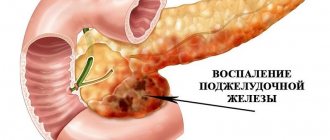
Characteristics of the pathology
The main cause of pancreatitis is a blocked duct. This condition can be caused by neoplasms, gallstones, and other factors. When the duct is blocked, the process of gastric juice outflow is disrupted (the substance contains enzymes that protect the pancreas from negative effects). The pathological process provokes deviations in the functional state of the organ. Enzymes begin to act inside the gland, destroying its tissue. This process is accompanied by swelling of the organ and pain.
An attack of pancreatitis is a period of exacerbation of this pathological condition.
Main causes of pathology
The causes of pancreatitis in some cases remain unclear, but attacks of the inflammatory process are always caused by specific factors. The main ones are alcohol abuse and poor diet. These factors can disrupt the action of pancreatic enzymes in a short period of time (especially if the digestive system is impaired by concomitant diseases).
Other causes of PP:
- malignant tumors in the pancreas;
- advanced gallbladder diseases;
- consequences of post-traumatic syndrome;
- nervous exhaustion of the body;
- excessively high cholesterol levels;
- infectious lesion of the digestive tract;
- regular intoxication;
- complications of operations on the digestive organs.
Why does an attack of pancreatitis occur?
Patients diagnosed with pancreatitis should follow a healthy diet. Even a single use of prohibited foods can provoke PP. Poor diet and alcohol consumption are the main causes of exacerbation of the disease.
There are also additional provoking factors that can shorten periods of remission. Their exclusion is the main measure for the prevention of pancreatitis.
Provoking factors:
- binge eating;
- drinking alcohol;
- reaction to certain medications;
- eating fatty, spicy, fried, salty foods;
- consequences of food allergies.
Symptoms of an attack
The intensity of symptoms in PP depends on the stage of development of the disease and the degree of damage to the pancreas. In acute pancreatitis, pain is pronounced. The chronic form of the disease may be accompanied by latent symptoms (in the early stages of development, the disease may develop asymptomatically). The attacks in this case will be practically imperceptible to the patient. All types of exacerbations are united by one factor - pain syndrome. PP always manifests itself in the form of girdling or spasmodic pain.
Symptoms of PP:
constant feeling of nausea;- uncontrollable vomiting;
- bloating;
- pale skin;
- girdle pain;
- intense diarrhea;
- signs of tachycardia;
- pain in the left or right hypochondrium;
- belching followed by hiccups;
- increased body temperature;
- lack of appetite;
- regular heartburn;
- headache;
- lowering blood pressure.
Diagnostics
A gastroenterologist diagnoses PP. To identify the inflammatory process, general and biochemical blood tests are prescribed. Additionally, various types of testing are carried out. The condition of the pancreas is studied using instrumental examination. If there are symptoms of an attack, doctors carry out a differential diagnosis with acute appendicitis, exacerbation of cholecystitis, intestinal obstruction, and abdominal ischemic disease.
Diagnostic methods:
- General analysis and blood biochemistry;
- urine test for amylase activity;
- diagnostic tests for organ stimulation;
- glucose tolerance testing;
- Ultrasound;
- radiography;
- CT or MRI;
- ERCP.
Diagnosis and treatment
Pancreatitis has a clear, specific clinical picture, which allows the gastroenterologist to make an initial diagnosis after examination, palpation, percussion and collection of the patient’s medical history. To determine the severity of the disease, it is necessary to undergo a complete examination.
Diagnostic methods:
- clinical blood test - allows you to see the degree of the inflammatory process;
- urinalysis - with pancreatitis, amylase levels increase;
- coprogram;
- blood sugar test;
- biochemical blood test - determines the level of pancreatic enzymes and liver function;
- Ultrasound, CT, radiography of the abdominal organs;
- EGDS - using a small camera to study the condition of the gastrointestinal tract from the inside.
Drug treatment
During an acute attack of the disease, a person is given intravenous drips of drugs to eliminate dehydration and normalize blood pressure, suppress the enzymatic activity of the gland, and eliminate pain. Then drug treatment is started, the purpose of which is to eliminate the symptoms of the disease and restore the functioning of the organ. Most often, tablets are used; in severe cases, injection solutions are used.
How to treat pancreatitis - doctor's advice:
- antispasmodics – Drotaverine, Papaverine;
- anticholinergics – Atropine;
- antibiotics – Trichopolum, Tobramycin;
- drugs to reduce the secretion of gastric juice - Orthanol, Ranitidine, Histodil;
- enzymes – Creon, Mezim, Pancral;
- sorbents – Enterosgel;
- medications to reduce the production of pancreatic enzymes - Gordox, Kontrikal.
For pancreatic necrosis, blockage of the gland ducts with stones, traditional treatment methods will not help; surgical intervention is necessary. The entire pancreas is rarely removed, since the operation is complex and fraught with complications.
Folk remedies
Alternative medicine methods help relieve inflammation and other manifestations of pancreatitis, prolong the remission stage, but they should be used in combination with drug therapy, only after agreement with the attending physician.
Simple recipes for treating pancreatitis at home:
- Pour 250 ml of boiling water over 20 g of chopped walnut leaves, simmer over low heat for 5 minutes, cool, strain. Take 70 ml three times a day.
- Mix chopped blueberry leaves and bean pods in equal proportions. 1 tbsp. l. pour 220 ml of boiling water over the mixture, strain after a quarter of an hour. Drink 100 ml three times a day before meals.
- Pour 500 ml of water into 100 g of unpeeled oat grains, cook over low heat for 40 minutes, grind the mixture, cook for another 20 minutes. Strain the resulting decoction and drink 100 ml three times a day.
- Pour 500 ml of cold water into 5 g of crushed dry immortelle and leave for 8 hours. Drink 200 ml once a day for 20 days.
To improve the digestion process, people with inflammation of the pancreas need to eat fresh strawberries, gooseberries, persimmons, cherries, drink juice from cabbage, celery, currants, and raw potatoes.
An attack of pancreatitis - what to do?
The manifestation of symptoms of PP is grounds for immediate consultation with a doctor. In most cases, an attack occurs suddenly, so the best option is to call an ambulance. Before specialists arrive, the patient must perform a number of actions to alleviate his condition. Home treatment is permissible only in cases of mild attacks of the chronic form of the disease.
First aid and relief
During PP, patients should not take a horizontal position (the pain will increase). The best option is the “embryo” pose. The second way to reduce pain is to sit down with your torso strongly tilted forward. After relief of the condition, it is necessary to carry out a number of actions to stop the attack.
If the pain syndrome persists, then the patient needs qualified medical care (a team of doctors must be called).
First aid measures:
- ensuring the patient complete rest (sudden movements are prohibited);
- exclusion of food consumption (at least for 24 hours);
- preventing dehydration of the body (you can drink alkaline mineral water every hour, a quarter glass);
- stopping an attack with antispasmodic drugs (No-Shpa);
- To relieve pain, you can use a cold compress (for example, any frozen food from the refrigerator).
Home treatment
Self-medication for pancreatitis is prohibited. The disease provokes complications that are incompatible with life. At home, you can carry out preventive measures, carry out courses of therapy drawn up by a doctor and provide first aid in case of exacerbation of the inflammatory process.
You cannot use folk remedies as the main method of treating pancreatitis or to relieve PP.
Acceptable home treatment options:
- diet therapy (a mandatory point in the treatment of the inflammatory process);
- taking medications prescribed by a doctor;
- changing lifestyle (observing a rest regime, ensuring sufficient physical activity, preventing stressful situations);
- implementation of preventive measures.
Specialized medical care
In most cases, PN involves inpatient treatment. The first task of doctors is to temporarily exclude the pancreas from the digestive system. This state of the organ is ensured by fasting. During the first day (or 48 hours), the patient should not eat food. The fluid supply is replenished with alkaline mineral waters. In severe cases of pancreatitis, the period of fasting can reach three days. The further treatment regimen depends on the individual clinical picture of the patient’s health status.
Stages of medical care for PP:
- elimination of signs of intoxication of the body;
- increasing the level of enzymes in the blood to normal levels (Pancreatin, Creon);
- elimination of the consequences of dehydration;
- drug treatment (antibiotics, antiseptics, antispasmodics, analgesics, enzyme medications, vitamin complexes, etc.);
- restorative therapy.
The hospitalization period is on average two weeks. After discharge, the patient is given recommendations on how to prevent repeated PN (daily routine, dietary habits, preventive measures). Additionally, the doctor explains what actions should be taken in the event of a relapse of the attack.
If the patient follows the specialist’s recommendations, the risk of exacerbation of pancreatitis is reduced. Remissions for this disease can be quite long.
Video on the topic: Health. Chronic pancreatitis. You can't stomach it!
Complications of the disease
Pancreatitis provokes the gradual destruction of the pancreas. Violation of the functional state of the organ leads to failures in other body systems. The inflammatory process can cause the death of the patient if there is no adequate therapy and preventive measures are not taken.
Possible complications:
- pancreatic necrosis (purulent destruction of the pancreas);
- peritonitis;
- vein thrombosis;
- sepsis;
- abscesses and cystic formations;
- pancreas cancer;
- obstructive jaundice;
- retroperitoneal phlegmon;
- diabetes;
- internal bleeding.
Signs of an attack in chronic pancreatitis
If in an acute course the pain can be tolerated, then an attack in chronic pancreatitis requires emergency care. After all, with such a course of the disease, the patient suffers from pain.
Also read on our website: We treat pancreatitis at home using folk methods
As for the pain syndrome, a spasm occurs that radiates not only to the back, but also to the epigastric region.
Often chronic pancreatitis is accompanied by a painful attack in the right or left hypochondrium.
In addition to pain, the patient’s temperature rises to a maximum of 38 degrees and chills occur.
Important! Chills can appear simultaneously with fever - this indicates the beginning of a purulent inflammatory process.
Many people ask why it is impossible to stop an attack at home? In fact, you can relieve the attack a little at home, but you still need to call an ambulance.
To the question: is it possible to cure a stomach or duodenal ulcer at home, a gastroenterologist, head of the gastroenterology department, Mikhail Vasilievich Arkhipov, answers.
After all, if measures are not taken in a timely manner, complications may arise. Now you understand what the symptoms of an attack of pancreatitis are, and then we will consider treatment at home.
What should be the diet during attacks of pancreatitis?
Proper nutrition for pancreatitis is one of the main methods of treating the inflammatory process. The diet is followed at all stages of treatment and is the most effective measure to prevent recurrent attacks. Violation of the diet reduces the tendency to recovery and can significantly worsen the patient's condition.
Principles of nutrition for PP:
- on the first day, food intake is prohibited (it is not difficult for the patient to fulfill this condition; during an exacerbation, patients have no appetite);
- food can be consumed on the third day after the relief of PP (carbohydrate-containing and protein foods, water-based cereals, vegetable soups);
- the first meals should be taken in small portions (it is better to eat it in minimal quantities, but often);
- on the fourth day, low-fat cottage cheese and fermented milk products can be introduced into the diet;
- boiled chicken or beef can be included in the menu from the sixth day (you cannot eat such products for dinner or breakfast);
- You can return to a full-fledged diet from the tenth day (the menu must comply with the rules of a healthy diet).
Diet No. 5
Diet No. 5 has some features. The diet is divided into two stages, each of which is carried out during a certain course of the disease (the first - during an exacerbation, the second - after the attack has stopped). In the first days, the patient is recommended to fast. Gradually, slimy soups, pureed porridges, fruit jelly, vegetable puree, steamed cutlets and low-fat cottage cheese are introduced into the diet. The second stage of the diet allows you to expand the menu.
Authorized products:
- vegetable soups with pureed vegetables;
- lean meat (rabbit, veal, beef, chicken, turkey);
- vegetables (potatoes, zucchini, pumpkin, beets);
- cereals (oatmeal, semolina, buckwheat porridge, rice);
- low-fat fish;
- unhealthy cookies;
- low-fat dairy and fermented milk products;
- egg white omelet;
- baked apples;
- dried fruits compote;
- fruit jelly;
- weak tea;
- rosehip decoction.
Prohibited foods include: fatty meats, rich meat and mushroom soups, wheat and rye bread, baked goods, whole milk, vegetables with coarse fiber, crumbly cereals. It is strictly forbidden to eat fried, salty, spicy foods, marinades, or lard. It is recommended to prepare food by boiling, stewing or steaming. Alcohol, strong coffee, chocolate, spices and seasonings can provoke PP.
How to eat properly after an attack?
In the first days after an attack, doctors strongly recommend that the patient go on a hunger strike.
On this day, after the main treatment, you will be prescribed droppers with glucose and vitamins; they will enrich your body with useful substances. Also read on our website: Treatment of pancreatitis with medications - which ones are more effective
On the third day, stick to a protein and carbohydrate diet. You can include soups and cereals in your diet.
The main thing is that the food consumed should be unsalted, and in no case should you add seasonings.
On the fourth day, you can include a little low-fat cottage cheese or other fermented milk product in your diet. Some doctors allow you to eat white fish on the 4th day, but only steamed fish.
Beef and chicken can be included in your diet only after the 6th day. But it’s still better to make do with cottage cheese products for breakfast.
Starting from the 10th day, you can switch to a regular diet. We would like to warn you - you should not immediately consume fatty foods, because this can negatively affect the pancreas.
Chief gastroenterologist of the Russian Federation: “PANCREATITIS does not go away?! A simple treatment method has already healed hundreds of patients at home! To cure the pancreas forever you need...” Read more »
How to prevent further aggravation
To prevent an attack of pancreatitis, you should follow your doctor's recommendations and change your lifestyle. Smoking, drinking alcohol, and eating prohibited foods should be excluded (even a one-time violation of the regime can cause an exacerbation). Excessive physical activity is prohibited. Concomitant diseases of the digestive system can provoke PP.
Any pathologies should be treated in a timely manner. You must not violate the medication therapy schedule drawn up by your doctor.
Preventive measures
Prevention of PP includes the exclusion of factors that can provoke an exacerbation of the inflammatory process. The recommendations represent basic rules for a healthy lifestyle. If the patient is prescribed a course of medication, it is impossible to stop it prematurely. In most cases, specialists prescribe medications to improve the functional state of the pancreas, which increase the protective properties of the organ.
Preventive measures:
- rejection of bad habits;
- providing the body with sufficient physical activity;
- stay in the fresh air for at least two hours a day;
- compliance with the diet (the diet should contain a sufficient amount of vitamins, harmful foods should be excluded).
Video on the topic: 5 exercises for pancreatitis, cholecystitis, gallbladder dyskinesia.
Symptoms of acute pancreatitis
An important internal organ in the human body is the pancreas, which helps digest food. It also secretes many hormones and enzymes necessary for digestion. Inflammation in the pancreas causes a disease called pancreatitis.
There are two forms of the disease:
- Spicy.
- Chronic.
In both cases, the inflammatory process of the pancreas is accompanied by acute pain. If there is no appropriate treatment and the patient violates the diet, damage to necrotic tissue is observed, as a result of which the person may die.
In acute pancreatitis, the following symptoms often occur:
- pain in the hypochondrium on the right;
- girdling pain in the back;
- nausea and vomiting;
- bloating is observed;
- no appetite;
- blood pressure decreases;
- headache;
- signs of tachycardia are observed.
Moreover, the pain may ease slightly if the patient, sitting, pulls his knees towards him. Even if the attack has passed, it is necessary to seek help from a doctor to avoid serious consequences.
Questions often arise about which specialist should be consulted in order to recognize the signs of acute pancreatitis. If these symptoms occur, it is necessary to contact a therapist, who, after examining the patient’s condition, will give a referral to a gastroenterologist. He will conduct a study and prescribe therapy for taking medications and following a strict diet. If necessary, you will need to consult a surgeon and other specialists.