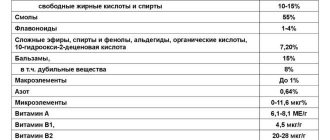
Instructions for use
Furazolidone is used in the treatment of a number of diseases caused by pathogenic bacteria of various types. The regimen for taking the drug may differ depending on the type of infection present and the individual health characteristics of the patient. Approximate dosages are indicated in the instructions. The duration of the course of treatment is adjusted by the attending physician. Additionally, the instructions describe the composition of the drug, the nuances of its pharmacological properties, indications for use and a list of possible contraindications (including side symptoms that may occur if the drug is used incorrectly).
pharmachologic effect
Furazolidone belongs to the group of antimicrobial and antiprotozoal agents. The drug is active against a number of pathogenic microorganisms and belongs to the group of nitrofuran derivatives. The drug has a bactericidal and bacteriostatic effect. The effect on the body is carried out at the cellular level.
Additionally, components from Furazolidone activate the immune system, increasing cell resistance to the negative effects of external factors and bacteria.
Properties of the drug
blocking the enzymatic properties of pathogenic microorganisms;- elimination of the consequences of toxic effects on the body;
- destruction of protozoan pathogenic organisms (Trichomonas and Giardia);
- relieving the consequences of protozoal and bacterial infections;
- suppression of the Krebs cycle;
- destructive effect on cholera vibrio;
- stopping the synthesis of nucleic acids;
- destructive effect on salmonella, campylobacter and shigella.
Indications for use
Furazolidone is prescribed to patients suffering from inflammatory and infectious diseases of the gastrointestinal tract, genitourinary system, and skin.
The drug is used to treat:
- paratyphoid, typhus;
- bacillary dysentery;
- enterocolitis;
- giardiasis;
- trichomonas infection;
- diarrhea caused by infectious causes (including food poisoning);
- urethritis, cystitis;
- infected wounds, skin burns.
Mode of application
Furazolidone is recommended to be taken orally, after meals, because it can cause dyspeptic disorders. You need to take the tablets with a glass of water. If the drug is taken for a long time to prevent neuritis, the patient is prescribed B vitamins.
For the treatment of dysentery, paratyphoid fever, foodborne toxic infections, Furazolidone is taken for 7-10 days, 100-150 mg four times a day.
For colpitis, the drug should be taken three or four times a day, 100 mg. Duration of therapy – 3 days. In parallel with this, once a day 5 g of powder is injected into the vagina, which consists of a mixture of lactose (milk sugar) with Furazolidone in a ratio of 400:1, and rectal suppositories with Furazolidone are injected into the rectum.
For children, the drug is prescribed at the rate of 10 mg per 1 kg of child weight per day (the daily dose is divided into three doses), and for adults - 100 mg four times a day.
Furazolidone can be used to treat burns and wound infections. In these cases, it is applied topically in the form of irrigation with Furazolidone solution or wet-dry dressings.
Release form, composition
The drug is produced in the form of flat-cylindrical tablets containing the active active substance (0.05 g) and auxiliary components - potato starch, sucrose, calcium stearate, lactose, polysorbate. The tablets are placed in blister-free and blister packs, and then in cardboard packs.
Interaction with other drugs
Since the drug is a monoamine oxidase inhibitor, the same precautions must be taken when using it as when using other monoamine oxidase inhibitors.
When taking ristomycin and chloramphenicol, the drug increases the inhibition of hematopoiesis.
Tetracyclines and aminoglycosides enhance the antimicrobial properties of Furazolidone.
The drug is incompatible with alcohol, because this combination may cause disulfiram-like reactions.
Features of taking the drug Furazolidone for gastritis
How much and in what dosage should Furazolidone be taken? Instructions for use state that adults need to consume 100-200 mg of the drug daily. The dosage will depend on the severity of the disease and the presence of concomitant pathologies. When treating children, the dosage is selected taking into account body weight. Usually it is 10 mg per 1 kg of weight.
The duration of the course of treatment is determined individually. As a rule, it is 5-10 days. Furazolidone tablets can also be taken in cycles of 2-3 days. Between each cycle there is a break of 5-7 days. The course of treatment with Furazolidn is allowed to be carried out no more than once a month. These tablets for diarrhea and infectious diseases have a number of contraindications.
Taking Furazolidone is strictly prohibited during pregnancy, since the active components of the drug can penetrate the placental barrier. Also contraindicated for use is the lactation period, age under 1 year, lactase deficiency. A person taking Furazolidone should not suffer from renal failure, organic damage to the central nervous system or hypersensitivity to the active components of the drug.
If you have chronic liver diseases, you can take the medicine, but in this case you need to reduce the dosage and monitor the level of liver enzyme activity. The use of Furazolidone when working with potentially dangerous mechanisms is not allowed, since its metabolites can negatively affect the reaction rate and the functioning of the central nervous system as a whole. Also, while taking this drug, it is strictly forbidden to drive vehicles.
Sources:
- https://wer.ru/opisanie/furazolidon/
- https://www.gastroscan.ru/handbook/144/1547
- https://gastritinform.ru/medknizh.ru/narodnye-sredstva/furazolidon-pri-gastrite/
- https://gastritinform.ru/peptic.ru/parazity/lekarstva/furazolidon-ot-chego.html
Side effects
Despite the fact that Furazolidone is considered a low-toxic drug, its use can cause the appearance of:
- itching of the skin, Quincke's edema, skin rash;
- vomiting, nausea;
- hepatotoxic effect;
- loss of appetite;
- bronchospasm, neuritis, pulmonary edema (with prolonged use).
Anemia, hypovitaminosis C and B, and diabetes mellitus increase the risk of peripheral neuropathy.
You can avoid the development of adverse reactions if you take B vitamins, antihistamines, and take each dose of the drug with a large volume of water.
Overdose
It is recommended to take Furazolidone in strict accordance with the testimony of a specialist or the regimen presented in the instructions. If the dosage is exceeded, the risk of side symptoms increases not only in the functioning of the body's lavatory systems, but also in changes in blood composition. An overdose will significantly worsen the patient's condition and reduce the tendency for his recovery.
Consequences of overdose:
- neuritis;
- bronchospasms (or pulmonary edema);
- toxic hepatitis;
- changes in blood composition;
- polyneuritis.
Did you know that the most common disease of the 21st century is liver disease? Find out more about liver disease:
- How to recognize the first signs of hepatitis and effectively cope with the disease?
- An interesting article about liver cirrhosis, you will learn about the history of the disease and its prevalence in the world.
- Pain or discomfort in the right hypochondrium? Perhaps it's hepatosis! Find out how it can be cured.
Contraindications
Furazolidone is not prescribed in the following cases:
- with individual hypersensitivity to the drug;
- in the presence of end-stage chronic renal failure;
- for the treatment of children less than 1 month of age;
- with lactose, glucose-6-phosphate dehydrogenase deficiency.
With great caution, the drug should be prescribed to persons suffering from diseases of the liver apparatus and nervous system. The drug should not be prescribed to patients whose activities require quick reactions and high concentration.
During pregnancy
Furazolidone is a Category C drug. This means that animal studies of the drug have shown no adverse effects on the fetus, but there is no information on the effect on the human fetus.
According to the instructions, the drug is not intended for use during pregnancy, but can be prescribed as necessary, taking into account the risk to the fetus and the expected benefit to the mother.
Reviews of the use of Macmiror for gastritis
It was prescribed to me just to combat Helicobacter. However, she is so disgusting, you can get rid of figs from the body with one medicine - you have to take a whole ton of medicines. Macmiror is an excellent antibacterial agent, one of the few that can generally fight this scourge.
cornflower2016
Hello everyone! I’ll tell you a little story about my use of the drug Macmiror. One day I complained to a gastroenterologist about abdominal pain and nausea. Without conducting any tests, the doctor prescribed me this drug. Manufacturer: Country of origin: Italy. In general, I think Italian drugs are one of the best. Packaging: Ordinary cardboard box and 20 small tablets. The tablet size is small, does not cause discomfort when swallowing. Active ingredient: Nifuratel. Indications: Diseases of the gastrointestinal tract caused by the Helicobacter bacterium, pyelonephritis, cystitis, diseases caused by microorganisms, etc. Contraindications: Side effects: Nausea, vomiting, bitterness in the mouth, diarrhea, heartburn. Allergic reactions: skin rash, itching.
Consequences: After seeing the doctor, I came home and took one tablet, after which I wanted to take a nap, I woke up about half an hour later because my body was very itchy. But what’s worse is that I felt my gums swollen. This scared me very much. With this one tablet, my treatment with this drug ended, as I am sure it can be life-threatening. I don't intend to take any more risks. It’s a pity that you have to experience the beauty of side effects and allergic reactions firsthand. Probably, if preliminary tests had been carried out to determine the possibility of an allergy to the components of this drug, then treatment would have been much easier. RESULT: I stopped taking the drug from the first tablet. I will not take this drug again.
mcmiror price
Yancy
Good day!
We were faced with the problem of giardiasis, Macmiror really helped, we were treated with a course of 10 days, the drug is modern and effective without side effects, on the first day the improvements were not significant because the drug has a cumulative effect, the effect came after the fifth day of use, appetite improved, abdominal pain decreased, the general condition improved, the stool became regular and normal, we drank along with the filtrum, and after the course, maintenance therapy for the gall and liver is definitely needed, we drank hophytol 3 times a day, a package of 60 tablets was enough for 20 days, this turned out to be quite enough, despite the price of the drug very worthy. beHelen74
I had a stomach ache for a long time and I found the strength to do a gasteroscopy. Helicobacter was detected in small quantities. The attending physician proposed a gentle treatment regimen (what is gentle about it I still don’t understand - three drugs Macmiror, Rabeloc and Helinorm - all drugs from Helik, quite expensive). I started the course of Macmiror in the evening on an empty stomach (as indicated doctor) - and after half an hour the headache began to hurt... Now it’s the second day of treatment, and the headache still does not go away. I also suffer from weakness and itching (well, you understand where). I assume that the guests of my body decided to pack their bags and run away, including from my head (what if they lived there too?) The urine turned lemon-colored (I read about such side effects) I hope the headaches and empty wallet will be worth it, that the body will become cleaner. I’ll add to the review: the headaches went away after a week when I finished taking Macmiror. A course of treatment of three drugs had a positive effect on the body (but in fact, treating Helicobacter is useless, because it can be picked up again from a poorly washed apple).
Sources:
- https://telegraf.by/2012/03/press-relizi/kogda-sleduet-prinimat-makmiror
- https://toxinam.net/polezno/preparaty/makmiror-kompleks-instrukcija.html
- https://sovets.net/15770-makmiror.html
- https://www.tiensmed.ru/news/macmiror-n7d.html
- https://chebo.pro/zdorove/instruktsiya-po-primeneniyu-antibiotika-nifuratel-ego-analogi.html
special instructions
Impact on driving vehicles and operating machinery
No negative effects were identified.
Pregnancy and lactation
Absolute contraindications for the use of Furazolidone are lactation and pregnancy.
Use in childhood
The drug is used in pediatric practice (in the form of a suspension, Furazolidone is allowed to be prescribed to children from one month, in the form of tablets - from three years).
For impaired renal function
Furazolidone is contraindicated.
For liver dysfunction
The drug is contraindicated.
Conditions for dispensing from pharmacies
A prescription is required.
Antibiotics for the treatment of Helicobacter pylori
One of the factors causing gastritis and peptic ulcers is a gram-negative spiral-shaped bacterium. An antibiotic against Helicobacter pylori is a necessary component of the treatment regimen. Without its use, getting rid of the bacteria is impossible. It has developed resistance to many of the classic antibacterial agents, so it is advisable to use the best drugs of new generations in treatment.
Analogs
There are no analogues of Furazolidone for the active substance. Drugs that have a similar effect include the nirofuran derivatives Entprofuril and Nifuroxazide, as well as a number of antibiotics: Rifaximin, Azithromycin, Fluoroquinolone, Imipenem, Ciprofloxacin, Amikacin.
All gastroenterology clinics and medical centers in your city. Tests and ultrasound. Consultation with a gastroenterologist. Diseases of the digestive system. Find out more: - In Kiev (Hertz, Ilaya, Euromed) - In St. Petersburg (SM-Clinic, Longevity, Allergomed, Doctor +, BaltZdrav, Professor) - In Moscow (SM-Clinic, Medlux, Onmed) - In Kharkov ( TsMEI, Olympic, Victoria, Fortis, Ecomed) - In Minsk (Belgirudo, Art-Med-Company, Sinlab, Mikosha, GrandMedica, MedClinic) - in Odessa (Medea, On Clinic, Into Sano, Venus) - In Razyan (Trust + , Polyclinic-Pesochnya, Evrikas +) - in Nizhny Novgorod (Only Clinic, Alpha Center, EuroClinic, SOLO, Altea) - gastroenterological clinics of Tyumen (Doctor A+, Clinic "Vera", Avicenna, Medis, Sibirina, Your Doctor)
Reviews
Doctors focus on the fact that the drug is positioned as a synthetic antibacterial agent - a drug that differs from antibiotics in its effect on the human body and the mechanism of action on microorganisms.
Some patients share their experience of using the drug for ailments not listed in the instructions.
For example, in the treatment of erosive and ulcerative diseases in adults, anti-Helicobacter pylori therapy including Furazolidone is effective. The same regimen is used to treat children infected with Hilicobacter pylori.
A number of reviews mention side effects - nausea and vomiting. That is why, before using the product, you need to familiarize yourself with the contraindications and consult a doctor, and subsequently follow the recommended doses.
You can read patient reviews about Furazolidone at the end of the article.
Helicobacteriosis treatment regimen
To date, a list of drugs that are highly effective in eradicating this infection has been established:
- Colloidal bismuth subcitrate (De-nol). There are treatment regimens with or without De-nol. But it has been proven that the effectiveness of the therapy is much higher when De-nol is included in the treatment regimen. This is due to the fact that this drug significantly reduces the absorption of antibiotics. They are concentrated in a higher dose precisely in the digestive tract, in the habitat of Helicobacter pylori.
- Antibiotics. Drugs of the amoxicillin group (Augmentin, Flemoxin solutab, Amoxil), clarithromycin (Klacid), azithromycin (Sumamed, Ziomycin, Ormax).
- A group of antisecretory drugs (Omez, Ranitidine, Gastromax, Gastrocepin).
- Antimicrobial drugs (Macmiror, Metronidazole).
The duration of the standard course of treatment is 7–10 days. In more severe cases, the course can be extended to 14 days.
There is first-line therapy, the so-called triple regimen, and second-line therapy, the so-called quadruple therapy. The first line can be with or without the use of De-nol. How to treat the patient and what therapy to start with is decided by the doctor after a full examination.
Triple therapy includes:
- De-nol (1 t in the morning);
- antibiotic (amoxicillin or clarithromycin or azithromycin group) + antimicrobial agent (Macmiror, Metronidazole).
- De-nol;
- 2 antibiotics (from the amoxicillin group + from the clarithromycin or azithromycin group).
Triple therapy includes:
- antisecretory drug (Omez, Gastromax, Gastrocepin);
- antibiotic (from the group of amoxicillin, clarithromycin or azithromycin) + antimicrobial agent.
- antisecretory drug;
- 2 antibacterial agents (from the amoxicillin group + from the clarithromycin or azithromycin group).
Quad therapy (quadruple therapy) includes:
- De-nol;
- an antibacterial agent (your choice of amoxicillin, clarithromycin or azithromycin);
- antisecretory drug (Omez);
- antimicrobial drug (Macrimor or Metronidazole).
Azithromycin preparations (Sumamed, Ziomycin, Ormax) are added to therapy on the 3rd – 4th day of treatment and prescribed for 3 – 5 days.
A big problem in the treatment of helicobacteriosis is the resistance of bacteria to antibiotics. This is due to the frequent and uncontrolled use of antibacterial agents to treat various diseases.
To resolve the question of what antibiotics should be used to treat a patient with unsuccessful eradication in the first and second lines of therapy, a study is conducted to determine the sensitivity of Helicobacter pylori to antibiotics during fibrogastroscopy. After this, a third-line treatment regimen is selected using an antibiotic to which the particular patient’s bacteria is highly sensitive.
If, in addition to the underlying disease, the patient also has reflux disease (reflux of gastric contents from the stomach into the esophagus), then domperidone drugs (Motilium, Motilak) are added to therapy.
Additional administration of probiotics (Lactobacterin, Bifidobacterin) is also used. It has been proven that the combined use of probiotics with antibacterial therapy improves the barrier functions of the stomach and slows down the growth of H. pylori, since the bacteria contained in them compete with Helicobacter. As a result, the percentage of eradication increases.
Published in the journal: “Infectious Diseases” 2008, Volume 6, No. 3. S.Yu.Konanykhina 1, O.A.Serdyuk 2, I.I.Stepanova 2, M.L.Kastorina 3
1 Research Institute of Vaccines and Serums named after. I.I. Mechnikov RAMS, Moscow; 2 Institute for Diagnostics and Prevention of Socially Significant Diseases, Moscow; 3 University of Pavia, Italy
67 patients with chronic inflammatory diseases of the upper gastrointestinal tract associated with H. pylori were examined (histological examination of biopsy specimens and immunochromatographic examination of fecal samples). Patients received omeprazole (0.5 mg/kg/day; 40 mg/day - children and adults, respectively), amoxicillin (30 mg/kg/day; 2g/day) and nifuratel (30 mg/kg/day) for 10 days. ; 800 mg/day). All patients showed positive dynamics of clinical symptoms and epithelization of erosive and ulcerative defects of the mucous membrane. Eradication was achieved in 93.8% of children (30 out of 32 patients) and in 88.6% of adults (31 out of 35 patients) according to the results of histological examination of biopsy specimens and immunochromatographic examination of fecal samples. The coincidence of results was noted starting from the 6th week after eradication (p > 0.05). Thus, a regimen based on nifuratel in combination with a proton pump inhibitor (PPI) and amoxicillin is effective and safe for the eradication of H. pylori infection in children and adults. A non-invasive immunochromatographic rapid test based on monoclonal antibodies for determining HP antigens in fecal samples can be used to diagnose H. pylori infection and evaluate the effectiveness of therapy.
Key words: Helicobacter pylori, diagnosis, histology, H. pylori antigen in fecal samples, eradication, nifuratel, omeprazole, amoxicillin
Currently, the increase in diseases of the gastrointestinal tract, of which the share of lesions in the gastroduodenal zone accounts for up to 75%, represents a serious medical and social problem. In recent years, there has been a rejuvenation of gastroduodenal pathology, a change in the morphogenesis and nature of the course of the pathological process in the gastroduodenal zone: the absence of a typical clinical picture of the disease, a long-term recurrent course, an increase in the frequency of destructive lesions, including ulcerative ones. In the development of chronic inflammatory and destructive processes in the gastroduodenal zone, the etiological role of Helicobacter pylori (HP) is generally recognized [1-4]. 80% of cases of chronic gastroduodenitis and peptic ulcer are associated with the persistence of HP in the mucous membrane, which made it necessary to include antibacterial drugs in the complex treatment of these diseases. Treatment regimens for HP-associated diseases of the gastroduodenal zone include drugs that affect secretion (from the group of H2-histamine blockers or proton pump inhibitors - PPIs) and at least two antibacterial drugs in various combinations (clarithromycin, amoxicillin, metronidazole, bismuth subcitrate, nitrofurans). The most common treatment regimen worldwide is a combination of a PPI with clarithromycin and/or amoxicillin and/or metronidazole. However, widespread and long-term use of metronidazole and clarithromycin led to the formation of HP strains resistant to nitroimidazoles and macrolides and a decrease in the effectiveness of therapy to 60-80% [5-8]. In recent years, in many countries with high natural resistance of HP to metronidazole, regimens with nitrofurans (furazolidone and nifuratel) have been successfully used in children and adults [9-16]. At the same time, regimens in which amoxicillin is replaced by clarithromycin demonstrate worse treatment results—a reduction in the eradication rate to 75% [10, 17]. In Russia, according to the results of clinical studies, triple regimens based on PPIs or bismuth subcitrate, amoxicillin and nifuratel provide a high incidence of HP eradication (80-92%) and are recommended as first-line therapy in children [9-13].