Human health largely depends on the state of the digestive system. Proper functioning of the gastrointestinal tract ensures the normal functioning of all body systems. However, due to the fact that modern people live in poor environmental conditions, experience regular stress, and eat junk food, the health of the digestive organs is under threat. As a result of the impact of a combination of negative factors on the human body, gastroparesis can develop. This gastrointestinal disease can lead to serious consequences.
What is gastroparesis
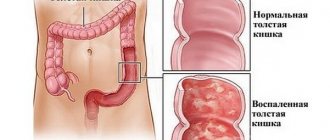
Gastroparesis develops as a result of damage to the gastric muscles, which leads to a weakening of their contractile function. Impaired peristalsis prevents food from mixing with gastric juice, pancreatic secretions and bile, which significantly impairs the digestion process. Unable to enter the small intestine, food lingers in the stomach, accumulates and undergoes a process of rotting. The consequence of this is intoxication of the body, which causes the following symptoms:
- discomfort or pain in the stomach;
- nausea;
- vomit.
Consequences of diabetic gastroparesis
The processes of rotting undigested food contribute to the proliferation of pathogenic bacteria that affect the functioning of the gastrointestinal tract. In addition to all this, food deposits clump and block the main exit to the intestine. The current situation is getting worse each time.
Another serious consequence of gastroparesis in diabetes is hypoglycemia. A process beyond the body’s control occurs against the background of unprocessed food that the human body needs. Based on all this, we can compare the discrepancy between the dosage of the hormone insulin and the amount of food transported. In this case, with a sharp decrease in glucose, the body will feel energy starvation, which does not allow it to control the level of monosaccharide.
The acquired consequences of diabetic gastroparesis can also manifest themselves in patients with type 2 diabetes, only with a lesser degree of severity. In this situation, the pancreas is still capable of producing its own hormone. Therefore, the threat of glycemia when following a low-carbohydrate diet with complex insulin administration is significant.
Causes of gastroparesis
Gastroparesis occurs as a result of disruption of the normal innervation of the stomach muscles, which, as a rule, indicates the presence of other chronic diseases. Doctors include the main reasons for the development of pathology:
- diabetes;
- stroke;
- Parkinson's disease;
- damage to the vagus nerve;
- long-term use of painkillers and sedatives;
- deficiency of some microelements (calcium, magnesium, potassium);
- postoperative complications;
- stress;
- multiple sclerosis.
Since the causes of gastroparesis are varied, for successful treatment of the disease it is important to know what led to its development, and this is only possible after a diagnostic examination.
Types of gastroparesis
Diabetes mellitus causes the development of this pathology in almost 30% of cases. High blood sugar causes nerve damage, which is why people with diabetes are at risk.
In cases where gastroparesis is not associated with diabetes, it is difficult to determine what exactly was the impetus for the development of the disease.
Thus, gastric paresis is represented by two types:
- diabetic;
- idiopathic.
These types of pathology differ in etiology, and, consequently, in treatment methods. The second type is accompanied by other chronic diseases and is more difficult to diagnose.
Diabetic gastroparesis
This type affects people who have been diagnosed with diabetes. In this case, the disease develops as secondary to diabetes mellitus and significantly complicates the treatment of the underlying disease. The main cause of this pathology is a high level of glucose in the blood, which damages the nerve fibers that transmit impulses to the muscles of the stomach .
If the normal process of gastric emptying is disrupted, it is more difficult to control glycemic levels. Therefore, the fight against this type of gastroparesis is necessary to maintain a stable condition of a person suffering from diabetes.
Idiopathic gastroparesis
Gastroparesis is called idiopathic, the causes of which cannot be clearly identified. The development of this pathology can be provoked by:
- rotaviruses;
- Epstein-Barr virus;
- acute gastroenteritis;
- other infectious diseases suffered by a person during his life.
Symptoms
Diabetic gastroparesis is dangerous because food cannot be fully digested by the stomach and accumulates in it, forming a lump. Severe pain appears, fermentation processes develop and the number of pathogenic microorganisms increases, which further worsens the human condition.
Symptoms of gastroparesis:
- a feeling of rapid satiety even after ingesting a small amount of food;
- an increase in the size of the anterior wall of the abdominal cavity;
- severe heartburn;
- prolonged belching;
- nausea leading to repeated persistent vomiting - it is worth noting that vomiting does not bring relief;
- defecation disorder;
- weight loss - occurs due to reluctance to eat food, since almost all clinical manifestations occur after a meal;
- feeling of fullness and distension in the stomach;
- pain of varying severity;
- increased anxiety;
- development of a depressive state;
- signs of dehydration;
- fluctuations in blood sugar levels.
Ignoring external manifestations can lead to complications that are dangerous to human life.
Clinical picture
When a malfunction occurs in the gastrointestinal tract, it always negatively affects the general condition of the patient and is manifested by a set of symptoms that are characteristic of many other types of disorders.
The following symptoms of gastroparesis in diabetes mellitus can be distinguished:
- vomiting and nausea after eating;
- bloating;
- early feeling of fullness;
- discomfort and pain in the abdominal area;
- large food remains in the vomit;
- weakness and general malaise.
The main signs of diabetic gastroparesis are nervous and physical exhaustion of the body, and, as a consequence, apathy and chronic fatigue. The severity and severity of symptoms depends on the stage of development of the disease.
- Gastric paresis or impaired evacuation function, not associated with diabetes, is also manifested by nausea up to several times a week, short-term vomiting at least once a week.
- With idiopathic gastroparesis, prolonged vomiting attacks are observed, occurring several times a year.
- When eating, the patient, just as with diabetic gastroparesis, feels early satiety, since undigested food remains in the stomach.
Gastroparesis and Ayurveda
According to classical Ayurvedic texts, a condition of "slow digestion" such as gastroparesis is the result of an aggravation of one or more of the three doshas of the body - vata dosha, pitta dosha and kapha dosha.
Therefore, Ayurvedic experts advise patients with gastroparesis to avoid eating foods that aggravate the associated dosha.
In general, patients with this disease should avoid fatty, heavy, toxic, sweet and cold foods. They are advised to eat foods that have pungent and bitter tastes (guna). In addition, patients with gastroparesis should eat pureed, well-cooked food, chew it properly, and drink plenty of water.
How is the disease diagnosed?
Diagnosis of gastroparesis is complicated by the fact that various diseases of the digestive system have similar symptoms. Diagnosis requires a comprehensive examination, including blood tests, tests that determine the rate at which food is eliminated from the stomach, and monitoring of glucose levels.
Radiography
To diagnose gastroparesis, an X-ray examination of the gastrointestinal tract is performed. The method is based on the use of an X-ray contrast agent (in this case, a weak barium solution), which is injected into the patient’s body in order to highlight or highlight the necessary areas of internal organs in the image.
Radioisotope testing is absolutely safe and does not cause pain, since the concentrated solution drunk by the patient, as a rule, does not cause allergic reactions, so it is not capable of causing harm to health. By tracking the movement of the radioisotope through the gastrointestinal tract, the rate of gastric emptying is determined. If, after 4 hours after eating food, the isotope content in the body reaches 10%, then the diagnosis of gastroparesis is confirmed. Subsequently, the radioactive element is eliminated from the body.
FEGDS
Another method for detecting gastroparesis is FEGDS (fibroesophagogastroduodenoscopy). This type of study is used to study the internal state of the digestive system.
The procedure is carried out using an endoscope, which is inserted through the oral cavity into the stomach and duodenum. This method allows tissue to be taken for biopsy.
Breath test
Along with other methods for diagnosing gastric paresis, a breath test is used. This technique is also based on the principle of tracking the movement of a contrast agent in the digestive organs.
- In this case, a non-radioactive carbon isotope is introduced into the stomach along with food.
- Once in the duodenum, the substance is transformed into carbon dioxide, which the patient exhales.
- Special devices analyze the composition of exhaled air. Based on the carbon dioxide content, conclusions are drawn about the rate of elimination of food from the stomach.
Antroduodenal manometry
Damage to the gastric muscles during gastroparesis leads to a weakening of contractions or a decrease in their frequency. To detect disturbances in the peristalsis of the stomach and duodenum, doctors use a research method such as antroduodenal manometry.
Diagnostics
One or more of the following diagnostic methods are used to confirm gastroparesis:
- Contrast radiography of the stomach.
The principle of the technique is based on contrasting the stomach with radiopaque agents. After preliminary fasting, the patient is asked to swallow a barium suspension (contrast agent). During this period, food intake is allowed. If 12 hours after the end of taking barium suspension it is found in the stomach, then this indicates gastroparesis. - Scintigraphy of the stomach.
The study involves the use of a radioactive drug. Scintigraphy can be both static and dynamic. In the first option, it is assumed to take a one-time series of images, in the second, several at certain intervals. During breakfast, the patient takes a radioactive isotope, which enters the stomach with food. The radiopharmaceutical acts as an indicator of the movement of food through the digestive tract. In the absence of gastroparesis, food along with the radioactive isotope is completely evacuated from the stomach after 4 hours. If after two hours more than half of the radioactive drug remains in the stomach, then the diagnosis of gastroparesis is confirmed. - Electrogastrography (electrogastrogram)
. This test examines the activity of the bioelectric potentials of the muscle cells of the stomach. The doctor inserts a thin tube down the throat and into the stomach. It contains a wire that measures the electrical activity of the stomach. If his motor skills are impaired, characteristic changes are recorded on the electrogastrogram (teeth with incorrect amplitude, abnormal waves). - Blood chemistry. Laboratory tests can detect electrolyte imbalances.
To exclude other causes of gastroparesis (for example, organic pathology of the stomach), the doctor may prescribe endoscopic and ultrasound examinations.
- Fibroesophagogastroduodenoscopy
is an endoscopic examination of the initial parts of the digestive system. It is usually carried out to exclude organic diseases of the pyloric part of the stomach, in which the symptoms are similar to gastroparesis. After administering the sedative, the doctor passes a long, thin tube (a device called a gastroscope) through the mouth, and then carefully guides it down the esophagus and into the stomach. Using a gastroscope, the doctor examines the gastric mucosa, where he can identify various abnormalities that cause problems with the evacuation of gastric contents.
- Ultrasound examination of the abdominal organs.
An ultrasound can help identify disease in the gallbladder and pancreas that may be causing the problem. During the study, harmless sound waves are used to visualize the organs of the upper half of the abdominal cavity (outline the contours and evaluate the tissue structure of the gallbladder and pancreas).
Treatment
Gastric paresis is a serious disease that affects all systems of the body. Therefore, treatment for gastroparesis should begin as early as possible. Therapy can only be prescribed by a qualified gastroenterologist after conducting the necessary tests, hardware and laboratory tests.
Drug treatment
This type of treatment involves taking medications that stimulate muscle contraction, facilitating the movement of food from the stomach to the intestines.
- Typically, drugs such as Domperidone and Metoclopramide are prescribed to increase gastric muscle activity.
- For a similar purpose, patients with gastroparesis are prescribed a common antibiotic, Erythromycin, in low doses.
- In severe cases, Cisapride is used.
It should be remembered that all drugs have side effects.
Diet recommendations
Treatment of paresis involves not only the use of medications, but also mandatory adherence to a therapeutic diet. Doctors recommend to patients:
- reduce fat intake in the diet;
- reduce the amount of fiber;
- take food in small portions and chew it thoroughly;
- give preference to food with a liquid and soft consistency;
- drink at least 1.5 liters of water per day;
- give up alcoholic, energy and any other carbonated drinks;
- have dinner no later than 4 hours before bedtime.
Usually, compliance with the above conditions significantly alleviates the patient’s condition; regular adherence to nutritional recommendations contributes to a speedy recovery.
Electrical stimulation for gastroparesis
In cases of severe gastroparesis, when the diet does not lead to positive results and drug therapy is ineffective, the patient is offered to have a device implanted under the skin for electrical stimulation of the stomach muscles.
The impulses sent by the device along the electrodes cause muscle contractions, and food does not stagnate in the stomach cavity.
Diagnosis and treatment
To identify gastric paresis in diabetes and determine its stage of development, you need to constantly monitor and record sugar levels for 2-3 weeks. In addition, the patient needs to be examined by a gastroenterologist.
The presence of a neurological syndrome is indicated by the following phenomena, which can be detected by keeping a self-monitoring diary. So, 1 or 3 hours after a meal, the glucose concentration always remains normal, and on an empty stomach the sugar levels are elevated even with a timely dinner.
Moreover, with paresis, the level of glycemia in the morning constantly fluctuates. And after eating food, the sugar content remains normal and increases only 5 hours after the meal.
Gastroparesis in diabetes can also be detected by performing a special test. The experiment is to not inject insulin before meals, but you also need to give up dinner and give the injection at night. The next morning, on an empty stomach, you should record your sugar levels.
If the course of diabetes mellitus is not complicated, then morning glycemia should be normal. However, with paresis, hypoglycemia most often develops in diabetes mellitus.
Treatment for diabetic gastroparesis involves following a certain lifestyle and regularly monitoring sugar levels. The main goal of treatment is to restore the function of the vagus nerve, so that the stomach will begin to function normally again.
Complications of diabetes should be treated comprehensively:
- taking medications;
- special gymnastics;
- dieting.
So, to speed up the emptying process, the doctor prescribes drugs in the form of syrups or tablets. These drugs include Motilium, Betaine hydrochloride and pepsin, Metoclopramide and others.