Diagnosis of Helicobacter pylori infection is a complex process, since none of the available tests alone can serve as the basis for making a final diagnosis. A person can be a carrier of Helicobacter pylori throughout his life, and the manifestation of clinical symptoms is not necessary.
There is experimental data on the possibility of spontaneous elimination of infection, however, in most cases, the selection of adequate treatment methods under the supervision of a physician is required.
Helicobacter pylori: general information about the microorganism
Helicobacter pylori (Helicobacter pylori) is an opportunistic bacterium of a spiral shape, Gram-stained red (gram-negative). The predominant habitat in the human body is the stomach and duodenum.
The role of Helicobacter pylori in the development of diseases of the gastrointestinal tract (GIT) has been denied for a long time. Only in 2005, Australian pathologist R. Warren and physician B. Marshall managed to prove the medical significance of bacteria, for which they were awarded the Nobel Prize.
Feature: in 90% of carriers, Helicobacter pylori is part of the normal microflora and does not cause the development of an infectious disease. However, there is an opinion that this particular species is the cause of many gastrointestinal pathologies (ulcers, gastritis, cancer, lymphoma).
Relation to opportunistic bacteria means their ability to provoke an infectious process in the presence of certain conditions (factors). For example, long-term use of antibiotics with subsequent dysbacteriosis, decreased immunity and the presence of concomitant pathologies. However, when infected with strains with pronounced pathogenic properties, the presence of the above factors is not necessary.
Immunoglobulin analysis
How can Helicobacter pylori be detected in the blood? Another method is an immunoglobulin test. This is the name given to specific proteins that take an active part in the “battle” with the infecting antigen.
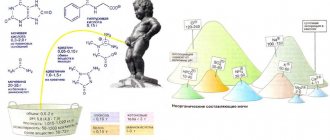
There is one peculiarity - they are not produced immediately. When fixing damage to the patient’s body, Helicobacter is given importance to the detection of three types of these proteins in the blood - M, A, G. In the inflammatory process, each of them will play its own special role:
- M is an indicator of early infection of the body, when a person does not yet show any symptoms. Note that it is found very rarely. However, this fact makes it possible to prevent infection of the family and relatives of the person being examined.
- A - also indicates an early degree of infection with a bacterium or a clear inflammatory process. Possible detection in the saliva and gastric juice of the subject. A high content of immunoglobulin A indicates the infectiousness of Helicobacter and the high activity of the bacterium.
- G – this marker confirms the presence of Helicobacter pylori in the body in general. The bacteria may be detected after 3-4 weeks of residence. However, it should be noted that high levels of this titer will persist for some time after the death of the bacterium and the complete cure of the patient.
Now let's look at the pros and cons of this type of analysis for Helicobacter pylori. The advantages of the method are as follows:
- Laboratory testing is quite effective. Statistics show that immunoglobulins G are detected in 95-100% of cases, group A proteins in 65-85% of cases, category M in 18-20% of cases.
- You can compare the results of this analysis with those of previous ones. This helps to track the development of the pathological process, detect deviations from the norm, and judge the effectiveness of the prescribed therapy.
- The study will be more likely to prove that the body is infected than an enzyme immunoassay for antibodies.
But this research methodology also has a number of disadvantages:
- Almost a month must pass before the most important marker (immunoglobulin G) appears. Such delayed diagnosis does not contribute to the effectiveness of therapy.
- After complete cure (especially in older patients), the high titer persists for quite a long time - up to 1-1.5 years.
- The research method does not allow distinguishing the acute stage of damage from passive penetration of Helicobacter into the stomach.
Where does Helicobacter pylori come from and how is it transmitted?
The infection is not transmitted by airborne droplets, since it is a strict anaerobe (dies on contact with oxygen). You can become infected by neglecting the rules of personal hygiene (cutlery and dishes, personal cosmetics and personal hygiene products), as well as by kissing.
Primary infection can occur in childhood (from mother to child). Another route of infection is water and meat that has undergone insufficient heat treatment. Infection through an endoscope, which is used for gastroendoscopy, is possible.
How does infection occur?
Rapid colonization of the mucous membrane of the gastrointestinal tract is ensured due to the high degree of mobility of Helicobacter pylori (using flagella). Specific proteins and lipopolysaccharides on the surface of the membrane help bacteria attach to the surface of cells. The presence of foreign antigens provokes the development of an immune response (the release of specific antibodies to Helicobacter pylori) and initiates inflammation of the mucous membrane.
Bacteria release enzymes into the external environment that dissolve the protective mucus of the stomach. Survival in the acidic environment of the stomach is ensured by the enzyme urease, which decomposes urea with the release of ammonia (neutralizes hydrochloric acid). A side effect of ammonia is chemical irritation of cells followed by their death. Along with this, bacteria release toxins that enhance the process of cell degradation and death.
Detailed description of the study
Helicobacter pylori is a bacterium that affects the gastric mucosa due to its resistance to acidic environments.
It is assumed that infection with this infection occurs at an early age and is transmitted to children from parents or in preschool institutions. The most likely route of infection is considered to be the fecal-oral route of infection when living with an infected person in the same house, as well as during a long stay in a large group.
In addition, the oral route of transmission of infection through saliva and kissing has been recorded. There have been suggestions about the possibility of Helicobacter pylori infection during fibrogastroscopy - an examination through an endoscope that has been insufficiently treated with disinfectants.
After penetration into the stomach, Helicobacter pylori colonizes its mucous membrane, causing gastritis of the antrum of the stomach. The bacterium is protected from exposure to an aggressive acidic environment by producing alkali (ammonia) and some other substances that damage the gastric mucosa.
In response to Helicobacter pylori entering the body, the immune system produces antibodies. Initially, antibodies of class A and M are formed, they are soon replaced by immunoglobulins of class G. In most cases, the body is not able to completely defeat this infection, which predetermines the preservation of a high level of class G antibodies to it.
When combined with other unfavorable conditions, such as stress, poor diet, and infection with this bacterium, it leads to the formation of erosions and stomach ulcers. The following symptoms are noted:
1. pain in the upper abdomen (on an empty stomach);
2. nausea;
3. belching air;
Some people are asymptomatic when infected with Helicobacter pylori. Long-term damage to the gastric mucosa by this bacterium leads to the development of atrophy and decreased acid production. The risk of developing stomach cancer and lymphoma increases. A particularly high risk of developing cancer is observed in those whose relatives suffered from it.
Determining the presence of Helicobacter pylori infection in the body is important for early diagnosis of gastric pathology. Class G antibodies are produced several weeks after infection and are detected throughout life in the presence of bacteria in the body.
This test is relevant, in combination with other antibodies (IgA, IgM), as a primary diagnosis of this infection, but is not recommended for assessing the effectiveness of treatment, because IgG may persist for a long time even after successful therapeutic measures.
Symptoms of Helicobacter pylori in adults
In most cases (up to 70%), carriage does not manifest itself in the form of clinical symptoms and is discovered accidentally during a comprehensive examination of the patient. However, pathologies of the stomach and intestinal tract, accompanied by Helicobacter pylori infection, have certain signs:
- feeling of pain in the abdominal area (stomach);
- frequent heartburn and belching;
- unexplained loss of appetite and weight;
- nausea or vomiting;
- heavy coating on the tongue;
- inflammation of the gums;
- putrid odor from the mouth (with the exception of dental diseases);
- feeling of heaviness after eating food;
- increased gas formation.
It was noted that in children the severity of clinical signs is higher than in adults. This situation is especially often observed in the presence of physical or emotional stress, as well as when the diet changes for the worse (replacing soups with sandwiches or eating irregularly).
Patients ask the question: when should you get tested for Helicobacter pylori? A referral for laboratory diagnostics can be issued by a general practitioner, pediatrician, gastroenterologist or infectious disease specialist. Indications for testing for Helicobacter pylori: suspicion or presence of gastrointestinal disease, as well as the manifestation of the above symptoms.
How to get tested for Helicobacter pylori?
Methods for identifying Helicobacter pylori are different:
- breath (urease) test;
- real-time PCR to detect pathogen DNA;
- enzyme-linked immunosorbent assay (ELISA) to determine the level of antibodies produced in response to infection;
- one-step immunochromatographic method for detecting pathogen antigens in the test material;
- biopsy during esophagogastroduodenoscopy.
Depending on the diagnostic method, the biomaterial studied, the cost and timing of the study differ. It is important that the patient follows the rules for preparing for the analysis; the accuracy and reliability of the results obtained depends on this. Let's take a closer look at each method.
What is a urease test for Helicobacter pylori?
Detection of Helicobacter pylori using a breath test. The Helicobacter pylori test is increasingly used in routine diagnostic practice. Advantages of the method:
- short time to obtain results (up to several hours);
- low cost;
- painlessness;
- no contraindications;
- no need for expensive equipment.
Disadvantages include the possibility of obtaining a false negative or false positive result. Reduced reliability of the study due to internal bleeding.
In what cases can a urease breath test for Helicobacter show a false negative result? In addition to improper preparation of the patient for the test and errors at the stage of collecting biomaterial, a false negative result can be obtained when infected with strains that do not produce urease. In other words, even if bacteria colonize the patient’s gastrointestinal tract but do not release urease, the test result will be negative.
Preparing for the ureaplase test
For 3 days, alcohol and medications in which alcohol is a solvent are completely eliminated. For 6 hours, food intake is limited, clean unsweetened water is allowed to drink. The minimum interval between the last dose of antibiotics and bismuth-containing drugs is 6 weeks. It is advisable to stop taking any medications 2 weeks in advance, in consultation with your doctor.
Collection of biomaterial (exhaled air) is allowed 24 hours after FGDS (gastroscopy).
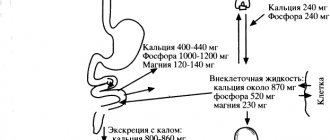
10 minutes before collecting air, you should drink juice (grapefruit or orange) in order to slow down the evacuation from the stomach. Then the patient exhales as much air as possible into a special bag.
After which you need to drink a solution of urea labeled with a carbon isotope (50 ml for adults, 25 ml for children under 12 years of age). The solution has no specific taste or smell; it must be prepared immediately before use. After 30 minutes, a control collection of exhaled air is carried out.
Both samples are analyzed on a special device and the carbon dioxide ratio is determined.
Preparation for testing and duration of the study
Your doctor will tell you in detail how to take the test. Preparation includes:
- exclusion from the diet the day before blood donation of fatty foods;
- a categorical ban on alcohol;
- medication should be stopped 2 weeks in advance;
- minimizing physical activity;
- On the morning of the test, you are not allowed to have breakfast, you can only drink water (at least eight hours must have passed since your last meal).
Plasma is obtained from venous blood taken by sedimentation of red blood cells and other elements. Using a micropipette, it is introduced into the wells of a special plate with an antigen standard applied to them. Between substances, in the presence of antibodies in the serum, a reaction occurs and complex compounds are formed, which are visualized by adding a coloring compound.
The amount of antibodies is judged by the degree of coloring
For a more accurate assessment of the result, photometry is carried out using a spectrophotometer. It compares the material under study with control samples. Mathematical processing allows you to obtain quantitative indicators. The laboratory test for immunoglobulin G takes 24 hours to prepare, and the patient will receive the result the next day. A week is needed to study other globulins.
Antibodies to Helicobacter pylori
Infection with Helicobacter pylori infection triggers protective immune responses. Immunoglobulin M (IgM) is produced first, followed by large quantities of IgG and IgA. Blood testing for antibodies to Helicobacter pylori allows one to establish the fact of infection, since IgG is detected in 90–100%, and IgA in 80% of cases.
It should be noted that a blood test for Helicobacter pylori may be an alternative to invasive diagnostic methods (if endoscopy is not possible). This rule does not apply to elderly patients. The strength of their immune response is insufficient, so it is possible to obtain false negative results.
A high titer of IgG indicates recent infection and an active process of infection, provided that the patient has not taken antibiotics. The IgG concentration remains moderately elevated for a long time (up to 1.5 years), so this test is not used to assess the effectiveness of the chosen treatment.
The IgA value allows you to determine the severity of the infectious disease. A low IgA content persists for up to several years; however, the absence of positive dynamics in reducing its value indicates the ineffectiveness of treatment.
How is blood donated for Helicobacter pylori (how is the test taken)? The biomaterial is venous blood from a peripheral vein on the elbow. No special preparation is required for the analysis. It is advisable to donate blood for Helicobacter pylori after 2-3 hours without food; smoking is prohibited for half an hour.
What does it mean if Helicobacter pylori IgG is positive?
If antibodies to Helicobacter pylori IgG are detected in the biomaterial, then a conclusion is drawn about:
- active infection - in the presence of a pronounced clinical picture;
- bacterial carriage.
A decrease in the IgG titer in a blood test for Helicobacter by 25% within six months after completion of treatment indicates the death of bacteria.
How to get tested
You have decided to get tested for Helicobacter pylori. How to do this, how to prepare for analysis?
First of all, you need to know that there are several ways to do this, and it is better not to rely on one of them, but to conduct at least 2 studies. Let's give the simplest ones.
Blood analysis
Your doctor may ask you to take a blood test to see if you have antibodies to Helicobacter pylori.
For reference. Our body fights infection and produces special antibodies that bind to the pathogen to neutralize it. If the patient’s blood contains these antibodies, then we can say that he is infected.
A blood test is given in the morning, blood is collected from the cubital vein.
The preparation for it is standard, but it still doesn’t hurt to remind you about it:
- You should not take medications or drink alcohol 2 days before the test.
- Before going to the laboratory, you should not play sports or go to the bathhouse.
- Before taking the test, you should not eat fatty or spicy foods.
- You need to avoid stress, take care of yourself, and don’t get nervous.
- Blood for Helicobacter pylori analysis must be taken on an empty stomach, i.e. The last meal should be the night before. In the morning you cannot have breakfast, even drink juice, coffee or tea, or smoke.
Urease breath test
For reference. The bacterium Helicobacter pylori synthesizes urease, this is a special enzyme. It can affect urea, breaking it down into carbon dioxide and ammonia in the intestines.
When conducting a study, they look at the concentration of these substances in the exhaled air before and after taking urea.
First, the patient breathes through a special tube. There is no need to worry or worry, breathing should be the same as in normal life. After the results have been obtained, the person is asked to drink a solution of urea (5%). You must wait 5 minutes and then take the sample again.
To determine whether a person is infected or not, it is necessary to check the concentration of ammonia in the exhaled air. If it is high enough (more than 0.5 mg/ml), then the test is positive. For the test to be correct, no saliva must enter the tube. If you can’t swallow it, you can sometimes pull out the tube.
In case of saliva contamination, the examination will have to be repeated.
How to prepare for the study:
- You should not take medications that reduce the acidity of gastric juice. It is worth abandoning them 3 weeks before the examination. These are antacids, antibiotics, etc.
- You will have to forget about alcoholic drinks for a while. You should not take them at least 3 days before the examination.
- The day before you go for the test, you should not eat foods that contribute to gas formation: brown bread, cabbage, peas, potatoes, etc.
- You must take the test on an empty stomach and have a light dinner beforehand.
- Before being examined, i.e. in the morning, you can’t smoke and have breakfast.
- During the day, do not chew chewing gum, which promotes strong salivation.
As we can see, preparing for the test is not difficult, but it is better to start it in advance.
Stool analysis
To determine whether the bacteria Helicobacter pylori is present in the body, you can take a stool test. Before taking stool for analysis, 3 days before you collect the material, you must give up dyes and dietary fiber, and you cannot take medications for constipation.
How to prepare for the analysis?
For reference. 72 hours before submitting stool for analysis, you should stop taking medications and medicinal suppositories in order for the result to be correct. A person must go to the toilet himself, without the help of laxatives. Do not stain biomaterial with urine or blood.
Feces should be stored in clean containers. It is better to go to the toilet in the morning and immediately take the stool to the laboratory. If that doesn’t work, you can do it in the evening, but the material should not be stored for more than 10 hours. And in this case, it must be kept in the refrigerator, at a temperature not exceeding 8 degrees.
Stool analysis for Helicobacter pylori
Feces are examined using 2 methods: immunochromatography (detection of antigens) and PCR (presence of pathogen DNA). Both methods are characterized by high sensitivity and act as complementary methods.
Determination of antigens
Testing stool for Helicobacter pylori antigen is a qualitative method, the accuracy of which reaches 95%. Obtaining positive results 7 days after taking antibiotics indicates the ineffectiveness of treatment. A repeat test is carried out after 1.5 months of therapy, and the absence of antigens in the patient’s stool indicates complete destruction of the bacterium.
The method does not allow one to determine the type of bacteria: H. suis, H. Baculiformis or H. Pylori, since all their biomaterial is foreign (antigen) to humans.
Real-time PCR
The sensitivity of the stool PCR method for Helicobacter pylori infection reaches 95%. The analysis makes it possible to determine infection by unculturable forms of bacteria. Disadvantages include the possibility of obtaining false-positive results after a successful course of treatment, since destroyed bacterial cells (and their DNA) remain in the human body for a long time.
The possibility of obtaining false positive results is excluded, since the specificity of the method reaches 100%. The method is an alternative to the breath test or FGDS for young children.
No special preparation is required for collecting biomaterial for both studies. Feces are collected naturally without the use of laxatives, preferably before starting antibiotics.
Norm Helicobacter pylori in the blood in numbers
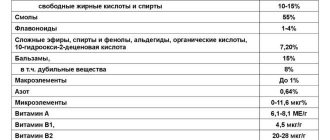
Decoding the blood test for Helicobacter pylori, as well as other data obtained, is the work of the doctor and does not allow the patient to independently interpret the results. The table shows normal values for each diagnostic technique.
| Method name | Norm | Approximate cost (for a private laboratory), rub. | Deadline for receiving results (excluding the day the biomaterial was taken) |
| Breath test | Less than 4 ‰ | 850 | Up to 6 days |
| PCR | Not detected | 500 | Up to 2 days |
| Antigens | 750 | 1 day | |
| Biopsy | 600 | ||
| Antibodies | IgG 0-0.9 IU/ml | 550 | |
| IgA 0 – 13.5 IU/ml | 650 | Up to 8 |
Patients are concerned about the question - what does Helicobacter negative mean? Obtaining such a result indicates the absence of Helicobacter pylori infection or successful therapy with complete destruction of bacteria.
Other research methods
Your doctor may order many other tests and procedures to help confirm the diagnosis:
- Physical examination.
During a physical examination, the gastroenterologist examines the abdomen to check for signs of bloating, abdominal wall tension, and pain. - Blood analysis.
The biomaterial is taken from a vein, the indication is a clear clinical picture of infection, everyday contact with the patient, and preventive measures. Blood samples are needed to look for antibodies against H. pylori. - Stool analysis.
Stool analysis is highly accurate (up to 95%). In order for a stool test to give a reliable result for the presence of Helicobacter, you must stop taking antibiotics before the test. - Endoscopic methods.
The most unpleasant examination option is examination with an endoscope. In this case, the doctor inserts a tube through the mouth into the stomach and duodenum. A camera attached to the end of the tube transmits images to a monitor. The method is quite accurate - the gastroenterologist can see ulcers and other changes on the mucous membrane and take tissue particles from their surface. But at the same time, this procedure is painful for patients, so it is better to resort to endoscopy in extreme cases, when you need to make sure that the process is benign.
If we compare all the tests for Helicobacter pylori, we can conclude that most of them do not have the proper accuracy, while the breath test gives a truly objective result. If we compare this analysis with an endoscopic examination, it is preferable for many people who do not want to endure nausea and discomfort during the examination.
The Helicobacter breath test is truly a wonderful alternative to outdated methods.
If you find an error, please select a piece of text and press Ctrl+Enter