Congestive gastropathy: what is it? How to treat?
All results of the inflammatory process in the stomach can be divided into two categories. These are gastritis and gastropathy familiar to everyone. With gastritis, the gastric mucosa is affected; erosions and minor ulcerations are visible on it. In this case, a person experiences discomfort after eating too spicy, hot or cold food. Everyone has encountered it at least once in their life, especially when they were young and lived separately from their parents.
With gastropathy, no significant changes occur in the gastric mucosa. Small areas of inflammation are visible on it - and that’s all. However, this prosperity is deceptive. There is still damage at the cellular level. Epithelial cells are destroyed, and their recovery is slow compared to normal.
Congestive gastropathy is a disorder of gastric motility and its passage through the digestive canal up to the small intestine.
Treatment of pathology includes drug therapy, taking vitamins, a certain diet and giving up bad habits. It is also recommended to lead a healthy lifestyle, including walks in the fresh air.
Why does the stomach stagnate? Congestive gastropathy - symptoms, treatment
Portal, or congestive gastropathy, is a condition caused by stagnation in the stomach. The clinical condition is very common in liver cirrhosis. And although liver damage is the main causative agent of portal gastropathy, it is not the only cause of the disease.
Gastric congestion can also occur as a result of bacterial infections, long-term use of certain medications, or bad habits such as alcohol or smoking.
The disease must be treated, since therapeutic actions not provided in time can lead to life-threatening bleeding.
Painful signs of congestive gastropathy
How does portal (congestive) gastropathy develop?
This is a disease in which inflammation of the gastric mucosa does not occur, but the epithelial cells of its walls are still damaged. In addition, the development of congestive gastropathy is facilitated by a lack of some enzymes.
Stagnation in the stomach leads to disruption of the microcirculation of the gastrointestinal tract, resulting in the so-called collateral circulation, which damages the walls of the stomach.
Complications of congestive gastropathy are hidden bleeding and severe anemia - a life-threatening condition.
Risk factors for congestive gastropathy
The etiology of this disease has not been fully explained, but liver cirrhosis to be a causative factor in its development. Organ damage leads to portal vein occlusion and hemorrhage. The risk of getting sick increases with age.
A cause-and-effect factor for congestive gastropathy is also an unhealthy lifestyle, for example, a person’s addiction to alcohol and smoking. In addition, certain medications can cause portal infections.
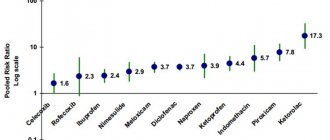
Long-term use of analgesics, anti-inflammatory and antipyretic drugs damages the mucous membrane of the stomach and liver, which is unable to get rid of excess toxins.
People with stomach ulcers, reflux disease, and chronic bacterial infections, especially Helicobacter pylori, are also vulnerable to gastric congestion.
Diet for congestive gastropathy
Types of portal gastropathy
Depending on the course of the disease, portal cholestasis is divided into two types:
- Mild degree - on the endoscopic image of the stomach, a mosaic of the mucous membrane is noticeable, but it is not yet very pronounced. The probability of bleeding in the gastrointestinal tract is 3-30%.
- Severe degree - membranous mosaic of submucosal hemorrhage of the stomach is very noticeable. The risk of bleeding in the gastrointestinal tract is 40-60%.
The diagnosis of congestive gastropathy is complicated by the fact that at first the disease does not manifest itself with any characteristic symptomatic signs.
Symptoms of portal (congestive) gastropathy
The onset of the disease is completely asymptomatic. Only over time does a number of signs of dyspeptic disorders appear, for example:
- progressive general weakness;
- abdominal pain of varying intensity;
- nausea, sometimes vomiting;
- lack of appetite;
- feeling full after eating, regardless of the amount of food eaten;
- burning in the stomach and esophagus, belching;
- dark color of the stool if bleeding occurs from the gastrointestinal tract.
Portal gastropathy may present with anemia, which is visible on laboratory tests.
How to recognize portal (congestive) gastropathy?
When diagnosing congestive gastropathy, an effective test is endoscopy of the gastrointestinal tract. In addition, patients are recommended to undergo gastroscopy and colonoscopy of the intestines .
The examination is not very pleasant, so in many cases it is performed under general anesthesia or sedation. Preparation for diagnostic procedures is of no small importance.
The patient needs to follow dietary recommendations and undergo additional examination - abdominal ultrasound, blood test, and so on.
Therapy for portal gastropathy
Treatment of congestive (portal) gastropathy
Portal infiltration is treated carefully. The therapeutic goal of clinicians is to suppress the development of the underlying disease. If the disease is caused by alcohol abuse or cirrhosis of the liver, then the patient is recommended to completely abstain from alcoholic beverages.
In cases where Helicobacter pylori is responsible for the disease, antibiotic therapy should be used.
If portal gastropathy occurs during long-term therapy with analgesics or anti-inflammatory drugs, then drugs are used that suppress the secretion of gastric acid. The patient should be under constant supervision of a gastroenterologist.
Regular endoscopic examinations should also be performed to eliminate the risk of bleeding. In severe conditions, surgery is recommended. Take care of yourself and always be healthy!
Source: https://gastrogid.ru/pochemu-zastaivaetsya-zheludok-zastojnaya-gastropatiya-simptomy-lechenie/
Prevalence
Doctors around the world record diseases of the gastrointestinal tract, and then compile the information into general statistics so that they know what measures to take to limit the disease.
Congestive gastropathy is a fairly common pathological process, even against the background of other nosologies. It occurs not only against the background of poor nutrition, but also when taking certain medications, after prolonged stress, as well as due to accidents and as a complication of other somatic diseases.
More than a quarter of patients taking non-steroidal anti-inflammatory drugs report stomach pain; the percentage of gastropathy after burns, injuries and surgical interventions already reaches eighty. Liver cirrhosis and hypertension also contribute to the general “cauldron”. And given that patients either do not pay attention to the symptoms or hide them from their doctor, the statistics are greatly underestimated.
Congestive gastropathy: causes, treatment and diet
Erosion of the lower part of the stomach must be differentiated from the onset of the ulcerative process. If there is at least one lesion, a series of diagnostic tests are performed to identify Helicobacter pylori. If the result is positive, in addition to the diet, the person takes a course of antibacterial drugs.
The diet for erosive-hemorrhagic gastritis is stricter than for the above forms, since chronic bleeding due to non-healing erosions can lead not only to problems with digestion of food, but also to anemia. We all love to eat delicious food, but how can we make it so that it is also healthy? Below are 3 delicious recipes that will help relieve pain and enrich the body with nutrients.
Cauliflower is cut into small florets and cooked until tender. Pour flour into a heated frying pan and pour in cabbage broth. The cabbage inflorescences are crushed using a blender, boiled milk and a little sugar are added. Bring the mixture to a boil and remove from heat. The egg and sour cream are added to the soup and brought to a boil. It is necessary to eat only warm; hot food has a bad effect on the stomach. Add egg, sugar, sour cream to cottage cheese.
Make the dough, dip it in flour and place it on a greased baking sheet. Bake in the oven for about minutes at 0 degrees, turning as needed. The berries are washed, dried and squeezed, then poured with cold water, boiled and filtered.
Then bring it to a boil again, add sugar and semolina, mix thoroughly, and cook until tender. Then remove from heat, cool, beat and pour into mold. All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical research.
Please note that the numbers in parentheses are [1], [2], etc. Currently, erosive gastritis is not such a rare disease of the stomach. We will talk about what kind of disease this is and how to treat it in a separate topic.
And now we have to find out what nutritional principles the patient should follow, or, more simply, what diet is recommended for erosive gastritis. The principles of nutrition in the treatment of erosive gastritis may depend on the complexity and phase of the disease.
In the acute form, a strict diet is prescribed, and during the period of relief of symptoms, the diet becomes less strict.
Etiology
Congestive gastropathy is caused by frequent and uncontrolled use of non-selective NSAIDs (non-steroidal anti-inflammatory drugs). They are often prescribed because they have several positive effects at once: they reduce inflammation, reduce temperature and swelling, and relieve pain. But patients must adhere to certain conditions that they often ignore or consider unimportant.
The second cause of gastropathy can be called diseases of other systems and organs:
- pancreatic tumor;
- cirrhosis of the liver;
- portal hypertension.
Next in the ranking are accidents associated with the use of chemically active substances. In fourth place are permanent stress and head injuries. And only at the end of the list do gastrointestinal diseases appear, such as reflux of bile or intestinal contents back into the stomach, antiperistalsis.
Symptoms of erosive bulbitis
The main symptom characteristic of any case of bulbitis is pain of varying strength.
- Catarrhal - pain, but minor, localized in the upper abdomen;
- Erosive - severe pain felt on an empty stomach or ten to fifteen minutes after eating, as well as loss of appetite, a feeling of nausea, sometimes turning into relieving vomiting, belching with a bitter taste and heartburn;
- Bulbitis with ulcers or damage to blood vessels - bleeding, accompanied by one of the following symptoms: intense pain, vomiting blood, severe weakness of the body. If blood loss is high, hemorrhagic shock occurs;
- Acute - a significant increase in temperature, frequent and clearly felt nausea, quickly turning into vomiting, indigestion due to insufficient processing of incoming food with enzymes, symptoms of dysbiosis.
Risk factors
Congestive gastropathy does not occur out of nowhere. It is always accompanied by actions or conditions that aggravate or provoke the action of the etiological factor.
These include:
- frequent drinking of alcohol;
- long smoking history;
- age over sixty years;
- presence of chronic diseases;
- the presence of Helicobacter pylori in the stomach (a microorganism that causes one of the types of gastritis);
- ulcer;
- long-term uncontrolled medication use.
Some of these factors are beyond a person's control, but for the disease to develop, a combination of two or three items from the list must be present.
Pathogenesis
Rough, hot or spicy food in large quantities enters the stomach, which is not able to cope with such a volume of work. Because of this, the area of the mucous layer increases, more folds appear, they become taller and thicker. Microcirculation and vascular permeability increase, more mucus and hydrochloric acid are produced. The body is trying to cope with overloads.
The antrum of the stomach is overstretched, which leads to loose closure of the sphincter between the stomach and duodenum. Because of this, the contents of the small intestine, along with bile and pancreatic enzymes, flow back into the stomach, causing burns and atrophy of the mucosa. This further complicates the digestion process.
Treatment of gastropathy
Therapy for functional stomach problems should be comprehensive and include the use of medications, normalization of the patient’s regimen and diet. With insufficient treatment, chronic stagnant gastropathy develops, which subsequently causes structural disorders in the mucosa and its inflammation. Drugs are used that eliminate functional disorders and normalize gastrointestinal motility.
Nutrition for gastropathy
The patient is recommended to eat a gentle diet. To do this, you need to avoid eating fatty, fried or spicy foods. Avoid drinking alcoholic beverages and smoking. When it comes to food, it is better to give preference to boiled or steamed food. Soups and fermented milk products will be useful. It is better to divide all food into 5-6 servings. This will allow you not to burden the gastrointestinal tract and avoid feelings of hunger.
The diet depends on what types of gastropathy the patient has developed.
Symptoms
How does congestive gastropathy manifest itself? Symptoms may appear much later than the onset of the disease itself. This is due to the fact that it takes time for gastropathy to form, and at first a person does not notice any uncomfortable changes in the body.
In a later period, the whole range of dyspeptic phenomena appears:
- nausea with vomiting, heartburn;
- decreased or lack of appetite;
- weakness;
- feeling of heaviness in the stomach, pain when pressing;
- belching and the appearance of a yellow coating on the tongue.
In advanced cases, when the patient stubbornly ignores the symptoms, gastropathy can manifest itself as gastric bleeding.
Symptoms of chronic bulbitis
Chronic bulbitis has a number of specific symptoms. The main signs of chronic bulbitis are nausea and the urge to vomit while eating.
As a rule, this pathological process is accompanied by pain of varying severity, ulcerative lesions, hemorrhages and disruption of the gastrointestinal tract.
The disease may be:
- superficial;
- erosive;
- catarrhal
The chronic form of erosive bulbitis has a more severe course.
This pathology often causes the development of duodenal ulcer.
In this case, a through form of damage to the bulb is observed. The main symptom of the disease is the formation of erosions and hemorrhages.
The pathological process has the most vivid clinical picture.
The acute form of the disease is characterized by the presence of nausea and vomiting, pronounced pain. The patient may feel a bitter taste in the mouth, especially in the morning.
If the pathological process becomes chronic, there are aching pains, which are usually localized in the solar plexus area. Sometimes mild nausea may appear, but there is no vomiting.
This form of the disease can last for several years, periodically manifesting itself in the form of seasonal exacerbations.
The main signs of the erosive form of bulbite include:
- feeling of weakness throughout the body;
- increased irritability;
- nausea and vomiting while eating;
- dizziness and headaches of varying intensity.
Particular attention should be paid to the superficial type of disease, which is less dangerous since it affects only the outer area of the duodenal mucosa.
Such a disease can have a latent course without showing any symptoms.
The main danger of the pathological process is that, against the background of latent symptoms, a sharp exacerbation may begin. As a result, the disease becomes erosive in nature.
To prevent the development of complications, it is necessary to undergo regular examinations with a doctor and pay attention to any changes in the functioning of the body.
The main difference between the chronic course of the disease is less severe symptoms.
In this case, the patient pays attention to the presence of discomfort and nagging pain in the epigastric region. Most often, this symptom appears at night.
Sometimes there may be a feeling of heaviness in the stomach regardless of food intake.
If vomiting occurs, the patient's condition may improve for a while, since a certain percentage of the load is removed from the duodenal bulb.
With chronic bulbitis, a person experiences constant weakness, periodic dizziness and headaches.
In some cases, digestive problems such as constipation or diarrhea may occur.
In this case, there are painful sensations of aching nature. Heartburn medications or milk can help eliminate these symptoms for a short time.
If complications such as Crohn's disease develop, sudden weight loss may occur.
Forms
Morphologically, there are two forms of congestive gastropathy - mild and severe. In mild cases, a mosaic pattern of folds and pathologically dilated vessels is found on the mucosa. In severe cases, there are also hemorrhages and inflammatory spots.
There is also gastropathy, which affects only the antrum of the stomach. It is located on the border with the duodenum, and the first is affected by chyme reflux. When stagnation occurs in the stomach, the passage of food through the antrum slows down, which leads to souring or fermentation of food. This increases the acidity of the environment and damages the mucous membrane. A person experiences pain at night, heartburn, nausea and vomiting.
Focal gastropathy is manifested by areas of redness against the background of gastric changes in the gastric mucosa. Ulcers may appear in these areas over time.
Congestive gastropathy of the body and antrum, congestive bulbopathy
Anton Pavlovich Chekhov, through the mouth of his hero, the secretary of the congress Zhilin, stated that “the doctors invented catarrh of the stomach. This disease comes more from freethinking and pride.”
In Chekhov’s times, “cathars” were the name given to the entire spectrum of stomach diseases. People suffered from them until death, which came much earlier than expected.
Medicine of the 21st century has learned to diagnose and heal the ill-fated catarrh, one of the varieties of which is gastropathy.
Definition and types of gastropathy
The term “gastropathy” refers to a group of diseases caused by damage to the epithelial layer of the gastric mucosa. Unlike gastritis, when there are obvious signs of an inflamed state of the mucous membrane, with gastropathy there is no inflammation, changes affect only the epithelium and its vessels.
Epithelial cells line the inside of the stomach, forming a natural protective barrier. They produce mucus, which protects the organ from hydrochloric acid and mechanical damage. Therefore, how damaged the barrier is, what changes the stomach tissues reacted to negative factors, the following types of disease are distinguished:
- Erythematous gastropathy is redness of the mucous membrane over the entire surface of the stomach or in certain areas.
- Erosive gastropathy is the formation of small, from 2 to 6 mm, ulcers on the mucous membrane, called erosions.
- Congestive gastropathy is a disorder of gastric motility. Blood supply deteriorates, mucosal lesions appear in the form of small ulcerations.
- Hyperemic gastropathy - increased blood flow in the walls of the stomach. The mucous membrane is red due to dilated vessels, edematous.
- Papular gastropathy - small swellings (papules) form in different parts of the stomach. Arranged singly or in groups. The deep layers of the mucous membrane are not affected and heal without scars.
- Hemorrhagic gastropathy - characterized by damage to the vascular wall followed by gastric bleeding.
According to the speed of occurrence and duration of the course, acute and chronic forms of the disease are distinguished. A single strong impact on the stomach of acids, alkalis, alcohol, drugs, microbial toxins gives rise to an acute form of the disease. If irritation from aggressive substances persists, it becomes chronic.
The slow progression of pathological disorders of the mucous membrane is considered a chronic course, in which several stages are distinguished:
- initial, with mild inflammatory processes in the stomach without deep lesions;
- atrophic, when secretory tissue is replaced by connective tissue. Digestion functions are impaired;
- hypertrophic, the most dangerous. The walls of the organ are covered with connective tissue growths and cysts. Food is almost not digested.
The pathological process can cover the entire stomach or a separate part of the organ. For example, congestive gastropathy is a lesion of the lower (antral) part of the stomach due to decreased muscle tone. Food soaked in gastric juice is not evacuated into the intestines for a long time. There is a long-term effect of hydrochloric acid on the bottom part, erosion and ulcers are formed.
Diagnostics
Gastropathy of the stomach does not have specific symptoms. It imitates several gastrointestinal diseases at once, so even the most experienced doctor is unable to understand at first glance what exactly the problem is.
It all starts with a survey, establishing the time of onset of the first symptoms and collecting complaints. Then comes an examination and laboratory and instrumental diagnostics. First of all, the doctor prescribes a general and detailed blood test, biochemical tests, and bacteriological examination of the gastric environment to detect Helicobacter pylori. Characteristic signs are a decrease in hemoglobin and platelet levels.
Fibrogastroscopy is the gold standard in the diagnosis of gastropathy. It allows not only to examine the mucous membrane, but also to collect material for histological examination. A biopsy is taken from pathologically changed areas of the stomach.
If required, the patient undergoes abdominal sonography, radiography, CT or MRI.
Complications
Congestive gastropathy in the antrum is prone to complications. The most common of them include bleeding from pathologically altered vessels of the stomach. Sometimes, this is a late and only symptom of the disease. In more than half of patients diagnosed with gastropathy, fibrogastroscopy reveals ulcers, erosions and perforations.
The most dangerous complication is the development of a tumor process in the gastric mucosa. Since the process of restoration of the mucous membrane is disrupted, and the organ’s protective system works “to wear out,” uncontrolled cell growth may occur against the background of inflammation.
Classification
According to the nature of the pathological process, it can be acute or chronic. The acute form is relatively treatable and rarely leads to serious complications. The chronic form of the disease is almost impossible to eliminate completely, but if you follow the doctor’s recommendations, there is a chance to achieve a long-term stage of remission.
Based on clinical and morphological characteristics, the following forms of gastrobulbitis are distinguished:
- surface;
- catarrhal;
- erosive;
- erosive-ulcerative;
- follicular.
Only a doctor can determine exactly what form of pathology is taking place by carrying out the necessary diagnostic measures. Erosive gastrobulbitis has the most unfavorable prognosis, as it often develops into an ulcer.
Differential diagnosis
Congestive gastropathy is an extremely difficult diagnosis, despite the apparent abundance of symptoms. Since it mimics other nosological forms found in the gastrointestinal tract. The most common among them are gastritis, gastric or duodenal ulcers, pyloric stenosis, antral sphincter insufficiency, reflux disease and other, more exotic diseases.
In order to make the right choice, the doctor prescribes fibrogastroduodenoscopy, bacterial examination, biopsy and other tests. Having excluded all other options, only congestive gastropathy remains.
Treatment
What can be done for a patient diagnosed with “congestive gastropathy”? Treatment begins with identifying the etiological factor and eliminating it. If the damage to the intestinal tube is secondary, then it is advisable to direct all efforts to cure the primary pathology.
To directly relieve the symptoms of gastropathy, proton pump inhibitors, histamine receptor blockers, antacids, antibiotics and drugs that improve microcirculation are used. The doctor’s main task is to select a combination of drugs that would multiply their positive effects and neutralize each other’s side effects.
The role of supportive therapy should not be underestimated. The patient must be prescribed B vitamins, especially B12, since if the gastrointestinal tract is disrupted, its amount decreases sharply. In addition, it is advisable to take vitamins C and K. In addition, the patient is advised to walk more in the fresh air, do gymnastics and strengthen the abdominal muscles and diaphragm.
Treatment of chronic bulbitis with medication
It is necessary to treat the chronic form of bulbitis using complex therapy.
In this case, both medicinal and non-medicinal means, as well as traditional medicine methods, are used.
The choice of medications for this disease directly depends on the factor that provoked the pathological process.
When treating Helicobacter pylori infection, the doctor prescribes eradication therapy, which involves eliminating the Helicobacter pylori bacterium.
In this case, antibiotics and drugs that reduce the level of acidity in the stomach are used.
The duration of treatment and dosage of certain drugs is determined by the attending physician.
In most cases, anti-inflammatory drugs are prescribed to help restore the normal state of the mucous membrane.
To eliminate pain, it is strictly forbidden to use non-steroidal anti-inflammatory drugs, since they have a damaging effect on the mucous membrane.
As painkillers, the doctor may prescribe antispasmodic drugs such as Duspatolin and Trimedat.
To reduce acidity, antacid drugs are used, for example Maalox, Reni, Almagel.
Of the non-drug methods, physical therapy is considered the most effective.