Basic therapeutic measures
Complex drug treatment of ulcerations that have developed in the small intestine in uncomplicated cases has been poorly developed to date.
Due to the fact that the specialist is not sure that this defect represents tumor ulceration, surgical intervention is always preferable. Since ulcers that develop chronically are not recognized, it is impossible to select targeted drug therapy for them. For such defective ulcerations, urgent surgical treatment is provided. This is due to the fact that their perforation, due to the anatomical structure of the small intestine, occurs very quickly and leads to peritonitis of the abdominal cavity, which can be fatal within a few hours, or at best days.
Surgical intervention consists of suturing the hole at the site of the perforated ulcer, but before this it is excised, since in the absence of this preoperative procedure, secondary perforation of the ulcerated defect is possible.
Intestinal resection is usually not performed for this disease, since such surgical treatment not only complicates the operation, but also worsens further prognosis for the person. This type of surgical intervention is performed only for special indications, which include:
- major changes that have occurred on the wall of this organ of the digestive system;
- developed cicatricial constrictions, provoking the rapid occurrence of fecal obstruction;
- significant bends, also leading to obstruction;
- suspicion of malignancy of pathological defects of the mucous membrane;
- formation of infiltrates.
Only in these cases is treatment carried out by resection. But after this, the patient faces a long recovery period, and possibly lifelong disability. Also, the operation to remove an ulcer that has penetrated (sprouted) into neighboring organs presents great difficulties. This is due to the fact that during this pathological process, interintestinal fistulas and infiltrates are formed.
A poorly understood disease of the small intestine, associated with partial or complete ulceration of its walls, is so dangerous and difficult to diagnose that people at risk for its development should pay more attention to their health. Maintaining a healthy lifestyle, giving up bad habits and regularly visiting a gastroenterologist for diagnostic tests will help avoid the risk of developing pathology or identify it at the very early stage, when the use of drug therapy is still possible and radical surgical intervention is not required
Maintaining a healthy lifestyle, giving up bad habits and regularly visiting a gastroenterologist for diagnostic tests will help to avoid the risk of developing pathology or identify it at the very early stage, when the use of drug therapy is still possible and radical surgical intervention is not required.
Symptoms of ulcers in the intestines
Duodenal ulcer and its possible symptoms
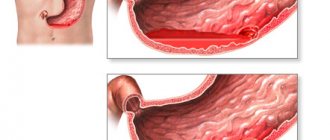
Peptic ulcer occurs as a result of increased acidity of digestive juice or mechanical damage. First, the walls of the organ are irritated, and this, in turn, leads to damage to its mucous surface. Then erosions appear (disturbances of the upper layer), which can develop into lesions penetrating into deeper layers and lead to the formation of intestinal ulcers. Even after it heals, either on its own or with the help of medications, a scar remains on the affected surface.
Symptoms of intestinal ulcers are highly variable (polymorphism). This depends on many factors:
- From the location of ulcerative plaques. The intestine, the longest organ in the human digestive system, consists of the duodenum, small intestine, jejunum, and large intestine.
- Peptic ulcers most often affect the duodenum and large intestine. The duodenum (DU), as the initial link of the entire intestine, brings the acid-base indicator of food to the optimal level for subsequent stages of digestion. It is more susceptible than other parts of the esophagus to inflammation and, as a result, the formation of ulcers. Since food and liquid, semi-processed in the stomach, are the first to enter it from the pylorus of the stomach.
- The small intestine is responsible for the absorption of nutrients into the human body. It produces enzymes that break down digestive products into separate fragments. An ulcer of the small intestine is formed due to inflammation of the mucous membranes under the influence of an acidic environment.
- The colon, the final part of the digestive tract, is responsible for absorbing water from processed food back into the bloodstream, producing vitamins, and processing fiber. In it, the formation of feces occurs and, in a healthy state of the body, their timely release.
- II. On the number and depth of ulcerative plaques. The intestinal walls consist of the outer (serous) lining of the intestines, the muscular layer, the submucosa and the inner, mucous membrane covered with epithelium. If the epithelial layer and submucous membrane are damaged, single or multiple ulcers may occur in the intestine, with different areas and depths of damage.
- III. Depending on the severity of the disease. The clinical manifestations of ulcerative symptoms may alternate. Flowing from the stage of exacerbation into the period of remission. The acute period, as a rule, occurs in the autumn and winter.
Also, the manifestation of symptoms of intestinal ulcers is influenced by indicators such as the presence of concomitant diseases in the anamnesis, gender, age and heredity.
A peptic ulcer can develop in several parts of the intestine at once if it is provoked by:
- Hereditary predisposition or congenital pathology (digestive enzyme deficiency);
- Infection with microbial toxins as a result of food or drug poisoning, inflammatory processes of the intestinal walls;
- If intestinal activity is disrupted due to diseases of the endocrine and nervous systems;
- Infection with parasites (N.P., worms);
- Adhesive processes;
- Crohn's disease, accompanied by chronic inflammation of the intestines.
The symptoms of an ulcer can be divided into:
- General, characteristic of all parts of the intestine.
- Specific, depending on the location of the ulceration.
Common symptoms include:
Specific symptoms are determined by the location of the ulcer. And here we can already talk about the signs of an intestinal ulcer (the same symptoms may relate to different diseases, but the signs of the disease objectively indicate precisely this disease).
Symptoms
The listed diseases have specific symptoms from the affected intestines and the body as a whole. They reach their greatest severity during periods of exacerbation, which disrupts a person’s quality of life. Duodenal ulcer, nonspecific ulcerative colitis and Crohn's disease are characterized by a chronic course with relapses as a result of exposure to provoking factors.
Intestinal manifestations
Characteristic signs of exacerbation of the disease:
- periodic or constant acute pain in the epigastric region of the abdomen;
- nausea, often leading to vomiting;
- increased pain on an empty stomach, at night;
- frequent belching with a rotten smell;
- flatulence;
- loss of appetite.
The intensity of pain depends on the duration of the process, the number of ulcers and the person’s pain threshold. The nature of nutrition also plays a certain role.
Crohn's disease is a systemic pathology in which segmental damage most often occurs to the small intestine with the formation of erosions, ulcers of various sizes and stenoses.
Symptoms of the disease:
- cutting or aching pain in the abdominal area that does not have a clear localization;
- flatulence after eating;
- loose stools up to 4-10 times a day;
- the appearance of blood impurities in the stool.
The severity of the described signs depends on the degree of activity of the inflammatory process in the gastrointestinal tract. The most severe disease occurs with combined damage to the stomach, small and large intestine.
With nonspecific ulcerative colitis, chronic inflammation of the intestine is determined, in which ulcers, microabscesses and polypous growths appear over time. Local signs of colitis:
- stool with pathological impurities (blood, mucus and sometimes pus);
- diarrhea up to 5-12 times a day;
- cutting pain in the lower abdomen;
- constant flatulence.
Be sure to read: Bismuth preparations: a list of medications and their use for the stomach.
Usually the disease is severe with a clear clinical picture. UC is more common in men aged 20 to 60 years.
Extraintestinal manifestations
In addition to local intestinal symptoms, ulcers may be accompanied by pathological changes in the skin, eyes, and joints.
A duodenal ulcer is characterized by:
- “jams” in the corners of the mouth, or angular stomatitis;
- desquamative glossitis (deep folds on the tongue, its redness);
- increased fragility of hair and nails.
In UC or Crohn's disease, extraintestinal symptoms are systemic and more severe:
- increased body temperature, chills;
- general weakness, poor appetite;
- progressive weight loss;
- inflammation of the membranes of the eye (conjunctivitis, uveitis, iridocyclitis);
- muscle and joint pain;
- skin rashes of various types (ring-shaped erythema, etc.);
- damage to small vessels (vasculitis).
Manifestations of colonic lesions
Reactive pancreatitis symptoms and treatment in adults
A colon ulcer has the following manifestations:
- Accompanied by acute pain of varying degrees of intensity during bowel movements.
- If pathogenic microorganisms enter the foci of ulcerative lesions, they cause infection of open wounds on the organ mucosa, which causes an abscess and the formation of purulent exudate.
- Chronic constipation occurs frequently.
- In addition to intense pain, the ulcers bleed and bloody mucus is released from the anus. When passing stool, the stool contains blood clots. If left untreated, minor bleeding causes the development of anemia. Severe blood loss can be fatal.
- When the rectum is affected, severe itching, irritation of the mucous membrane, oozing, and spastic contractions are observed. The development of polyps, anal fissures, and inflammation of hemorrhoids is possible. Ulcers bleed and often become infected. There is a risk of developing neoplasms of benign and malignant origin. A person feels the urge to defecate. This process is called tenesmus. False sensations may be accompanied by severe pain.
An early symptom of the lesion is causeless diarrhea. Loose stools may contain bloody clots, mucous discharge, and copious foam. With the development of the pathological process, body temperature does not increase. In the first stages, the disease is asymptomatic.
Differential diagnosis
For different diseases of the colon, the symptoms are similar to each other; clear specific signs rarely occur
Therefore, differential diagnosis is important. It includes a number of laboratory and instrumental studies
The gastroenterologist compares the data obtained with specific symptoms of intestinal diseases.
Diagnostic procedures
To make a correct diagnosis, a gastroenterologist collects a detailed medical history of the patient and analyzes the patient’s complaints. Then he conducts a physical examination and anoscopy. During the procedure, the doctor assesses the person’s general condition. Using palpation, the degree of damage to the rectum is checked. If there are no ulcers on its mucosa, to exclude pathologies in the cecum and colon, the doctor prescribes a number of additional studies:
- colonoscopy;
- irrigoscopy;
- sigmoidoscopy.
If copious mucous, serous, purulent or bloody discharge comes out of the anus, it is taken for laboratory analysis. This is necessary to exclude or confirm the presence of a secondary infection, and to check the likelihood of complications.
Diet therapy
Hirschsprung's disease in adults: symptoms and treatment for the syndrome
Proper fractional balanced nutrition plays a decisive role in the treatment of gastrointestinal pathology
It is important to put the secretion of the stomach in order, to completely restore it, since the activity of the duodenum depends on this
The patient must follow a strict diet recommended for the ulcer, consume foods that are rich in minerals and vitamins, and eliminate all irritants. You should eat at least five to six times a day.
The therapeutic diet during the period of exacerbation of intestinal ulcers prohibits such foods as:
- alcohol;
- carbonated drinks;
- coffee, strong tea;
- rich broths, borscht;
- fried, spicy, salty and hot, smoked products;
- berries and fruits with hard skin;
- sweets, baked goods and fresh baked goods;
- peas, beans, corn and asparagus.
The diet for intestinal ulcers recommends creating a diet based on the following products:
- lean meat - turkey, chicken and veal;
- milk porridge;
- honey, jam, marshmallows, jelly and jelly;
- biscuits;
- stale bread, crackers;
- still mineral water;
- tea with milk.
The ideal temperature of the finished dish should be no less and no more than thirty degrees. It is advisable to add butter and olive oil to porridges and soups during an exacerbation of an ulcer. Diet therapy during an ulcer involves consuming 3 thousand kilocalories per day. Thanks to a balanced and nutritious diet, the healing process and scarring of the ulcer are significantly accelerated.
The noted ulcerative pathology of the gastrointestinal tract is amenable to conservative treatment. It is necessary to recognize the symptoms of the disease in time. Thanks to a healthy lifestyle, a balanced diet, and medications, the patient can get rid of the unpleasant symptoms of an ulcer.
https://youtube.com/watch?v=w8RxI47fXwU
Few people are not familiar with heaviness in the stomach after eating.
And most people do not pay attention to such sensations, believing that this is a temporary consequence of overeating or poor nutrition.
However, if such sensations begin to visit you more and more often, and stomach pain is added to them, then you urgently need to take care of yourself. After all, this may indicate an incipient ulcer.
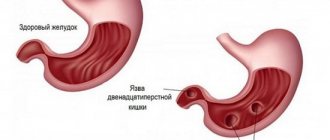
A gastric ulcer is a disease that is manifested by the formation of chronic ulcerative defects in the gastroduodenal zone (in the stomach and duodenum). Ulcers can be either single or multiple (more than three).
The main difference between a chronic gastric ulcer and erosion is deeper penetration into the stomach wall, penetration not only into the cells of the mucous membrane, but also into the submucosal layers, healing of the defect with the formation of a scar.
As you know, when treating a stomach ulcer, it is important to eliminate the following symptoms - severe pain in the stomach, frequent vomiting, heartburn, “hunger pains” that stop after eating. Exacerbation of the disease may be accompanied by unbearable night pain
Therefore, during drug treatment, an integrated approach must be used with mandatory consideration of the individual characteristics of the process to effectively eliminate the causes of the disease.
Treatment of stomach ulcers with folk remedies
Important!
Before using folk remedies for stomach ulcers, be sure to consult your doctor! Read also Osteochondrosis - symptoms, causes, types and treatment of osteochondrosis
Potato juice. Grate the washed and peeled potatoes, squeeze the juice from the puree through cheesecloth. You need to take 20 g of potato juice, 30 minutes before meals, 3 times a day, for 7 days. In the second week, the amount of juice per dose should be 40 g, in the third week – 60 g, in the fourth week – 100 g. The course of treatment is 1 month. The effectiveness of the product will be best if no more than 10 minutes pass from squeezing the juice to drinking it. At the same time, traditional healers prohibit the use of juice from old potatoes in treatment, for example, in winter.
A beneficial and healing effect on the body has also been noticed if potato juice is diluted with carrot juice in a 50/50 ratio.
St. John's wort. Pour 15 g of dried St. John's wort herb into 200 g of boiling water, and set the vessel aside overnight to infuse. In the morning, strain, add a little boiling water to make 200 g of infusion, and take this infusion for ulcers warm, 50 ml, 3-4 times a day, 30 minutes before meals. The course of treatment is 14 days. If symptoms from the disease remain, you need to take a week break and repeat the course for 14 days.
Please note, dear readers, that St. John's wort can cause an allergic reaction, so start drinking it with a small sip, and if there is a reaction, then do not use this remedy.
Propolis. Add 1 liter of fresh cow's milk and 50 g of propolis to the pan, mix them thoroughly and place on the stove to heat and completely dissolve the propolis in the milk. You need to take this remedy for ulcers in an amount of 100 g, 40 minutes before meals, 3-3 times a day. The course of treatment is 30 days. If the signs of the disease have not disappeared, the course is extended.
Please note that propolis is a bee product and may therefore cause an allergic reaction. This drug is also contraindicated in children under 3 years of age and in case of liver failure in adults.
Honey with butter and walnuts. Place 300 g of flower honey, walnuts and butter in an enamel pan. Next, place the pan in the oven for 20 minutes at 100 °C, after which remove the product and mix well. You need to take this honey mixture 1 tbsp. spoon 3 times a day, 30 minutes before meals, without washing down with water.
Calendula. For treatment, we will need calendula oil, for the preparation of which we need to pour 30 g of calendula flowers into 100 g of vegetable oil (preferably olive oil), mix and place in a water bath, heat to 70-80 ° C and simmer the product for about 2 hours. Next, the product is set aside for a day to infuse, filter and take 5 g 30 minutes before meals for 2 weeks.
This remedy is contraindicated for ulcers in the acute stage, pregnant women, breastfeeding, children under 12 years of age, as well as for cardiovascular diseases.
Plantain. 1 teaspoon of plantain leaves is poured into 200 g of boiling water, cover the glasses with a lid and set aside for 20-30 minutes to infuse. Afterwards, the plantain infusion is drunk whole, 30 minutes before meals, 2-3 times a day.
Complications of duodenal ulcer
Bleeding is the most dangerous complication of a duodenal ulcer.
If the ulcer “corrodes” the vessel, bleeding begins. With slight blood loss, the stool becomes black. As the stool intensifies, it becomes black, pasty (melena) or clearly mixed with blood. Chronic blood loss causes anemia, which is manifested by dizziness, weakness, pallor, brittle hair and nails. Acute heavy blood loss causes severe weakness up to loss of consciousness, dizziness, and “spots” before the eyes. This condition requires immediate hospitalization in a surgical hospital - the mortality rate for ulcerative bleeding reaches 15%.
Another dangerous complication is perforation of the ulcer. The intestinal wall “breaks through” and the contents spill into the abdominal cavity, causing peritonitis. A sharp, “dagger” pain occurs in the abdomen, the abdominal wall becomes hard, and the patient usually lies or sits with his legs pressed to his stomach. Perforation of an ulcer requires urgent surgery: the sooner the patient gets to the surgical table, the greater his chances of recovery. The average mortality rate for perforated ulcers is 8.9%.
If the ulcer is located on the wall of the stomach adjacent to the liver or pancreas, penetration may develop. As the ulcer deepens, it “grows” into the neighboring organ, fusing the intestinal wall with it. Pain during penetration becomes constant, and the symptoms of an ulcer are accompanied by signs of damage to the organ into which penetration occurred.
After the ulcer heals, a scar remains in its place. If there are many such scars, cicatricial stenosis of the duodenum may develop. In the initial stages, it manifests itself as a feeling of heaviness and fullness in the stomach immediately after eating, nausea, and vomiting may occur, which brings relief. As the condition worsens, vomiting becomes frequent, and food eaten the day before or even several days ago can be found in the vomit; the patient loses weight, and signs of exhaustion appear.
Malignancy of a duodenal ulcer is extremely rare; it is usually a diagnostic error when the ulcerative form of cancer is mistaken for a regular peptic ulcer.
Signs and symptoms
The main symptom is regular, frequent and severe abdominal pain. Usually, you feel worse after eating. The stomach may hurt for a long time, up to several hours, during the day or at night. Other signs include general digestive disorders, nausea, belching with a sour smell, and vomiting.
Pain appears only during exacerbations; it is absent during periods of remission. Remission may last for several months or years. The more attentive a person is to nutrition and the recommendations of the attending physician, the lower the risk of exacerbation of the ulcer.
The first signs at an early stage
At an early stage, the disease may manifest as discomfort and moderate abdominal pain. They appear after eating, can gradually weaken or intensify, leading to vomiting, after which relief comes.
The disease at this stage is not always accompanied by pain. It can manifest itself as discomfort, general digestive problems, a feeling of heaviness in the stomach, rare heartburn, and belching. If an ulcer develops due to the use of painkillers, they can also dull the pain associated with it. There are cases when at the initial stage of a peptic ulcer there are no manifestations at all.
How does a stomach ulcer manifest in an adult?
Adults may experience the following symptoms:
- some time after eating, your stomach begins to hurt;
- there is regular heartburn and belching with a sour smell;
- nausea, vomiting of partially digested food;
- discomfort, bloating, heaviness;
- decreased appetite, rapid satiety;
- stool disorders and flatulence.
Appetite decreases, nutrition becomes insufficient, food is less digestible. Because of this, your overall health deteriorates. General malaise, insomnia due to nighttime abdominal pain, weakness, and fatigue may appear.
What are the clinical symptoms of a stomach ulcer?
The clinical picture depends on the location of the ulcer, the general health of the person and some other factors. Most often, the disease manifests itself as pain in the epigastric region (just below the sternum in the midline). The pain is similar to a feeling of hunger. They can be sharp and intense. Eating can either strengthen or weaken them. It depends on the location of the ulcer:
- if the cardial or subcardial part of the stomach is affected, the stomach hurts immediately after eating;
- if the body of the stomach is affected, 30-60 minutes pass between eating and the onset of pain;
- late pain is typical for damage to the mucous membrane of the duodenal ampulla and pyloric canal. The stomach begins to hurt 2-3 hours after eating, on an empty stomach or at night.
Peptic ulcer disease occurs as a chronic disease. Its exacerbations can last from 3 to 8 weeks. The periods of remission between them are several weeks, months or years. This largely depends on the prevention of exacerbations: diet and diet, lifestyle, and other factors. Often exacerbations are seasonal (appear in spring or autumn) and begin due to provoking factors (if a person starts taking painkillers or drinking alcohol, if he is stressed, overexerted, if his health condition worsens).
When to see a doctor?
Call your doctor if you have serious signs or symptoms of a stomach ulcer:
- burning pain in the stomach;
- unexplained weight loss;
- vomiting blood;
- dark blood in the stool;
- sudden sharp pain in the abdomen that gets worse;
- difficulty breathing, feeling of weakness.
Also see your doctor if over-the-counter antacids and acid blockers relieve your pain but the pain returns.
Treatment of the disease
Let's consider what drugs are used to treat this dangerous disease during an exacerbation period.
1. Antisecretory agents inhibit gastric secretion, thereby reducing the aggression of gastric juice. These include proton pump inhibitors (Nexium, Pariet, Omez and Omeprazole), as well as anticholinergics (Gastrocepin) and histamine receptor blockers (Ranitidine, Famotidine, Cemetidine).
2. Products containing bismuth are also used to combat this disease in the presence of Helicobacter pylori. These medications inhibit the activity of bacteria and create a film on the surface that protects against damage from gastric juice. This group includes the following drugs: De-nol and Vikair.
3. Medicines that improve duodenal motility, that is, prokinetics, are also prescribed during the period of exacerbation of the disease. These include medications: Motilium, Cerucal, Trimetad.
4. To suppress Helicobacter pylori, doctors usually prescribe prokinetics and antibacterial agents: Tetracycline, Metronidazole, Clarithromycin and Amoxicillin.
5. Duodenal ulcers cannot be treated without the use of antacid drugs, such as Maalox, Almagel or Phosphalugel. Their exposure is necessary to neutralize the aggressive effects of hydrochloric acid. In addition, these products have an astringent and adsorbing effect.
6. Doctors also have gastroprotective agents in their arsenal, for example, the medication Venter, which, when entering the body, coats the mucous membrane, largely protecting it from the effects of digestive enzymes and hydrochloric acid.
7. Among other drugs for the treatment of duodenal ulcers, one should highlight the frequently used antispasmodics (Drotaverine), analgesics (Baralgin), as well as medications designed to improve the nutrition of the intestinal mucosa. These include Actovegin, as well as B vitamins. Good health to you!
Modern pharmacotherapy for peptic ulcer disease includes more than 1000 different drugs and their combinations. The concept of therapy involves their use as part of various treatment regimens, depending on the course and severity of the disease, the causes of its occurrence, as well as the characteristics of the patient’s body, his age and the presence of concomitant diseases. Therefore, treatment should only be prescribed by a doctor
An important feature of modern therapy for peptic ulcer disease is that there is practically no difference in the treatment of duodenal ulcer (DU) and gastric ulcer (GUD).
Principles of treatment of colon ulcers
Treatment tactics depend on the cause, severity of the disease and the presence of complications.
Treatment for colon ulcers includes:
- surgical methods;
- medications;
- a carefully selected diet.
Traditional medicine can be used with the permission of the attending physician and under his supervision.
Surgical treatment
Indications for surgical treatment of colon ulcers are the ineffectiveness of conservative methods and the development of complications - bleeding, perforation, intussusception and others.
Types of operations
The type and technique of surgical intervention depend on the size and location of the ulcer, as well as the presence of complications.
To eliminate an ulcer:
- Endoscopic operations - a flexible optical part of the equipment and microsurgical manipulators are inserted through the anus.
- Laparoscopic minimally invasive interventions - instruments are inserted through small punctures in the anterior abdominal wall.
- Open, extensive interventions - classic operations with dissection of the anterior wall of the abdominal cavity.
In the absence of complications, surgeons tend to perform minimally invasive operations. They are the least traumatic, have minimal blood loss and allow you to heal colon ulcers in a short time.
Recovery period
After the operation, the patient spends in the hospital from 2 to 10 days (depending on the volume and method of intervention). The surgeon prescribes painkillers.
Meals should be fractional and sparing. Patients are advised to get out of bed as early as possible and move more (walk on a straight, level surface). Physical activity is prohibited for 1.5-2 months.
Possible consequences and prognosis for life
If the operation is performed in a timely and correct manner, the patient complies with all the doctor’s instructions, the postoperative prognosis is usually favorable.
However, there is always a risk of developing:
- bleeding;
- wound infection;
- cicatricial narrowing of the intestinal lumen;
- adhesive disease.
The risk of these complications increases if the patient has previously undergone intestinal surgery.
Drug therapy
The goals of drug therapy are to relieve inflammation, restore motility and normalize intestinal microflora. Main groups of drugs:
- antibacterial drugs selected taking into account the sensitivity of pathogenic flora;
- probiotics – “Maxilak”, “Normobakt”, etc.;
- antidiarrheal drugs - Smecta, Loperamide, Imodium;
- antispasmodics - “No-shpa”, “Papaverine”, “Platifillin”;
- laxatives - Bisacodyl, Duphalac, Glycelax.
Medications are prescribed in the form of tablets for oral administration and rectal suppositories. To speed up the healing process, Sucralfate is used in the form of therapeutic enemas.
Diet
Along with medications, proper nutrition plays an important role in the treatment of colon ulcers. Fried, spicy and smoked foods, coarse fiber, coffee, carbonated and alcoholic drinks are excluded from the diet.
Products are served boiled or baked and eaten warm. Slimy soups and porridges, jelly, and vegetable purees are useful.
Treatment with folk remedies
Treatment of colon ulcers with tablets and suppositories can be combined with folk recipes. This can only be done under the supervision of the attending physician.
You can treat the symptoms of colon ulcers at home with herbal remedies:
- Wound healing - yarrow, plantain, tansy.
- Eliminates pain and inflammation - chamomile, oregano, galangal, etc.
- Laxatives - dill, flaxseed, senna, buckthorn.
Herbal decoctions and infusions are taken orally or administered as enemas.
Diagnostics
Diagnosis of pathology can be carried out by a therapist, gastroenterologist or surgeon.
Data collection and inspection
In the first stages, it is important to interview the patient, during which the doctor finds out the complaints, their nature, duration and frequency. It is mandatory to establish the onset of the disease, find out the hereditary history, and the plan for previous treatment.
A detailed examination will help the doctor detect inflammatory lesions of the eyes, skin or tongue, and joint contractures as a result of long-term arthritis. Palpation of the abdomen is carried out to determine the area of pain, pathological changes in the shape and size of the intestine, and bloating.
Instrumental studies
Invasive techniques allow a more detailed and “personal” examination of the intestinal mucosa, detect the nature and number of defects on it, perform a biopsy and even minor operations if necessary.
To establish a diagnosis, the following types of instrumental diagnostics are prescribed:
- Fibrogastroduodenoscopy (with/without urease test). This is an examination of the upper segment of the gastrointestinal tract using an endoscope (from the esophagus to the duodenum). It is the “gold” standard for diagnosing peptic ulcer disease.
- Fibercolonoscopy. The rectum and colon are examined; It is possible to perform a biopsy and minor surgical interventions (stop bleeding, remove polyps).
- Contrast irrigography. X-ray examination of the intestine using a contrast agent and taking a series of images.
Laboratory research
Laboratory tests include clinical and biochemical blood tests (decrease in hemoglobin and albumin levels, appearance of C-reactive protein and fibrinogen). In some cases, they resort to immunological analysis, which detects the presence and amount of plasma antibodies.
A coprocytogram and bacteriological examination of stool can show the presence of undigested particles, leukocytes and a high concentration of pathogenic microbes. Equally important is a stool test for occult blood.
The treatment is complex. Therapy should include dietary advice, medications and, if necessary, surgery.
It is important to maintain a balanced diet both during and outside of exacerbations. You should avoid overeating, eating dry or on the go, excessive consumption of carbonated drinks, fast food
Food should be prepared using gentle methods (baking, boiling) and served at the optimal temperature (20-40 °C).
- slimy porridges (rice, oatmeal);
- vermicelli;
- soft-boiled eggs;
- non-acidic juices;
- low-fat cottage cheese, milk;
- lean fish, meat (hake, pollock, chicken, rabbit);
- fruit compotes;
- boiled or baked vegetables;
- cracker.
- spices, hot sauces;
- legumes;
- canned food, semi-finished products;
- alcohol, coffee, sweet carbonated water;
- pearl barley, wheat porridge;
- fatty meat, fish;
- crackers, chips;
- fresh bakery.
The presence of frequent diarrhea implies an increase in daily calorie intake and the amount of fluid consumed. This will avoid dehydration and sudden weight loss.
Medications that can be used include:
- Antibiotics. Designed to fight infection (penicillins, cephalosporins, fluoroquinolones).
- Antisecretory, antacid drugs. Reduce acidity, protect the walls of the gastrointestinal tract (omeprazole, rabeprazole, Maalox, Almagel).
- Corticosteroids. They have anti-inflammatory activity and inhibit autoimmune processes (Prednisolone, Budesonide).
- Aminosalicylates/cytostatics. Prevents the progression of autoimmune inflammation in the intestines (Sulfasalazine/Methotrexate).
In addition, symptomatic therapy is prescribed: painkillers, vitamins.
Surgical interventions are indicated in case of steady progression of the disease, development of complications, and ineffectiveness of drug therapy. Statistics indicate a high relapse rate (up to 45%) 3-5-7 years after the intervention. Surgeries for duodenal ulcers are most effective.
Types of operations
- Necrectomy. Excision of ulcerative defects.
- Vessel ligation. Used to stop bleeding.
- Bowel resection with/without anastomosis. Removal of the most altered segment of the intestine with or without the formation of an anastomosis with another part of the gastrointestinal tract.
Recovery period
In most cases, the recovery period takes from 2-4 weeks to several months, which depends on the degree of intestinal damage and the timeliness of therapy. In some cases, remission is achieved for years or the disease leads to disability.
Prevention of stomach ulcers
Prevention of gastric ulcer includes the following recommendations:
- Follow the rules of personal hygiene;
— Use well-washed cutlery;
— If there is a person with an ulcer in the family, give him a separate set of cutlery for use for a while;
— Do not ignore chronic diseases of the gastrointestinal tract;
- Avoid stress;
— Strengthen your body’s immune system, which is your defense against various infections;
— Follow the correct diet - small meals, chew food thoroughly, do not eat very hot or cold food;
— Try to give preference to foods rich in vitamins and macro-microelements, minimize spicy, fried and smoked foods in food;
- Move more;
— Use medications only after consulting a doctor;
— Don’t forget to follow the work/rest/sleep schedule; you need to sleep at least 8 hours a day;
— Stop drinking alcohol and smoking.
Outpatient examination and treatment of illness
A gastroenterologist will tell you how to treat an ulcer with drugs and procedures
When examining a patient, the doctor pays attention to the symptoms and signs of the disease and sends for tests:
- mucous membrane for the presence of infections;
- blood for antibodies;
- urine for the presence of bacteria in the body;
- stool for antigens (bacteria that cause ulcers).
The main diagnostic information is obtained through a full examination using special equipment: x-ray and endoscopic examination, which will 100% confirm or refute the diagnosis. The motor and evacuation activity of the internal organs will be visible.
https://youtube.com/watch?v=PPu4rXaOwV0
Gastroscopy is performed on an empty stomach. A tube with an optical device is inserted through the mouth into the stomach cavity. The gastroenterologist examines the esophagus, stomach and intestines. If necessary, a biopsy has to be done to examine the mucous membrane in the laboratory. This is an unpleasant but informative procedure. X-rays are rarely performed if a duodenal ulcer is suspected. An ultrasound examination of the internal organs of the abdomen is prescribed to clarify the diagnosis if the picture from previous procedures is unclear.
After determining the type of ulcer and location, drug treatment is prescribed: a number of drugs and procedures necessary to eliminate the pathology. Bactericidal, pain relievers, antacids and absorbents are the main components of an ulcer first aid kit. Physiotherapy is prescribed.
An individual diet must be selected and prescribed, depending on the type of ulcer. It is necessary to follow the recommendations regularly to maintain human health.
You will have to go through a surgical cure if the ulcer has worsened and caused peritonitis, perforation or penetration, or transformation into cancer. A different course of recovery and struggle is already being used here.
After treatment, you will have to take tests again to make sure that the pathology has disappeared. Monitor your body’s behavior and don’t neglect going to the doctor. Self-medication is dangerous; you should always consult a doctor before taking medications. This will prevent an unpleasant illness or save a life.
An intestinal ulcer is a gastroenterological disease that leads to disruption of the integrity of the intestinal walls, which can subsequently lead to tissue necrosis. In this case, even death cannot be ruled out.
An intestinal ulcer is dangerous because it can be asymptomatic for a long time, so in most cases it is diagnosed in a chronic form. The course of the pathological process is characterized by periods of remissions and exacerbations.
An intestinal ulcer can be caused by certain gastroenterological diseases, long-term use of medications, poor diet, and exposure to the bacterium Helicobacter pylori. Only a doctor can accurately determine the cause of such a disease by taking all necessary measures.
The clinical picture of this pathology is in many ways similar to inflammatory bowel disease, and the initial course of the disease resembles a common indigestion. In fact, it is precisely this nature of the manifestation of symptoms that leads to the fact that patients do not seek medical help in a timely manner.
For diagnosis, a physical examination of the patient, laboratory and instrumental research methods are performed. Treatment tactics will depend on the clinical and morphological signs of this pathological process. If the disease is diagnosed at an early stage of development, then it is quite possible that conservative measures will be sufficient to eliminate the disease. In all other cases, surgical intervention will be required.
There is no clear prognosis in this case, since everything will depend on whether treatment was started in a timely manner and the form of the disease itself.
Symptoms of stomach and duodenal ulcers
Signs of gastric and duodenal ulcers and their interpretation include the following.
First of all, these are pain attacks that vary in intensity and are often associated with food intake.
It is important to note how long it takes for discomfort to begin after eating and what the location of the pain is. This can help in diagnosing the disease
If pain occurs in the first 2 hours after eating, then it is called early pain. Then their intensity decreases or they disappear completely.
Late pain is called pain that appears after a period of time of more than 2 hours.
Hungry (or fasting) pain is considered to develop 6-7 hours after eating, and night pain is felt in the second half of the night.
Symptoms of stomach and duodenal ulcers can vary and appear in different forms. Separately, it should be recalled that there is also a painless form of ulcerative lesions.
It is typical for older people, diabetics, or with long-term use of NSAIDs (non-steroidal anti-inflammatory drugs). By the way, it is precisely because of drug abuse that stomach and duodenal ulcers occur.
As a result of stomach and duodenal ulcers, a person experiences a variety of unpleasant sensations, including pain. By nature, the following types are distinguished: acute cramping, paroxysmal, cutting, piercing, aching, drilling, squeezing, dull, burning.
A painful attack can last from 1 to 2 hours. The intensity can vary, ranging from barely perceptible signs to very pronounced ones.
In addition, it is observed:
- Heartburn is a sensation of something sharp or hot behind the breastbone, which is associated with increased acidity in the stomach.
- Bloating (flatulence).
- Nausea, sometimes vomiting of food eaten.
- Heaviness in the epigastric region after eating.
- Belching with an unpleasant odor.
- Loss of appetite.
- Losing weight. Perhaps due to a psychological barrier: a person does not want to eat, remembering a painful attack (sitophobia).
- Change in stool: constipation.
Another indirect symptom is the seasonality of relapses.
Most often, peptic ulcers of the stomach and duodenum appear in spring and autumn.
Exacerbation of gastric ulcer increases the above symptoms.
Types of stomach ulcers
Gastric ulcers are classified as follows:
According to clinical manifestations:
- Acute stomach ulcer;
- Chronic stomach ulcer.
By localization:
- Cardiac ulcer of the stomach;
- Subcardial department;
- Antrum;
- Pyloric canal;
- Body of the stomach, anterior and posterior walls, lesser and greater curvature.
By ulcer size:
- Small - less than 5 mm;
- Average - 5-10 mm;
- Large - 11-30 mm;
- Giant - more than 30 mm.
By stage:
- Active stage;
- Scarring stage;
- “Red” scar stage;
- “White” scar stage;
- Stage of prolonged absence of scarring.
By phase:
1. Exacerbation (relapse); 2. Faded exacerbation (incomplete remission); 3. Remission.
With the flow:
1. Latent flow; 2. Mild, rarely recurrent course; 3. Moderate ulcer, recurrent 1-2 times a year; 4. Severe course - the disease is accompanied by complications and frequent relapses (3 or more times a year).
Diagnosis of stomach ulcers
Diagnosis of stomach ulcers includes the following examination methods:
- Taking anamnesis;
- General blood analysis;
- General urine analysis;
- General stool analysis;
- Fibroesophagogastroduodenoscopy (FEGDS);
- Ultrasound of the gallbladder, pancreas and liver;
- X-ray using contrast agent;
- Computed tomography (CT);
- Monitoring the pH of gastric juice throughout the day;
- Tests for the presence of the bacterium Helicobacter pylori in the body;
- Biopsy.
Read also Obesity - degrees, causes, diet and treatment of obesity