What is Crohn's disease?
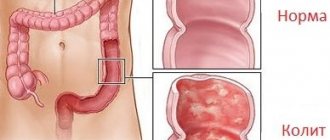
Crohn's disease is a chronic inflammatory bowel disease of an autoimmune nature.
In this case, all parts of the gastrointestinal tract can be affected, from the oral mucosa to the rectum and anus. The disease occurs everywhere, but residents of North America and Europe are most often affected. Recently, there has been an increase in the number of cases, especially in developing countries.
In Europe, the incidence of Crohn's disease reaches 5-6 cases per 100 thousand people.
Characteristic manifestations of the disease include abdominal pain and diarrhea, and the appearance of blood in the stool. Treatment of Crohn's disease includes therapy with anti-inflammatory drugs, antibiotics, and often surgery.
Causes
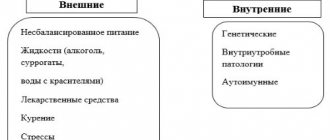
Crohn's disease (CD) develops when the immune system begins to attack the body's own tissues - the intestines and other digestive organs. However, the exact cause of the disease is unknown. There are several groups of factors that may be involved in the development of the disease:
- hereditary factors (if Crohn's disease is present in family members, the risk of the disease in relatives increases);
- genetic factors (in particular, mutation of the NOD2 gene, responsible for the synthesis of proteins involved in the work of innate immunity);
- infections (the influence of some bacteria and viruses on excessive activation of the immune response is assumed);
- immunological factors (directly, disorders of the immune system).
Additional risk factors may include:
- age (Crohn's disease often manifests itself before 30 years of age);
- excessive intake of non-steroidal anti-inflammatory drugs (NSAIDs), combined oral contraceptives (COCs);
- smoking;
- errors in diet.
Is Crohn's disease contagious?
Crohn's disease occurs due to a malfunction of the immune system. It's not contagious. However, if the disease is present in close relatives, the disease may manifest itself due to a hereditary factor.
Classification
Despite the fact that Crohn's disease can affect any part of the digestive system, there are several most common locations:
- ileocolitis (damage to the ileum and colon) - 42% of cases;
- ileitis (damage to the ileum) - 33%;
- colitis (colon damage) - about 20% of cases.
Additionally, isolated damage to the small intestine, damage to the anal area and multiregional inflammation involving the upper gastrointestinal tract (stomach, etc.) - 5% - are distinguished.
On the website msdmanuals.com you can independently calculate the degree of activity of Crohn's disease by assessing the presence of certain symptoms and complications.
Short description
Crohn's disease is a nonspecific inflammatory lesion of various parts of the gastrointestinal tract of unknown etiology, characterized by segmentation, a recurrent course with the formation of inflammatory infiltrates and deep longitudinal ulcers, often accompanied by complications. Depending on the affected part of the gastrointestinal tract, small intestinal, colonic and mixed forms of the disease are distinguished. Frequency: 25–27 cases per 100,000 population. Small intestinal form - 25% of cases, large intestinal form - 25%, mixed form - 50%. In the small intestine, the most common location (90%) is the terminal ileum, which explains the outdated name of this disease - terminal ileitis. Predominant age. The first peak of incidence is 12–30 years, the second is about 50 years. International classification of diseases ICD-10 code: K50 Crohn's disease [regional enteritis]
How dangerous is the disease? Complications
Crohn's disease is dangerous due to its complications (Fig. 1), including:
- Thickening of the intestinal wall, and as a result, narrowing of the intestine (narrowing of part of the intestine due to inflammation and the formation of scar tissue). Often makes it difficult to pass stool. In severe cases, intestinal obstruction may occur, which is manifested by pain and bloating, nausea and vomiting. In the future, the stricture can develop into stenosis - complete closure of the intestinal lumen.
- An anal fissure is a break in the lining of the intestine that can cause pain and bleeding.
- Intestinal perforation is a through defect that forms in the intestinal wall due to inflammation, cracks, or ulcers. Through this hole, intestinal contents leak into the abdominal cavity, which leads to the development of peritonitis, a condition requiring immediate surgery.
- Fistula - is formed when, as a result of inflammation, a through channel is formed between the intestine and a nearby organ or skin, through which intestinal contents are released into another organ or out.
- An abscess is a limited purulent inflammation that can be located near the intestinal wall, in the abdominal cavity, or in the tissues in the rectal area.
- Cancer—The risk of developing colorectal cancer in people with inflammatory bowel disease depends on how long the disease has lasted and how far it has spread in the colon. To diagnose colon cancer, a colonoscopy with biopsy is performed.
Figure 1. Diagram of complications of Crohn's disease. Source: propionix. ru
Crohn's disease during pregnancy
According to research, the effect of Crohn's disease on the course and outcome of pregnancy is determined by the activity of the disease at the time of conception and during pregnancy.
Complications include premature birth, miscarriages, and fetal development disorders. It is believed that with highly active Crohn's disease, the percentage of uncomplicated pregnancies is only 54%, while with inactive disease it is 80%. Thus, in the active phase of the disease, the risk of premature birth increases by 3.5 times, spontaneous miscarriages - by 2 times. With this disease, artificial termination of pregnancy and cesarean section are often performed.
Regarding the influence of pregnancy itself on the course of Crohn's disease, it is worth noting that when at the time of pregnancy the disease is in remission, then in 2/3 of cases remission remains during pregnancy. The frequency of exacerbations does not differ from non-pregnant patients. Exacerbations often develop in the first trimester of pregnancy, after abortion and after childbirth. Also, relapses often occur as a result of women refusing to take medications during pregnancy.
Complications
Progression of the disease - an increase in existing and the appearance of new areas of intestinal damage. Relapse of the disease after surgical treatment (often damage to the proximal intestine occurs). Fistulas occur in 15% of patients: rectum and anal canal, intestinal-vaginal, intestinal-vesical, interintestinal and external, coming from various parts of the gastrointestinal tract. Extraintestinal lesions occur in 10% of cases (erythema nodosum and pyoderma, episcleritis, uveitis, ankylosing spondylitis). Intestinal obstruction occurs in approximately 25% of cases. Extensive involvement of the colon increases the risk of developing adenocarcinoma. Perforation of the colon and profuse intestinal bleeding. Formation of infiltrates of different localization in the abdominal cavity. Acute toxic dilatation of the colon. Crohn's disease can lead to malabsorption due to mucosal damage, multiple strictures with bacterial overgrowth, or due to multiple bowel resections.
Pathogenesis
Crohn's disease develops when, under the influence of various factors (hereditary predisposition and genetic mutations, microbial activity and disorders of the immune system), an inflammatory response from the immune system is activated. The action of the immune system leads to damage to the intestinal wall. At the same time, a distinctive feature of the disease is the occurrence of ulcers affecting the entire thickness of the intestinal wall.
Over time, the intestinal mucosa takes on the characteristic appearance of a “cobblestone pavement” - areas of ulcers and cracks alternate with areas of accumulation of immune cells and swelling of the mucous membrane (Fig. 2).
Figure 2. Cobblestone-like changes in the intestinal mucosa in Crohn's disease. Source: aboutkidshealth ca Source: unspecific. ru.
Crohn's disease in adults
Crohn's disease is considered a disease of the young - it affects mainly middle-aged people, with the peak incidence occurring between 15 and 35 years of age. Among the older age group, a second peak is observed - after 60 years.
At the same time, the disease has a widespread nature of the lesions - unlike other diseases from the IBD group ("inflammatory bowel diseases"), it can affect any part of the digestive tract, from the oral cavity to the rectum (Fig. 3).
Figure 3. Crohn's disease can affect the entire digestive tract. Source: QuIBDO
Crohn's disease, like many others from the group of autoimmune diseases, has a chronic course - one way or another, once it occurs, it will accompany the patient for many years. However, with proper treatment, the symptoms of the disease can often be minimized.
Crohn's disease in children
The onset of Crohn's disease in children occurs on average at 10-15 years of age. Boys are more likely to get sick. Just like in adults, any part of the digestive tract can be affected in children, but most often the disease occurs in the form of ileocolitis, colitis and ileitis.
Symptoms of Crohn's disease
Symptoms of Crohn's disease can be divided into several groups:
- General symptoms: fatigue and weakness, fever, bone loss.
- Intestinal symptoms: abdominal pain and intestinal cramps, nausea, vomiting, weight loss, vitamin deficiencies, etc.
- Extraintestinal symptoms: damage to the oral mucosa (“aphthous stomatitis”, Fig. 4), eyes (conjunctivitis, etc.), skin. Occurs in approximately 12% of cases.
- Symptoms of complications that have begun.
Figure 4. Aphthous stomatitis sometimes becomes the only manifestation of Crohn's disease.
Source: jorgecachoh/Depositphotos Depending on the location of the lesion, symptoms can be combined in different ways (Table 1).
Table 1. Symptoms of Crohn's disease with lesions of various locations.
| Form of the disease | Localization of the lesion | Symptoms | Frequency |
| Ileocolitis | Ileum+right flank of colon | Diarrhea, abdominal pain, intestinal cramps, weight loss | 42% |
| Ileitis | Ileum | Diarrhea, abdominal pain, intestinal cramps, weight loss | 33% |
| Colitis | Colon | Diarrhea, rectal bleeding, formation of abscesses, fistulas and rectal ulcers | 20% |
| Other forms | A combination of various areas involving the stomach, duodenum, anal area, etc. | Anorexia, weight loss, nausea, vomiting. | 5% |
Symptoms in children
In children, there is a predominance of extraintestinal symptoms over intestinal ones. So, the disease at first may manifest itself:
- joint pain,
- anemia,
- hypovitaminosis,
- a rise in temperature for no apparent reason (the so-called “fever of unknown origin”),
- growth retardation and weight loss.
Diarrhea and abdominal pain may be absent.
Types of Crohn's disease depending on the classification according to the main characteristics
The classification of Crohn's disease has changed several times. Experts tried each time to group the pathology according to a certain type of sign.
First, we give the names of inflammation depending on location:
- gastroduodenal form - indicates damage to the stomach and duodenum;
- Crohn's disease of the small intestine is divided into ileitis (inflammation of the ileum) and jejunoileitis (ileum and jejunum);
- Crohn's disease of the colon - represents a limited lesion of the large intestine only;
- ileocolitis is a form indicating a simultaneous process in the ileum and colon.
The 1976 classification further highlighted:
- jeunitis - isolated lesion of the jejunum;
- inflammation of the anal area.
Enterocolitis is a joint inflammation of the entire intestine, granulomatous colitis is a lesion within the large intestine, pan-regional is Crohn's disease with damage to the entire gastrointestinal tract.
In 1982, Soviet scientists V. Fedorov and M. Levitan proposed to simplify the classification:
- enteritis,
- enterocolitis,
- colitis
The latest modification was adopted by a specialized European society in 2005. She combined the age of the patients, the form of the disease, and the location of inflammation. The text version has been replaced by coding for signs of Crohn's disease.
The age of initial diagnosis is noted: for children under 16 years old - A1, then up to A3
Pathology forms are coded as code B:
- B1 - inflammatory without complications, possibly combined with a fistula or abscess, transition to the anal area;
- B2 - stenotic, confirmed by examination, possibly associated with a perianal fistula or abscess;
- B3 - penetrating, intraperitoneal fistulas predominate in the clinic.
Each localization is assigned an L code from 1 to 4; in case of combined lesions, the record is kept in the form of a sum.
The severity of the flow is assessed by points when calculating activity. They consist of a seven-day observation of the patient, taking into account the frequency of diarrhea, abdominal pain, extraintestinal symptoms, fistulas or anal fissure, temperature rise above 37.8, patient weight, general health, dose of drugs, determination of infiltrate in the peritoneal cavity, hematocrit in the analysis blood.
The sum of points shows the severity of the patient:
- 150–220 - light;
- 220–450 – moderate;
- over 450 - high;
- less than 150 is considered remission.
According to this system, an exacerbation is considered to be the reappearance of symptoms with a score of more than 150, and a relapse includes cases of resumption of symptoms after surgical treatment of Crohn's disease, confirmed by laboratory diagnostics and instrumental methods.
Diagnostics
Diagnosing Crohn's disease is often difficult. Due to the fact that the symptoms of the disease are nonspecific and the disease is uncommon, the patient may experience pain for years without knowing about the disease. Therefore, if there are suspicions and a family predisposition, it is necessary to consult a doctor and undergo diagnostics - in several stages.
Clinical signs
Like diagnosing any disease, diagnosing Crohn's disease begins with the patient's medical history. The doctor carefully interviews the patient, paying attention to:
- the presence of characteristic symptoms and their intensification at night,
- any symptoms of the eyes, joints or skin,
- the presence of intolerance to any food,
- a history of smoking or the patient's use of various medications (including antibiotics) for a long period.
Based on the obtained clinical picture, the doctor prescribes further examination.
It should be borne in mind that the symptoms of Crohn's disease (abdominal pain, diarrhea, nausea, vomiting, bloating, etc.) may be characteristic of other diseases - for example, irritable bowel syndrome or ulcerative colitis. The main differences between ulcerative colitis are the presence of a urge to defecate with a small volume of stool (tenesmus) and damage only to the colon, in contrast to Crohn's disease, which can affect any part of the digestive tract. With irritable bowel syndrome, there is a connection between exacerbations and psychoemotional factors, the absence of severe pain on palpation of the intestine, and the absence of signs of inflammation.
What examination is necessary if Crohn's disease is suspected?
Unfortunately, it is impossible to make a diagnosis based on the clinical picture alone. Therefore, the patient undergoes tests and, according to the doctor’s indications, undergoes various instrumental studies:
- general and biochemical blood test: identifying signs of inflammation, the presence of deficiencies (protein, various vitamins and microelements, etc. due to impaired absorption in the intestine due to damage to the mucous membrane), assessment of the degree of disease activity (detection of anemia, leukocytosis, thrombocythemia, acceleration of ESR , increased concentration of CRP, hypoproteinemia with hypoalbuminemia, hypokalemia);
- detection of antibodies against Saccharomyces cerevisiae (ASCA) - helps in the differential diagnosis with ulcerative colitis, since these antibodies are detected in Crohn's disease more often than in any other IBD.
- Calprotectin and lactoferrin in feces are signs of exacerbation of inflammatory bowel disease.
Imaging research methods
This is a group of methods where, using various technologies (X-ray radiation, reflection of ultrasonic waves, etc.), it is possible to obtain an image of an internal organ and examine it for the presence of pathologies. Imaging methods include:
- X-ray contrast examination is a method of x-ray examination, which involves the introduction into the body of a special contrast agent that stains the intestinal lumen. The method allows you to identify altered areas of the small or large intestine (single or multiple narrowings, characteristic deep ulcerations giving a “cobblestone” picture, fistulas);
- Ultrasound, CT and MRI. They are used to detect abscesses and fistulas, visualize the intestinal wall, assess its thickness and lumen width. The sensitivity of CT and MRI in diagnosing CD is ≈ 80%. This figure means that this study can detect Crohn's disease in 80 out of 100 sick patients.
Endoscopy
An endoscopic research method is a type of examination in which a flexible tube (endoscope) with a camera at the end is inserted into the natural openings of the body (mouth, rectum), and the image from the camera is displayed on the screen. This allows the doctor to visually assess the condition of the patient’s internal organs. Endoscopic methods include:
- Colonoscopy (Fig. 5), which involves inserting an endoscope through the rectum into the large intestine. Allows you to assess the nature and degree of inflammation in the colon and in the final section of the ileum (taking a large number of biopsies is indicated - using an endoscope and special forceps, a small section of the intestinal mucosa is taken for further examination).
- Capsule endoscopy, when not an endoscope is used, but a capsule with a video camera inside, which the patient must swallow. While passing through the gastrointestinal tract, the camera takes pictures and transmits them to a special device. The method is used when inflammatory changes in the small intestine are suspected, which are inaccessible to conventional endoscopic and radiological examinations.
- Enteroscopy is an examination of the small intestine using an endoscope inserted into the mouth or anus. Among other things, it allows you to obtain biopsies from the small intestine, increase the narrowing of the intestine, remove the retained endoscopic capsule and stop bleeding (all this is done by introducing special instruments into the endoscope channels).
All these methods require preliminary preparation of the patient: refusing to eat for 8 hours or more, using laxatives or enemas.
Figure 5. Performing endoscopy. Source: Mayo Foundation
Histological examination
When performing endoscopic examinations - colonoscopy, enteroscopy - a biopsy of a section of the intestine is taken using an endoscope and examined under a microscope. Studying the biopsy cells allows us to assess the presence of signs of inflammation and the degree of its activity.
Microbiological examination of stool
The patient's stool is cultured on nutrient media to determine the type of bacteria living in the intestines.
With chronic inflammation in the intestines, favorable conditions are created for the development of pathogenic microflora. Bacteria are the direct cause of the development of purulent complications. To prevent and treat them, a microbiological study is performed to determine the type of bacteria and prescribe antibiotics.
Symptoms
Symptoms of Crohn's disease in adults and children are very diverse. There is no single evidence-based set of clinical signs. Patients visit different specialists to treat their symptoms.
Regarding aphthous stomatitis - see a dentist, a therapist with unknown abdominal pain, or a proctologist with a lesion in the anal area (fistula, fissures, abscess formation). There are intestinal and extraintestinal symptoms. It depends on the localization of the process, the severity of the course, the frequency of relapses, and the form of inflammation.
Intestinal signs include:
- prolonged diarrhea (considered chronic if it lasts more than 6 weeks);
- abdominal pain - worse after eating;
- nausea, vomiting;
- flatulence;
- weight loss - first supported by refusal to eat due to fear of pain, then by malabsorption syndrome against the background of a widespread process.
The pain can be disguised as acute appendicitis if it is localized in the iliac region on the right.
Symptoms of the general condition:
- lack of appetite;
- increased fatigue, constant fatigue;
- temperature rise of a wave-like nature.
The fistula form is manifested by: non-healing anal fissures, rectal fistulas. The correct diagnosis is made after unsuccessful use of medications and surgery for another reason.
Symptoms of Crohn's disease of the colon are often accompanied by high body temperature. Damage to the small intestine is indicated by the patient's sudden weight loss, impaired absorption of proteins, fats and carbohydrates, loss of vitamins (especially A, D, B12) with signs of hypovitaminosis, severe steatorrhea (fatty feces).
Extraintestinal signs
The course of the disease is characterized by the involvement of various organs and systems in the pathological process. How inflammation is transmitted from the intestine is unknown.
In the oral cavity, aphthous stomatitis is detected with painful bleeding ulcers, pain when eating
The eyes react with diseases of the membranes: conjunctivitis, uveitis, keratitis. Damage to the joints is characterized by inflammation of one (monoarthritis) with pain, redness, swelling, ankylosing spondylitis of the spine with severe pain during body movements, and the development of stiffness.
The skin reveals erythema nodosum, multiple pustules, gangrenous pyoderma, and angiitis of superficial vessels are possible.
Fatty degeneration forms in the liver, subsequently cirrhosis, sclerosing cholangitis develops in the biliary tract, stagnation of bile causes the formation of stones (cholelithiasis), which can subsequently lead to a malignant tumor, cholangiocarcinoma. For kidney and urinary tract tissues, typical manifestations are: cystitis, chronic pyelonephritis, nephrolithiasis, amyloidosis, hydronephrosis.
Manifestations of varying degrees of process activity
In practice, doctors use a combination of signs of the disease to determine the degree of activity of the process.
A mild degree is characterized by:
- diarrhea no more than four times a day;
- rare presence of blood in the stool;
- temperature not higher than 37.5 degrees;
- normal pulse.
In case of moderate activity:
- diarrhea recurs more than six times a day;
- there is always blood in the stool;
- moderate tachycardia (pulse 90);
- complications are likely.
Severe degree is different:
- severe diarrhea, stool more than 10 times a day;
- massive discharge of blood in feces;
- temperature within 38 degrees;
- tachycardia above 90 per minute;
- addition of complications.
Hyperthermia is one of the signs of an acute process
Symptoms in children
Features of symptoms in children for a long time do not allow making a correct diagnosis and prescribing optimal treatment for Crohn's disease. The clinical picture is blurred, poorly expressed, diarrhea is inconsistent, and primarily extraintestinal signs are detected. Cases of illness in children are severe and are accompanied by numerous complications.
Parents and attending physicians are advised to pay attention to the following signs:
Intestinal atresia in newborns
- pain in the abdomen - a child may have different types of pain from strong cramping to dull, aching;
- nausea, vomiting - observed when the gastric mucosa is damaged;
- bloating;
- diarrhea - the more intense, the higher the prevalence of intestinal inflammation, blood clots, impurities of pus and mucus, a fatty film are possible in the stool, the color of the stool becomes lighter;
- lack of appetite, weight loss;
- an unclear elevated temperature is determined;
- in a blood test, with good nutrition, a reduced hemoglobin level is found;
- teenage girls stop having periods;
- in half of the cases, inflammation occurs in the ileocolic area, symptoms manifest themselves in the form of an “acute abdomen”, urgent observation by a surgeon is required;
- extraintestinal symptoms do not differ from those in adult patients (stomatitis, congestion in the biliary tract, perianal abscess, fissures and fistulas of the anus, joint pain).
Treatment
Treatment of Crohn's disease is carried out comprehensively, using drugs of different classes and dietary recommendations.
Diet for Crohn's disease
There is no special diet designed exclusively for patients with Crohn's disease. In this case, the doctor prescribes a diet for patients with IBD (inflammatory bowel disease).
During the period of remission, such a diet is followed in order to prevent exacerbation and is based on the following principles:
- Food should not irritate the intestinal mucosa. Avoid foods rich in fiber and fat. The amount of fats and carbohydrates is reduced, protein consumption is increased at the rate of 2 g per 1 kg of the patient’s body weight.
- Dishes are prepared in a dietary way by boiling or steaming.
- Hard and thick foods that are difficult for inflamed intestines to digest are prohibited.
- Meals are distributed into 5–6 meals per day in small portions.
- The drinking regime must be observed: during the day you should drink 1.5–2 liters of liquid at room temperature.
- Herbs, spices, semi-finished products, pickles, smoked foods, and canned food are excluded.
- Salt is limited to 10 g per day.
- Food should not be hot or cold, so as not to cause an undesirable intestinal reaction to temperature.
During the period of exacerbation of the disease, normal absorption of food is disrupted. Pain of various localizations occurs (depending on the form of the disease in a particular patient) and diarrhea. Therefore, it is better to discuss the menu during an exacerbation with your doctor.
The basis of the diet will include liquid mixtures prepared from something that will not worsen the condition of the intestines. Also, the following products may most often be allowed:
- soups with a second broth;
- slimy porridges made from soft cereals;
- lean types of meat and fish, boiled or steamed;
- yesterday's white bread;
- jelly and jelly from berries and fruits;
- steam omelette;
- homemade cottage cheese.
Important! In order to alleviate the symptoms during the acute stage of the disease at home, in case of severe pain and cramps, you can use a warm heating pad, placing it on your stomach. In the first days of an exacerbation, the doctor may recommend a 1-2 day fast to reduce the symptoms of pain and diarrhea. A decoction of chamomile or rose hips, weak tea with lemon, and jelly can have a calming effect on the intestinal mucosa.
Drug treatment
Due to the fact that the pathogenesis of the development of the disease is complex, and the specific cause of its occurrence has not been identified, it is impossible to cure Crohn’s disease with one drug. With the help of various medications, we try to influence different stages of the pathogenesis of the disease - suppress the inflammatory reaction, treat purulent complications, etc.
Antibiotics
Prescribed in the presence of fistulas, abscesses and the development of other complications of Crohn's disease, as well as in the presence of pathological microflora in the intestines. Metronidazole, cephalosporins and other antibiotics are used, depending on the type of pathogenic flora identified. If the selected group of antibiotics does not help the patient, the drugs are changed until the desired effect of treatment is achieved.
Corticosteroids
They are first-line drugs for exacerbation of Crohn's disease. Depending on the degree of disease activity, prednisolone, methylprednisolone, budesonide, and hydrocortisone are prescribed in different doses. After relief of the acute phase, the dose is gradually reduced until complete withdrawal, if possible.
Immunosuppressors and immunomodulators
Taking into account the autoimmune mechanism of the disease, drugs that affect the immune system are used as a complex treatment to maintain a state of remission, as well as for intolerance to corticosteroids.
Biological products (monoclonal antibodies, etc.)
A number of biological products can be prescribed to influence the inflammation process and as a complex therapy that helps prolong the remission stage.
Other medicines
To relieve various symptoms (abdominal pain, diarrhea, etc.), the patient is prescribed analgesics, antidiarrheal drugs, salicylates and others - drugs that do not directly affect the mechanism of development of the disease, but alleviate certain symptoms.
Surgery
Surgical treatment is used for recurrent intestinal obstruction or untreatable fistulas, abscesses and other complications. Resection of the affected part of the intestine helps to reduce the severity of symptoms, but does not lead to a complete cure. Recurrences are possible even after resection of all affected areas.
Folk remedies
As a treatment method, folk remedies for Crohn's disease have no proven effectiveness. However, as a comprehensive treatment, they can improve the course of the disease. Traditional methods include taking herbal remedies that relieve inflammation in the intestines and stomach: chamomile, St. John's wort, plantain, elecampane and others.
Some authors note the importance of the psycho-emotional component in the development of Crohn's disease and its exacerbations. Healthy sleep, stress reduction and psychotherapy can be a good help in the fight against the disease.
Is it possible to permanently cure Crohn's disease?
As stated above, Crohn's disease is a chronic disease. And most chronic diseases cannot be completely cured - you can only control the severity of symptoms. Thus, subject to following the diet, prescribed treatment, and recommendations for maintaining a healthy lifestyle, it is possible to maximize remission and prevent relapses.
How to live with Crohn's disease?
Undoubtedly, Crohn's disease worsens the quality of life of patients. This largely depends on the period of the disease (relapse or remission), the degree of disease activity, and the presence of complications. At the time of exacerbation, constant pain and diarrhea almost make it impossible to function normally. However, in the remission stage the disease hardly manifests itself. By carefully following the treatment, diet and preventive measures prescribed by the doctor, the patient has every chance to prolong the period of remission as much as possible, although he will probably have to undergo treatment for the rest of his life.
Coping with the physiological discomforts of Crohn's disease is difficult, but here are some tips:
- Drink more water. This will help cope with dehydration.
- Wear loose clothing that will not constrict your body and cause discomfort.
- Rest often . Sleep will help you regain your strength and feel better.
- Use a heating pad to soothe stomach pain.
- Take probiotics as prescribed by your doctor to restore your gut microflora.
For many people, Crohn's disease is not only a health problem, but also a moral difficulty.
Diarrhea, pain, taking medications, frequent visits to the doctor, the threat of complications - all this cannot pass without leaving a mark on a person’s nerves. To cope with stress and make it easier to cope with exacerbations, people try a variety of methods, and here are some of them:
- Keeping a diary . In personal notes, you can throw out all your negative emotions, perhaps this will help you endure the disease more calmly and cope with stress.
- Meditation is a great way to calm down. If you find it difficult to do classical meditations, you can try guided meditation or various breathing practices to help you relax.
- Light physical activity and yoga . If your condition allows, you can go for a short walk and get some fresh air. For those who find it difficult to get out of bed, yoga in bed (video 1) may be suitable - easy and enjoyable exercises.
- Soothing tea with chamomile, nettle, lemon balm, mint - in the absence of contraindications.
- Watching your favorite films or TV series helps not to aggravate the stress of the disease, and to get a charge of pleasant emotions.
A flare-up of the disease can be very unpleasant and overwhelming, but the main thing to remember is that it is temporary.
Video 1. Yoga in bed. Source: youtube. com/c/videolikeworkout/
Treatment of Crohn's disease and ulcerative colitis
Both diseases respond well to various types of therapy, which may include medications. Both diseases can be controlled with medications that target the body's inflammatory response. They can reduce and eliminate many symptoms of illnesses, such as pain and diarrhea.
Both diseases reduce a person's appetite. In both cases, proper nutrition is of great importance. The diet must have sufficient nutrients. In any case, your doctor will help you develop a nutrition plan to avoid aggravating symptoms and ensure a healthy diet.
For complications such as intestinal perforation, excessive bleeding, cancer, or severe inflammation, the doctor will prescribe surgery. Surgery for any condition has a number of potential risks and will require recovery time. The doctor should discuss the possible benefits and risks of surgery with the patient before recommending it.