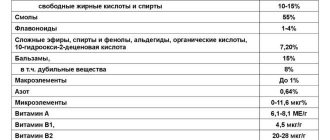
- The main side effects of the main drugs used in anti-Helicobacter therapy regimens
| Bismuth Tetracycline | Dark chair Dizziness Dizziness (vertigo; synonym - vertigo) is a term that is used to designate a distorted perception of the position of one’s body in space, a feeling of imaginary movement of one’s own body or the environment. For more information, see the article Dizziness. Increasing renal failure |
| Metronidazole | Pseudomembranous colitis Anorexia Anorexia (anorexia; an- + Greek orexis, desire to eat, appetite) is a lack of appetite in the presence of a physiological need for nutrition, caused by disturbances in the activity of the food center. There are several types of anorexia. Anorexia neurotic occurs when the cerebral cortex is overexcited, especially with negative emotions. Neurodynamic anorexia is caused by inhibition of the appetite center when exposed to extreme, for example, painful stimuli. Anorexia nervosa (A. nervous, nervous cachexia) is a persistent refusal to eat due to mental illness, accompanied by emaciation and other symptoms of starvation. Anorexia can be primary - with hypothalamic insufficiency in young children, Kanner's syndrome, depressive states, schizophrenia and secondary - with neurotic conditions, as well as due to prolonged restriction in food for the purpose of losing weight. Along with anorexia, hyporexia (decreased appetite), bulimia (see), as well as selective and perverted appetite (pica) are distinguished. Teturam-like reaction when taking alcohol |
| Amoxicillin | Diarrhea, candidiasis Pseudomembranous colitis |
| Clarithromycin | Diarrhea Pseudomembranous colitis |
The effectiveness of treatment for peptic ulcer disease is assessed by the disappearance of pain and dyspeptic syndromes, as well as by the dynamics of the endoscopic picture - scarring of the ulcer (with duodenal localization of the ulcer, endoscopic examination is carried out after 4 weeks, and with gastric localization after 8 weeks).
Treatment regimen for Helicobacter pylori
The drug treatment regimen for Helicobacter pylori has the only goal - to destroy the pathogenic bacterium and permanently cure the patient from this infection. Treatment regimens can be different, it all depends on the individual characteristics of the patient’s body and his general condition. It is important to undergo treatment under the strict supervision of a doctor; this is the only way to get rid of Helicobacter pylori infection and prevent relapses.
What determines the ineffectiveness of eradication?
Sometimes, during deep therapy of helibacteriosis, it is not possible to destroy pathogenic microorganisms. This is a consequence of the following errors:
- the use of medications that are not included in the developed treatment regimens or the prescription of incorrect doses;
- short therapeutic course;
- lack of laboratory control.
If you do not follow the prescribed dosages and do not adhere to bacteria eradication regimens, the risk of side effects increases. If you refuse to take medications, severe complications cannot be ruled out. Therefore, it is necessary to strictly follow all the instructions of the attending physician in order to get rid of unpleasant symptoms and avoid serious consequences.
Main causes
Helicobacter pylori is a pathogenic microorganism that has a spiral shape, lives outside the body, and upon penetration inside settles on the mucous walls of the stomach or the nearby duodenum. Helicobacter bacteria often enter the human body through household contact and through close interaction with the carrier of the bacteria. Even under conditions of high hydrochloric acid content, the microorganism does not die, but continues to actively develop and multiply.
If the analysis shows the presence of this bacterium in the human body, comprehensive and long-term treatment is necessary to help remove the pathogen. Otherwise, the patient risks developing chronic gastritis, polyposis, gastroduodenitis, ulcers and even stomach cancer.
How is the bacterium Helicobacter pylori transmitted?
The main cause of gastritis and ulcers is the bacterium Helicobacter pylori, which parasitizes and multiplies in the human body. The microbe is an anaerobic species, one that dies in the air. To avoid infection, every person should know where Helicobacter pylori comes from and how it is transmitted.
The risk of contracting the disease increases with close contact with a sick person. The infectious bacterium can be transmitted through shared utensils, kissing, or sexual intercourse. Gastroenterologists warn that timely treatment will help avoid serious complications and protracted illness.
Distinctive features of the bacterium
Helicobacter has adapted to survive in our body due to the presence of special flagella legs and enzymes that neutralize the hydrochloric acid secreted by the stomach. As a result, the protective mucus dissolves, which leads to the appearance of gastritis and ulcers.
Sad statistics show that a third of the world's population suffers from the disease. Scientists say that the ability of Helicobacter pylori to survive in an acidic environment has led to an increase in the number of gastrointestinal diseases. You can get rid of the microbe only with the help of special antibacterial therapy, which involves the use of antibiotics and vitamins.
Helicobacter pylori has distinctive features:
- The microorganism is the main cause of peptic ulcers. It is worth remembering the routes of infection with Helicobacteriosis. The proliferation of bacteria inevitably leads to the destruction of epigastric cells, releasing dangerous toxins. As a result, ulcers, gastritis, and inflammation of the duodenum appear.
- Helicobacter survives even in an acidic environment. This is not typical for other microorganisms that die under the influence of gastric juice.
- Diseases caused by Helicobacter pylori can only be treated with antibiotics.
In the absence of correct and timely treatment, the bacterium provokes the development of ulcers and subsequently oncological processes of the digestive organs.
Dangerous symptoms
The first signs of the disease begin to appear already on the 6th day after infection. You should be concerned if you feel:
- pain;
- nausea;
- burping;
- vomiting
Many patients do not pay attention to such symptoms, because pain and nausea go away after eating, and vomiting can be attributed to poisoning. If you notice the listed manifestations, immediately contact a gastroenterologist to receive timely therapy.
In the meantime, you do not take the alarm signals seriously, Helicobacter continues to live quietly and parasitize inside the stomach. If you are exposed to stress, abuse alcohol, or smoke, then this is even more conducive to the long-term existence of the microbe.
The disease is transmitted in the most unexpected way, even from pets.
Routes of infection
The harmful microorganism attacks the digestive tract, causing gastritis and ulcers. Even if you lead a healthy lifestyle and observe the principles of personal hygiene, this does not guarantee protection.
Full information about the routes of transmission of Helicobacter pylori is presented in the table.
Method of infection Brief description
| Airborne | It is impossible to become infected because the bacterium does not survive in the open air. However, if a healthy person is in close proximity to an infected person who is coughing or sneezing, then the likelihood of becoming infected with Helicobacter pylori increases hundreds of times. |
| Personal items | Someone else's toothbrush and even lipstick are provoking factors for infection. |
| Kiss | The bacterium is transmitted through mucous secretions or saliva, so you should only kiss with a regular partner. |
| Through animals | Despite the fact that humans are the main carrier of the pathogen, you can become infected through direct contact even with domestic animals - a cat or dog, as well as through contact with pigs, cows, and monkeys. |
| Sexually | During intercourse, the microbe is transmitted through saliva, which enters the body through oral and anal sex. To minimize the risk of pathogen penetration, do not forget about intimate hygiene and contraception. |
| Transplacental | The infection can be passed from mother to child. This is indicated by the fact that after the baby is born, antibodies to Helicobacter pylori are present in his blood. |
| Breast milk | Human milk is a kind of antibiotic, so the baby cannot pick up the bacteria during breastfeeding. |
| Water | The risk of infection increases if you drink contaminated liquid. Helicobacter can survive in liquid for up to 2 weeks. Therefore, try to use boiled, purified or purchased water, whose quality is beyond doubt. |
| Household way | The most common way a microbe enters the body. Shared dishes, towels, stationery, and that's not all. If a family has an infected member of the household, the likelihood of infecting others increases significantly. |
| Food | Contaminated food is one of the main factors for Helicobacter pylori disease. The bacterium is transmitted in places of public catering through food products: restaurants and cafes, the owners of which are negligent in the cleanliness of their catering unit. |
As you can see, you can catch a dangerous microbe almost anywhere. The infection is insidious in that it may not manifest itself until a certain moment (stress, illness).
The most effective method of prevention is personal hygiene.
At-risk groups
Scientists have long wondered about the routes of transmission and life activity of the bacterium. There is still no consensus about Helicobacter pylori infection and the need for treatment. Be that as it may, you need to get rid of the dangerous microbe, otherwise a mild form of gastritis will eventually develop into an ulcer.
Surely many are interested in the question of who is susceptible to helicobacteriosis in the first place.
Children
Most often, it is not adults who suffer from the disease, but the youngest patients. The bacterium is transmitted through contact with infected children, using dirty dishes, and failure to comply with personal hygiene rules. It should be remembered that the body of a child, especially an infant, does not yet have sufficient protection to resist pathogenic microbes, so it is very easy to infect it.
To avoid Helicobacter pylori disease in children, try to give your baby only clean fruits and berries and teach him good hygiene. If you notice that your little one has become capricious, holding his tummy and complaining of constant pain, make an appointment with a specialist.
To protect your baby from illness, monitor his well-being and the quality of the products you cook from.
With weakened immunity
Frequent stress, moral fatigue and family problems lead to a decrease in immunity, which is already a proven fact.
As is known, a person with low body defense is susceptible to infection by various pathogens. The bacterium Helicobacter pylori “loves” weakened areas and chooses just such for its existence.
It also happens that a person who is absolutely healthy at first glance suddenly falls ill with a stomach disease.
The disease can also be transmitted during gastroscopy or FGDS, surgery, if the instrument has not undergone sufficient treatment.
Family
Gastroenterologists agree that if there is at least one carrier of Helicobacter pylori in a family, then all other household members are also at risk of becoming infected. There are quite a few factors for familial infection:
- shared utensils;
- Houseware;
- often family members use the same towel for their hands and face;
- personal contact, such as kissing.
Experts also suggest that Helicobacter pylori is transmitted after close contact with pets. Pregnancy, infancy and weakened immunity of the epigastric mucosa are reasons why contact with pets should be avoided.
One version of infection with stomach bacteria is eating foods on which flies have sat.
In the dining room
Helicobacter pylori “loves” to live in public feeding areas. A person can become infected with it quite quickly by eating there. Typically, such places do not pay due attention to hygiene, and these are ideal conditions for the life of a pathogenic microorganism.
Using shared utensils, irregular cleaning, and failure to comply with food storage rules are the hallmarks of establishments where you are likely to “pick up” Helicobacter. Therefore, the best option is to eat at home to reduce the risk of infection.
Are stomach diseases transmitted?
The question of how gastrointestinal diseases are transmitted is of interest to many. Some believe that the routes of infection for gastritis and ulcers lie in poor diet and lack of hygiene, while others worry whether gastritis is transmitted genetically. But is it really that simple?
According to scientists, the most common causes of gastritis are stress and poor regular nutrition. They are the catalysts for the development of the disease with weak gastrointestinal immunity, which may just be hereditary.
If you suffer from a stomach ailment, learn to overcome exacerbations that occur in the autumn and spring. The ancient Chinese developed a unique technique aimed at combating pain. Judging by the reviews, this kind of charging really helps.
- Begin your exercise routine by methodically rubbing your palms together. This will help fill the body with energy.
- Place your hands on your lower abdomen, positioned on either side of your navel.
- Close your mouth and breathe in through your nose.
- Exhale slowly and imagine that you are lifting your stomach with your hands. Visually, the pose should resemble a crane standing on one leg.
- Inhale slowly, sticking your stomach out as much as possible.
- For the first time, limit yourself to 2-3 repetitions, gradually increasing their number to 12.
According to Eastern sages, the best time for classes is 7-9 am, when our biorhythms are in the most favorable position.
Only Helicobacter can be transmitted, which provokes gastritis in the presence of stimulating factors. These include, as mentioned above, stress and weak stomach immunity.
Canadian scientists have come up with an interesting hypothesis. They believe that 2 bananas a day are the best prevention of stomach ailments. The fruits contain substances that protect the inner wall of the epigastrium from damage and aggressive influences.
Re-infection
Unfortunately, secondary infection with Helicobacter pylori cannot be ruled out. However, before you ask this question, check whether you completely got rid of the bacteria the first time. To do this, you need to undergo a breath test and FGDS, which will determine the presence of a microorganism with one hundred percent probability.
How to avoid getting infected again after treatment is a question that interests many patients. According to statistics, only 3-5% of the world's population are re-infected.
If infection does occur, it is necessary to look for the reasons. One of them is weakened immunity of the gastric mucosa.
There is a high level of infection in the group of people who suffer from diabetes or have chronic helicobacteriosis.
Gastroenterologists recommend undergoing preventive examination for those who have managed to recover from the disease. A breath test should be performed 1.5-2 months after therapy.
Before diagnosis, contact your doctor so that he can prescribe a full range of tests.
Prevention
To effectively combat Helicobacter, it is not enough to be treated with antibiotics and other drugs. An important role in therapy is played by preventive measures that are aimed at recovery and prevention of re-infection. Basic Rules:
- Wash your hands before eating.
- Do not use dirty dishes, especially shared ones.
- Try to cut off or break off pieces rather than bite off, since a person with helicobacteriosis may have eaten the same product before you.
- Use only your own personal hygiene products.
- Do not drink from shared mugs or glasses.
- Avoid smoking and alcohol as it weakens the immune system.
If you have symptoms of Helicobacter pylori, you should undergo a medical examination annually. One of the best methods is to conduct an FGDS with taking a sample of gastric mucus. Such an examination will determine with one hundred percent probability the presence of a microbe in the body.
Now you know how gastritis is transmitted and what you need to do to avoid catching this disease and becoming infected with Helicobacter pylori. Lead a healthy lifestyle and practice good hygiene.
Source: https://gastrox.ru/live/helikobakter-pilori-kak-peredaetsya.html
Characteristic symptoms
With progressive helicobacteriosis in adults, the very first manifestation indicating infection is acute pain in the stomach, which intensifies after eating. This symptom indicates damage to the mucosa by erosions and ulcers. Another common symptom is severe heartburn and sour belching. The patient also experiences loss of appetite, intolerance to certain foods, frequent nausea and digestive problems. If such symptoms begin to bother you constantly, the usual medications do not bring relief, but, on the contrary, the situation worsens, you should not postpone a visit to the doctor, otherwise complications cannot be avoided.
Eradication
Indications
Anti-Helicobacter therapy is prescribed to patients whose tests for Helicobacter pylori have shown a positive result. In this situation, the patient may develop the following diseases:
- stomach and duodenal ulcers;
- atrophic gastritis;
- severe inflammatory complication of the entire stomach or certain areas;
- multiple formation of ulcers, erosions, polyps;
- high risk of cancer;
- MALT lymphoma of the stomach;
- reflux esophagitis;
- chronic form of gastritis or ulcerative pathology.
Return to contents
General principles
It is possible to get rid of Helicobacter forever and prevent relapses if the treatment regimen was prescribed correctly. The following simple rules will help you successfully deal with the problem:
Return to contents
How to treat?
For Helicobacter pylori treatment to be effective, the doctor prescribes medications that kill the infection and promote rapid healing of damaged mucous membranes. Standard drug treatment includes the following groups of drugs:
- Antibiotics. They destroy the bacteria, thanks to which the patient is cured, and the risk of relapse is minimized.
- Antacids. Recommended for patients with high acidity. Thanks to its enveloping properties, the medicine helps reduce inflammation and reduce acidity.
- Proton pump blockers and H2-histamine blockers. Reduces the production of hydrochloric acid.
Return to contents
Treatment regimens
To effectively cure an infection, modern medicine offers 2 schemes:
- Triple. The course of treatment is 7 days. Recommended drugs against Helicobacter pylori: Pariet - Clarithromycin - Amoxiclav.
- Quadruple quad therapy. Duration - 7 days. For treatment, the following drugs are prescribed: “Pariet” - preparations of bismuth salts - “Metronidazole” - “Tetracycline” - “Cifran”.
Return to contents
Proton pump inhibitor drugs (PPIs)
Modern drug treatment cannot do without the prescription of this group of pharmaceuticals, so they are necessarily included in the first and second line eradication therapy for Helicobacter pylori. The medicine selectively blocks the functioning of stomach cells that secrete hydrochloric acid. Due to this effect, the production of gastric juice is reduced, and the Helicobacter pylori bacterium stops multiplying. It also reduces the aggressive effect of hydrochloric acid on the affected stomach walls. As a result, erosions and ulcers heal faster and damaged structures regenerate. The list of recommended drugs is as follows:
Treatment for reduced susceptibility to Clarithromycin
Classic triple pattern
The first line includes the following types of treatment:
- Triple therapy, which lasts 7 days. In this case, the pathology is treated with the following drugs: PPI - Clarithromycin - Amoxiclav or Metronidazole. You can get the best effect from treatment if you double the PPI dose or take the medication for 14 days.
- Bismuth-containing quad therapy. Duration of therapy is from 10 to 14 days. The regimen includes medications: “De-nol” - “Tetracycline” - “Tinidazole” - PPI.
When treated with Denol, the development and reproduction of Helicobacter is inhibited, and it is effectively eliminated from the body.
Second line
If, after a course of treatment according to the 1st line regimen, there is no cure, the best one is prescribed:
- Quadruple therapy: bismuth subcitrate - Tetracycline tablets - Metronidazole - PPI. If Metronidazole is ineffective, it is replaced with McMiror, which kills the infection more effectively.
- Triple regimen: Levofloxacin - PPI - Amoxiclav.
Return to contents
Third line
If antiulcer therapy using the first and second lines is ineffective, a new, individual schedule is selected based on determining the sensitivity of Helicobacter to antibiotics. Often a reaction to Levofloxacin and Clarithromycin is determined. In case of increased sensitivity to the second drug, the most effective regimen looks like this:
- Triple, lasting 10-14 days: Amoxicillin - Clarithromycin - Tinidazole - PPI.
- If the reaction to Levofloxacin is positive, the regimen includes the drug of the same name, Amoxicillin tablets and PPIs. The duration of treatment is 14 days.
Return to contents
With increased resistance to Clarithromycin
First line
- Bismuth-based quadruple therapy lasting 10-14 days: “Tetracycline” - “Metronidazole” - PPI “Nolpaza”.
- 1-5 days: “Amoxiclav” - PPI;
- PPI - Amoxicillin - Clarithromycin - Tinidazole.
Second line
If there is no improvement after using the first line, a triple regimen is used, lasting 10-14 days. Medicines used:
Adverse reactions during treatment
It will take a long time to treat and kill Helicobacter with medication, so the pills taken can negatively affect the patient’s general health, causing negative consequences, the most common of which are:
- allergy;
- dyspepsia;
- nausea, vomiting, indigestion;
- dysbiosis.
To ensure that the treatment of gastritis brings a minimum of side effects, and the drugs that kill the infection have less impact on the functioning of the intestines, the antidiarrheal drug “Hilak Forte” is prescribed. The best remedy that normalizes the microflora of the rectum is Enterol and Bifiform drops. It will be possible to reduce the acidity of the stomach if you regularly drink Phosphalugel.
The latest developments for the destruction of Helicobacter pylori
Modern medical microbiology has developed unique bacteriophage viruses that destroy pathogenic bacteria and microorganisms, for example, staphylococci, streptococci, E. coli, Helicobacter, and even lamblia and roundworms. To treat these pathologies, it is not a living bacteriophage that is used, but its enzymes, which negatively affect microorganisms and destroy them. These microbiological elements are considered the drugs of the future. They are able to cure helicobacteriosis, staphylococcus, and giardiasis without harm to the body.
Colloidal silver has long been considered a universal antimicrobial agent, its destructive effect on pathogens has been proven by traditional medicine. An aqueous solution of silver ions is often prescribed to patients diagnosed with chronic gastritis. After taking this drug, patients note an improvement in their condition and a decrease in accompanying symptoms.
Joint effect
The bacterium Helicobacter pylori, responsible for HP-associated forms of gastrointestinal diseases, quickly develops resistance to antibiotics. The likelihood that microorganisms will become resistant to several active substances at once decreases several times.
Clarithromycin in combination with Amoxicillin is able to quickly suppress the growth and reproduction of bacteria by expanding the spectrum of action and different ways of influencing the pathogen. The triple eradication regimen must include proton pump inhibitors - Omeprazole or its analogues. Amoxicillin can be replaced with Metronidazole.
Amoxicillin is a penicillin antibiotic that has a wide medicinal spectrum.
Helicobacter Pylori eradication therapy
Marina Pozdeeva about the principles and schemes of anti-Helicobacter therapy
Colonization of Helicobacter pylori on the surface and folds of the gastric mucosa significantly complicates antibacterial therapy. Successful treatment is based on a combination of drugs that prevent the emergence of resistance and overtake the bacteria in different parts of the stomach. Therapy must ensure that even a small population of microorganisms does not remain viable.
Helicobacter pylori eradication therapy includes a complex of several drugs. A common mistake that often leads to unpredictable results is replacing even one well-studied drug from a standard regimen with another drug from the same group.
When is mandatory treatment required?
If you suspect Helicobacter, you should immediately contact a gastroenterologist. In the absence of inflammation in the gastric mucosa and positive diagnostic tests, treatment of the bacteria is not carried out. Treatment of Helicobacter with modern antibiotics is necessary in cases of suspected:
- ulcer requiring immediate surgical intervention;
- benign, malignant tumors of the gastrointestinal tract;
- lymphoma;
- chronic heartburn;
- severe forms of gastritis;
- atrophy of the gastric mucosa.
Proton pump inhibitors (PPIs)
PPI therapy has proven effective in various clinical studies. Although PPIs have a direct antibacterial effect on H. pylori in vitro, they do not play an important role in eradicating the infection.
The mechanism by which PPIs synergize when combined with antimicrobials to enhance the clinical efficacy of eradication therapy has not been fully established. It is assumed that antisecretory drugs of the PPI group may help increase the concentration of antimicrobial agents, in particular metronidazole and clarithromycin, in the gastric lumen. PPIs reduce the volume of gastric juice, as a result of which the leaching of antibiotics from the surface of the mucosa decreases, and the concentration, accordingly, increases. In addition, reducing the volume of hydrochloric acid maintains the stability of antimicrobials.
Bismuth preparations
Bismuth was one of the first drugs to eradicate H. pylori. There is evidence that bismuth has a direct bactericidal effect, although its minimum inhibitory concentration (MIC - the smallest amount of drug that inhibits the growth of a pathogen) against H. pylori is too high. Like other heavy metals such as zinc and nickel, bismuth compounds reduce the activity of the enzyme urease, which is involved in the life cycle of H. pylori. In addition, bismuth preparations have local antimicrobial activity, acting directly on the bacterial cell wall and disrupting its integrity.
Metronidazole
H. pylori is generally very sensitive to metronidazole, the effectiveness of which is independent of pH. After oral or infusion use, high concentrations of the drug are achieved in the gastric juice, which makes it possible to achieve the maximum therapeutic effect. Metronidazole is a prodrug that undergoes activation by bacterial nitroreductase during metabolism. Metronidazole causes H. pylori to lose its helical DNA structure, causing DNA damage and killing the bacterium.
Clarithromycin
Clarithromycin, a 14-member macrolide, is a derivative of erythromycin with a similar spectrum of activity and indications for use. However, unlike erythromycin, it is more acid resistant and has a longer half-life. The results of studies showing that the triple eradication therapy regimen for Helicobacter pylori using clarithromycin gives a positive result in 90% of cases, led to the widespread use of the antibiotic.
In this regard, an increase in the prevalence of clarithromycin-resistant strains of H. pylori has been recorded in recent years. There is no evidence that increasing the dose of clarithromycin will overcome the problem of antibiotic resistance to the drug.
Indications for eradication therapy
According to the Maastricht 2-2000 Consensus Report, H. pylori eradication is strongly recommended:
- all patients with peptic ulcer disease;
- patients with poorly differentiated MALT lymphoma;
- persons with atrophic gastritis;
- after resection for gastric cancer;
- first-degree relatives of patients with stomach cancer.
The need for eradication therapy in patients with functional dyspepsia, GERD, as well as in persons taking non-steroidal anti-inflammatory drugs for a long time remains a subject of debate. There is no evidence that eradication of H. pylori in such patients affects the course of the disease. However, it is well known that individuals with H. pylori who have nonulcer dyspepsia and corpus-predominant gastritis are at increased risk of developing gastric adenocarcinoma. Thus, H. pylori eradication should also be recommended for patients with nonulcer dyspepsia, especially if histology reveals corpus-predominant gastritis.
The argument against anti-Helicobacter therapy in patients taking NSAIDs is that the body protects the gastric mucosa from the damaging effects of drugs by increasing cyclooxygenase activity and prostaglandin synthesis, while PPIs reduce natural defenses. However, eradication of H. pylori before prescribing NSAIDs significantly reduces the risk of peptic ulcer disease during subsequent treatment (a study by American scientists led by Francis K. Chan, published in The Lancet in 1997).
Indications for simultaneous use
The combination of drugs is used to treat infections of various locations caused by the following microorganisms:
- streptococcus;
- salmonella;
- staphylococcus;
- chlamydia;
- coli.
Both antibiotics destroy microorganisms susceptible to their composition, and when interacting, they strengthen each other.
The combination is prescribed for the following pathologies:
- gastroduodenal diseases of a bacterial nature: peptic ulcer, chronic gastritis, stomach cancer;
- respiratory tract infections;
- skin bacterial lesions;
- tuberculosis.
Combination therapy is especially indicated for chronic forms of diseases that cannot be treated with one medication.
Clarithromycin is a semisynthetic antibiotic from the macrolide group that has a bacteriostatic effect.
The combination of Clarithromycin-Amoxicillin-Omeprazole is the best treatment regimen for the eradication of Helicobacter pylori, leading to cure in 85-95% of cases. The complex drug Pilobact AM based on 3 substances was created specifically for the treatment of Helicobacter-related diseases.
Eradication therapy
Despite the use of combination treatment regimens, 10–20% of patients infected with H. pylori fail to achieve elimination of the pathogen. The best strategy is to select the most effective treatment regimen, but the possibility of using two or even more sequential regimens should not be ruled out if the treatment of choice is insufficiently effective.
If the first attempt at eradication of H. pylori fails, it is recommended to immediately proceed to second-line therapy. Antibiotic sensitivity testing and switching to salvage therapy regimens are indicated only for those patients in whom second-line therapy will also not lead to eradication of the pathogen.
One of the most effective “rescue regimens” is a combination of PPI, rifabutin and amoxicillin (or levofloxacin 500 mg) for 7 days. An Italian study led by Fabrizio Perri and published in Alimentary Pharmacology & Therapeutics in 2000 confirmed that the rifabutin regimen was effective against strains of H. pylori resistant to clarithromycin or metronidazole. However, the high price of rifabutin limits its widespread use.
Research data confirm that a 10-day salvage therapy regimen, including rabeprazole, amoxicillin and levofloxacin, is much more effective than standard second-line eradication therapy (a study by Italian scientists led by Enrico C Nista, published in Alimentary Pharmacology & Therapeutics in 2003 year).
Found a mistake? Select the text and press Ctrl+Enter.
Third line
The regimen involves the simultaneous use of two antibiotics and any drug from the group of proton pump inhibitors (PPIs) or (PPI) pumps. Their actions are aimed at reducing the formation of gastric juice.
The scheme may vary depending on the habituation of the bacteria stamp to the medicines and the inability of the patient’s body to accept the medicine. The following options exist:
- They take clarithromycin (500 mg 2 times a day) and amoxicillin (500 mg 4 times a day), PPI medication (20 mg twice a day).
- Use of clarithromycin (500 mg twice a day), amoxicillin (500 mg 4 times a day), PPI (20 mg 2 times a day), De-nol (240 mg twice a day).
- The PPI drug is not taken, De-Nol and antibiotics are left in the same doses.
- This option is used for elderly patients if the standard regimen is not possible. Gentle treatment is used: amoxicillin at a dosage of 0.1 g twice a day, De-nol 120 mg 4 times a day, a PPI (lansoprazole, pantoprazole or another) 20-40 mg twice a day.
Treatment of the microbe Hilary Bacter pylori lasts 7-14 days. The duration of the therapeutic course depends on the stage of the lesion, symptoms and other factors.
When previous methods are ineffective, four-component options are used. The duration of the therapeutic course reaches two weeks.
The options are as follows:
- Tripotassium bismuth dicitrate (4 doses of 120 mg daily), PPI, tetracycline (4 doses of 500 mg), metronidazole (500 mg, 3 doses).
- De-nol (240 mg 2 times), amoxicillin (500 mg 4 times), PPI, nitrofuran medicine.
- Amoxicillin (500 mg 4 times), PPI, bismuth subcitrate (120 mg 4 times), rifaximin (400 mg twice).
When previous methods do not help, antibiotics for Helictobacter are taken as a third line of therapy. The individual regimen is based on the use of colloidal bismuth subcitrate (De-nol). The bacteria's susceptibility to certain medications is first studied. De-nol is used for Helicobacter pylori precisely because the pathogen is not able to adapt to it.
De-nol forms a protective film on the surface of the digestive organs, preventing the effects of aggressive factors. In addition, it reduces acidity, increases the production of protective mucus, and promotes scarring of ulcers.
Helicobacter pylori, is it so scary?
Helicobacter pylori is a microorganism that is transmitted orally, lives in approximately 50% of people, but does not cause clinical manifestations in everyone.
In most people, this infection is completely asymptomatic, does not cause clinical manifestations, and therefore does not require diagnosis and further treatment.
But in a certain part of the population it causes inflammation of the mucous membrane of the stomach and duodenum, up to the formation of atrophic and metaplastic changes in them, thus being one of the main factors in the development of peptic ulcers of these organs.
Data on the association of Helicobacter pylori with the development of other diseases (mucosal tissue lymphomas, inflammation of the coronary arteries, gastroesophageal reflux disease (GERD), iron deficiency anemia, some skin and rheumatological diseases) currently remain insufficiently substantiated, and debate to confirm or refutations of this cause-and-effect relationship remain open.
There are many different studies confirming a clear connection between H. pylori infection and the development of gastric and duodenal ulcers (the first data were obtained back in 1983).
Peptic ulcer of the stomach and duodenum is one of the most common diseases of the digestive system - up to 15% of pathologies of the gastrointestinal tract.
According to data from different countries, peptic ulcer disease affects from 2.9% to 10% of the adult population; its main clinical manifestation is the formation of a fairly persistent ulcerative defect in the wall of the stomach and/or duodenum.
Helicobacter pylori has unique microbiological characteristics that allow it to alkalize the environment in the stomach, thereby causing an increase in the secretion of hydrochloric acid, as well as a decrease in the secretion of bicarbonate (alkali) in the duodenum, thus disrupting the acid-base balance in both the stomach and duodenum intestine, due to which the microorganism further colonizes the mucous membrane, forms its increased susceptibility to hydrochloric acid, and inflammation begins in the mucous membrane, which subsequently leads to the development of ulcerative defects.
Symptoms that suggest H. Pylori infection include pain in the upper left and center abdomen, in the umbilical area, pain may occur on an empty stomach and go away after eating, or occur after a certain time after eating (after 30-60 minutes, or after one and a half to two hours), heartburn, belching, bad breath, bloating, a feeling of heaviness in the stomach after eating, stool disorders.
But it should be remembered that these symptoms can be caused by other diseases of the stomach and duodenum, or other organs.
What antibiotics are used?
Initially, scientists identified more than 20 drugs that successfully deal with the microbe. However, as studies have shown, many of them lose activity under the influence of hydrochloric acid. And only 7 medications were approved by the Ministry of Health.
The list includes the following:
- tetracycline;
- azithromycin;
- tinidazole;
- levofloxacin;
- amoxicillin (flemoxin);
- clarithromycin;
- Metronidazole.
Treatment of helicobacteriosis is prescribed by the doctor after a complete examination of the patient. Therefore, you should not immediately buy all the medications from the above list. Perhaps the specific situation does not require the use of antibacterial agents. Many patients live with the microbe for many years without feeling any symptoms.
Diagnostics
Various methods are used to diagnose H. Pylori infection. The greatest diagnostic significance is the determination of the antigen (but not the determination of DNA!) in the stool, a breath test with C-13 radioactive carbon-labeled urea; to detect a primary infection, a serological method is used - determination of class G immunoglobulins in the blood (the method cannot be used to evaluate the treatment performed! ).
The determination of H. Pylori in a mucosal biopsy is also used during an endoscopic examination of the stomach and duodenum (the absence of a microorganism in the material taken does not indicate the absence of infection, since it could be taken from points of the mucosa where there is no H. Pylori, but, for example , at 3 centimeters it is already there).
Should not be used for diagnosis: various breath tests that do not use urea labeled with radioactive carbon C-13, determination of H. Pylori DNA in stool, stool culture for Helicobacter, determination of Helicobacter in scrapings from the tongue, as well as other unreliable diagnostic methods.
Treatment regimen for Helicobacter pylori
The drug treatment regimen for Helicobacter pylori has the only goal - to destroy the pathogenic bacterium and permanently cure the patient from this infection. Treatment regimens can be different, it all depends on the individual characteristics of the patient’s body and his general condition. It is important to undergo treatment under the strict supervision of a doctor; this is the only way to get rid of Helicobacter pylori infection and prevent relapses.
Basic eradication schemes
Treatment regimens for Helicobacter pylori were approved at the Maastricht conference. Two lines of therapy have been developed. The first of them is the main one, the so-called “Gold Standard”. The second line is an alternative option, which is appropriate to use if the first line is low in effectiveness.
Both regimens involve taking antibiotics and proton pump inhibitors. The role of antibiotics is the rapid eradication of Helicobacter pylori. These drugs block cell wall synthesis and prevent the formation of colonies of microorganisms. They are effective even in conditions of high acidity.
Proton pump inhibitors (PPIs) are medications that regulate pH levels in the digestive system. Their task is to suppress the excessive secretion of hydrochloric acid by stomach cells. The active substances of the drugs block the process of transfer of hydrogen cations. As a result, the environment inside the gastrointestinal tract becomes less aggressive.
Triple therapy
The first line of treatment is the use of a three-part regimen. According to studies, this combination is effective in 80% of cases of treatment of gastritis, duodenitis or peptic ulcer at an early stage. This technique involves the appointment:
- Amoxicillin at a dosage of 1000 mg for 7 days;
- Clarithromycin at a dosage of 500 mg for 7 days;
- a drug from the PPI group in the dosage specified in the instructions - for 7 days.
This eradication scheme has its own nuances. So, Amoxicillin can be replaced with another antibiotic - Metronidazole at a dosage of 500 mg. The choice of proton pump inhibitors is wide. Omeprazole, Pantoprazole, Rabeprazole or Lansoprazole are prescribed. Their operating principle is the same. The minimum duration of therapy is 1 week, but if large Helicobacter pylori colonies form inside the digestive system, it is recommended to increase the treatment period to 10-14 days.
Quadruple therapy
An alternative treatment option is an expanded regimen of 4 components, including not only antibiotics and agents for normalizing acidity, but also bismuth-based drugs that have a complex effect.
The duration of four-component therapy is at least 10 days.
To completely get rid of Helicobacter pylori, patients are prescribed the following drugs:
- Tetracycline at a dosage of 500 mg;
- Metronidazole at a dosage of 500 mg;
- bismuth subsalicylate at a dosage of 120 mg;
- PPI in standard dosage.
If the second line of therapy also does not produce an effect, switch to treatment using fluoroquinolones. This is a group of drugs with pronounced antimicrobial activity. They differ from antibiotics in their chemical structure and origin. Fluoroquinolones are completely synthetic substances and have no natural analogues.
Main causes
Helicobacter pylori is a pathogenic microorganism that has a spiral shape, lives outside the body, and upon penetration inside settles on the mucous walls of the stomach or the nearby duodenum. Helicobacter bacteria often enter the human body through household contact and through close interaction with the carrier of the bacteria. Even under conditions of high hydrochloric acid content, the microorganism does not die, but continues to actively develop and multiply. If the analysis shows the presence of this bacterium in the human body, comprehensive and long-term treatment is necessary to help remove the pathogen. Otherwise, the patient risks developing chronic gastritis, polyposis, gastroduodenitis, ulcers and even stomach cancer.
Characteristic symptoms
With progressive helicobacteriosis in adults, the very first manifestation indicating infection is acute pain in the stomach, which intensifies after eating. This symptom indicates damage to the mucosa by erosions and ulcers. Another common symptom is severe heartburn and sour belching. The patient also experiences loss of appetite, intolerance to certain foods, frequent nausea and digestive problems. If such symptoms begin to bother you constantly, the usual medications do not bring relief, but, on the contrary, the situation worsens, you should not postpone a visit to the doctor, otherwise complications cannot be avoided.
Eradication
Indications
Anti-Helicobacter therapy is prescribed to patients whose tests for Helicobacter pylori have shown a positive result. In this situation, the patient may develop the following diseases:
- stomach and duodenal ulcers;
- atrophic gastritis;
- severe inflammatory complication of the entire stomach or certain areas;
- multiple formation of ulcers, erosions, polyps;
- high risk of cancer;
- MALT lymphoma of the stomach;
- reflux esophagitis;
- chronic form of gastritis or ulcerative pathology.
Return to contents
General principles
It is possible to get rid of Helicobacter forever and prevent relapses if the treatment regimen was prescribed correctly. The following simple rules will help you successfully deal with the problem:
- If auxiliary drugs and the prescribed antibiotic do not affect the life of the bacterium in any way, and it continues to multiply, it is necessary to immediately change the treatment regimen.
- If modern drugs for the treatment of helicobacteriosis are powerless and not a single approved regimen is effective, the sensitivity of the disease strain to the entire spectrum of antibacterial drugs is checked.
- If a year after the patient was able to completely recover, a re-infection occurs, this is considered a relapse and not a reinfection.
- In case of relapses, stronger medications are selected with each subsequent regimen.
Return to contents
How to treat?
For Helicobacter pylori treatment to be effective, the doctor prescribes medications that kill the infection and promote rapid healing of damaged mucous membranes. Standard drug treatment includes the following groups of drugs:
- Antibiotics. They destroy the bacteria, thanks to which the patient is cured, and the risk of relapse is minimized.
- Antacids. Recommended for patients with high acidity. Thanks to its enveloping properties, the medicine helps reduce inflammation and reduce acidity.
- Proton pump blockers and H2-histamine blockers. Reduces the production of hydrochloric acid.
Return to contents
Treatment regimens
To effectively cure an infection, modern medicine offers 2 schemes:
- Triple. The course of treatment is 7 days. Recommended drugs against Helicobacter pylori: Pariet - Clarithromycin - Amoxiclav.
- Quadruple quad therapy. Duration - 7 days. For treatment, the following drugs are prescribed: “Pariet” - preparations of bismuth salts - “Metronidazole” - “Tetracycline” - “Cifran”.
Return to contents
Proton pump inhibitor drugs (PPIs)
Modern drug treatment cannot do without the prescription of this group of pharmaceuticals, so they are necessarily included in the first and second line eradication therapy for Helicobacter pylori. The medicine selectively blocks the functioning of stomach cells that secrete hydrochloric acid. Due to this effect, the production of gastric juice is reduced, and the Helicobacter pylori bacterium stops multiplying. It also reduces the aggressive effect of hydrochloric acid on the affected stomach walls. As a result, erosions and ulcers heal faster and damaged structures regenerate. The list of recommended drugs is as follows:
Treatment for reduced susceptibility to Clarithromycin
Classic triple pattern
The first line includes the following types of treatment:
- Triple therapy, which lasts 7 days. In this case, the pathology is treated with the following drugs: PPI - Clarithromycin - Amoxiclav or Metronidazole. You can get the best effect from treatment if you double the PPI dose or take the medication for 14 days.
- Bismuth-containing quad therapy. Duration of therapy is from 10 to 14 days. The regimen includes medications: “De-nol” - “Tetracycline” - “Tinidazole” - PPI.
When treated with Denol, the development and reproduction of Helicobacter is inhibited, and it is effectively eliminated from the body.
Second line
If, after a course of treatment according to the 1st line regimen, there is no cure, the best one is prescribed:
- Quadruple therapy: bismuth subcitrate - Tetracycline tablets - Metronidazole - PPI. If Metronidazole is ineffective, it is replaced with McMiror, which kills the infection more effectively.
- Triple regimen: Levofloxacin - PPI - Amoxiclav.
Return to contents
Third line
If antiulcer therapy using the first and second lines is ineffective, a new, individual schedule is selected based on determining the sensitivity of Helicobacter to antibiotics. Often a reaction to Levofloxacin and Clarithromycin is determined. In case of increased sensitivity to the second drug, the most effective regimen looks like this:
- Triple, lasting 10-14 days: Amoxicillin - Clarithromycin - Tinidazole - PPI.
- If the reaction to Levofloxacin is positive, the regimen includes the drug of the same name, Amoxicillin tablets and PPIs. The duration of treatment is 14 days.
Return to contents
With increased resistance to Clarithromycin
First line
- Bismuth-based quadruple therapy lasting 10-14 days: “Tetracycline” - “Metronidazole” - PPI “Nolpaza”.
- 1-5 days: “Amoxiclav” - PPI;
- PPI - Amoxicillin - Clarithromycin - Tinidazole.
What antibiotics kill Helicobacter pylori
Antibacterial drugs are the “heavy artillery” that forces the bacteria to desert and leave the patient’s body.
The standards for the treatment of Helicobacter-associated gastric pathologies indicate at least two antibiotics. With significant contamination of the mucous membrane and pronounced clinical manifestations of the disease, it is impossible to do without them.
What antibiotics are recommended to take for Helicobacter pylori:
- Amoxicillin
- Clarithromycin
- Tetracycline
- Metronidazole
- Rifambutin
- Levofloxacin
Rifambutin and levofloxacin are “reserve” drugs; they are not included in standard treatment regimens, but can be used if pathogenic strains develop resistance to common drugs included in the protocols.
Antibacterial drugs have side effects: allergic reactions, dysbacteriosis, candidiasis, nausea. Patients are often afraid to take antimicrobial drugs precisely for this reason.
If you are infected with Helicobacter and have gastric diseases, you should not do this. Taking antibiotics in this case is justified.
Without these medications, the patient runs the risk of developing a stomach ulcer, and by refusing treatment, he exposes the body to the risk of developing oncopathology of the gastrointestinal tract. Stomach cancer is 3-6 times more likely to occur in patients infected with H. pylori who have not received proper therapy.
How to treat Helicobacter pylori with antibiotics - eradication therapy regimens
Today, 3- and 4-component treatment regimens aimed at destroying the bacteria have been developed and are actively used.
If a patient has a microbe in the stomach, there are symptoms of gastrointestinal damage, and the person has not previously received treatment, therapy is always started with a three-component regimen, which includes:
- Proton pump blocker (omeprazole, lansoprazole, rabeprazole, pantoprazole 20 mg) 2 times a day
- Amoxicillin 1000 mg 2 times a day
- Clarithromycin 500 mg 2 times a day
A 3-component regimen is prescribed when a patient first seeks treatment; elderly, debilitated patients can be individually adjusted to the dosage of medications.
This therapy is prescribed for 7 (minimum) to 14 days. Clinical studies have shown that in some cases, taking drugs for a week is not enough to ensure eradication, and therapy is ineffective.
After two weeks of taking the drugs, on the contrary, the effect of treatment was an order of magnitude higher: in a much larger number of patients, eradication of the pathogen reached 80% or more.
Four-component treatment regimen
If the effect of the 3-component regimen is not achieved, the destruction of the infectious agent has not occurred, the doctor will recommend continuing therapy after a month and a half, consisting of:
- Proton pump blocker (omeprazole, lansoprazole, rabeprazole, pantoprazole 20 mg) 2 times a day
- Preparations of bismuth salts 120 mg 4 times a day
- Metronidachol 500 mg 3 times a day
- Tetracycline 500 mg 4 times a day
This is a 4-component eradication scheme. It is important to ensure that previously used antibacterial drugs are not repeated. If resistance to the above antibiotics is detected, “reserve” medications can be prescribed: levofloxacin, rifambutin.
Despite the developed standards, the doctor, when carrying out eradication, must approach each case and disease individually, taking into account the patient’s age, concomitant pathologies, possible allergic reactions of the body and the resistance of specific strains of bacteria to drugs.
How many days to take antibiotics for Helicobacter pylori
A 3-component regimen is prescribed by a doctor for a period of 7 to 14 days. It is not advisable to take the drugs for less than a week; there will be no effect from such treatment.
The bacterium is difficult to treat and develops resistance to drugs, so more and more evidence is emerging that even a week is not enough to achieve a positive result and get rid of the pathogen. More and more doctors are inclined to extend antibiotic therapy to 10-14 days.
A weekly course of administration is recommended for elderly and weakened patients who have concomitant multiple organ pathologies and who find it difficult to tolerate a load of two antibiotics.
The 4-component regimen is prescribed for a period of two weeks.
The effectiveness of treatment should be assessed using diagnostic and laboratory methods no earlier than 1-1.5 months from the end of taking the drugs.
If eradication is 80% or more of the initial level, or no bacteria are found in the body at all, we can talk about success in treating the disease associated with this pathogen.