manifests itself as a “target” symptom due to uneven accumulation of contrast in the presence of a zone devoid of blood vessels along the periphery.
Liver lymphoma is extremely rare as a primary tumor; it is usually detected in systemic diseases, for example, lymphogranulomatosis. The CT picture is generally nonspecific - hypodense or isodense nodes of various sizes can be identified, and enlargement of the nearest lymph nodes can also be determined.
Undifferentiated embryonic cell sarcoma of the liver is a malignant neoplasm of sarcomatous cells. It looks like a large cyst, in some cases containing septa. However, despite its low density, it is actually solid, soft tissue. It sharply increases with contrast (in the periphery), differential diagnosis with the cystic variant of HCC is extremely difficult.
How does the disease progress?
At first, a person cannot independently identify a tumor, but if he begins to get very tired, loses appetite, or loses weight, he should immediately consult a doctor who will prescribe an examination. People whose relatives have had cancer or hemochromatosis, when there is excess iron in the body, should undergo regular examination. An examination is even more necessary for severe symptoms that arise in the absence of apparent causes.
First signs
At the initial stage of development, the tumor does not yet affect the blood vessels and is small in size, does not interfere with the liver to perform its functions, and malignant cells do not spread beyond the organ. Stage 1 cancer is usually detected during the diagnosis of other pathologies. The person does not feel pain, but notices:
- constant fatigue;
- drowsiness;
- weakness.
Liver cancer symptoms
Over time, nausea appears. Due to deterioration of digestion, either diarrhea or constipation occurs. There is a feeling of heaviness under the right rib. At this stage, with the right treatment, the disease recedes. But people rarely go to the doctor if they only feel weak.
You can suspect that a tumor is growing in the liver when other signs appear:
- Weight drops sharply.
- Lost appetite.
- The sclera turns yellow.
- Veins protrude through the peritoneum.
- Fluid accumulates in the abdomen.
Even with a small amount of food consumed, there is a feeling of fullness in the stomach. But almost all of these symptoms are similar to those of other diseases.
It is not possible to determine the presence of a small tumor using a blood test; it is detected only by instrumental diagnostic methods.
2nd and 3rd degrees
At the second stage, the neoplasm quickly increases in size, takes on different shapes and grows up to 50 mm. Malignant cells are sent to the vessels, but the tumor does not go beyond the liver and does not metastasize. The first signs become more pronounced, and digestive problems are added to them:
- The stomach is bloated.
- Nausea and vomiting.
- Diarrhea appears.
A person feels discomfort under the right rib and lower back. The pain that initially occurs with exertion intensifies and becomes more frequent. Sometimes the temperature rises a little. In this way, the body reacts to toxic substances released by the tumor. Added to weakness is loss of appetite and loss of body weight. The liver becomes denser and enlarges. The skin turns distinctly yellow.
At the third stage of cancer, several foci are formed where malignant cells accumulate, enter the veins, grow together with other organs, and spread to the lymph nodes. At this stage, specific signs characteristic of liver cancer appear. A person notices them himself. The tumor makes itself felt:
- sudden weight loss;
- swelling of the legs;
- yellowness of the skin;
- nosebleeds;
- exhaustion of the body;
- increasing pain.
The palms take on a reddish tint, and spider veins appear on the body. The temperature rises to 39 degrees, it does not decrease after using medications. The peritoneum fills with fluid, the abdomen greatly enlarges.
The production of hormones by the neoplasm leads to endocrine disorders, which are accompanied by redness of the skin, decreased blood pressure, increased cholesterol levels, and muscle weakness. Lumps form on the liver, which a person can easily palpate on their own.
Terminal stage
At the final stage of its development, the tumor covers most of the organ. Metastases through the bloodstream enter the brain, kidneys, spread to the spine, and affect the heart muscle and ribs. Symptoms of other pathologies are added to the signs of liver destruction.
Human skin loses elasticity, dries out and turns pale. The lower part of the body swells, the abdomen swells, and the bones are clearly visible. Unbearable pain does not leave a person for a minute. Doctors only alleviate his condition with drugs, but there is no point in removing the tumor. The patient dies without living even a year. Some signs remind you of imminent death from cancer, which manifest themselves in the form of:
- refusal to eat;
- heavy breathing;
- foggy consciousness;
- urinary disorders;
- formation of blue spots on the legs.
Liver cancer stage 4
In the last days of life, the patient sleeps almost all the time. He is unable to turn on his other side, eat food, talk or even drink water, and is not interested in anything. Before death, the limbs and fingers become cold.