Where is the esophagus located?
The esophagus is the connecting chain between the oropharynx and the body of the stomach. The anatomy of the organ is quite complex. It has its own innervation and a network of feeding vessels; glands that produce secretions open into the cavity. The wall is multi-layered, with natural bends and narrowings throughout.
The topography places it between the 6th cervical and 11th thoracic vertebrae, behind the trachea. The upper segment is adjacent to the lobes of the thyroid gland, the lower, passing through an opening in the diaphragm, connects to the stomach in its proximal part. The posterior part of the esophagus is adjacent to the spinal column, the anterior part is adjacent to the aorta and the vagus nerve.
You can see where the human esophagus is located; the photo gives a schematic idea.
Esophagus: skeletotopy, syntopy, parts, wall structure, blood supply and innervation.
The esophagus, esophagus, looks like a tube connecting the pharynx to the stomach (Fig. 488-491). The place of transition of the pharynx into the esophagus in an adult corresponds to the level of the VI cervical vertebra or the lower edge of the cricoid cartilage, and the place of transition to the stomach is projected at the level of the XI thoracic vertebra. In a living person, these boundaries can change when throwing back the head, taking a deep breath, or lowering the stomach. The length of the esophagus is up to 25 cm. A small part of the esophagus lies in the neck area, then the esophagus through the upper aperture of the chest descends into the chest cavity, and then, having passed the latter, through the esophageal opening of the diaphragm it penetrates into the abdominal cavity, passing into the cardiac part of the stomach (see. Fig.489). In this regard, three parts are distinguished in the esophagus: the cervical part, pars cervicalis, the thoracic part, pars thoracica, and the abdominal part, pars abdominalis. The cervical part, pars cervialis, is located from the level of the VI cervical vertebra to the I-II thoracic vertebra. Its length ranges from 5 to 8 cm. The thoracic part, pars thoracica, has the greatest length - 15 -18 cm and ends at the level of the IX-X thoracic vertebrae, i.e. at the point where the esophagus enters the esophageal opening of the diaphragm. The abdominal part, pars abdominalis, is the shortest, its length is 1-3 cm. The esophagus lies in front of the spinal column and has 4 bends along its path: two in the sagittal plane and two in the frontal plane. The initial section of the esophagus is located almost strictly along the midline. At the level of the II thoracic vertebra, the esophagus deviates to the left, occupying the extreme left position in the region of the III and IV vertebrae. Then, at the level of the V vertebra, it again lies along the midline, and below it goes slightly to the right of it. The bend to the right extends to the VIII thoracic vertebra. Heading downwards, the esophagus at the level of the VIII to X vertebrae again passes to the left side. These two curves lie in the frontal plane. The esophagus makes its first bend in the sagittal plane under the bifurcation of the trachea - here it deviates posteriorly. The second bend in this plane is noted at the level of the VIII-IX vertebrae, corresponding to the place where the esophagus passes through the diaphragm - here the esophagus deviates anteriorly. Along its course, the esophagus adjoins a number of organs. The cervical part of the esophagus with its posterior surface lies on the prevertebral plate, and the anterior surface is adjacent to the membranous wall of the trachea. From the sides, the common carotid arteries and recurrent laryngeal nerves closely approach the esophagus in this section. The thoracic part of the esophagus with its posterior surface also lies along the spine, and the upper third of the anterior surface is adjacent to the membranous wall of the trachea. Then, at the level of the IV-V vertebrae, the esophagus with its anterior surface is adjacent to the aortic arch, and below the latter it is adjacent to the posterior surface of the left bronchus, connecting to it using the underdeveloped bronchoesophageal muscle, m. bronchoesophageus. The paired muscle, non-constant, is a muscle-elastic extension attached to the posterior surface of the main bronchus. In the lower third, the esophagus touches the area of the pericardium corresponding to the left atrium and left ventricle, and, heading down, spirals around the aorta, passing into the abdominal part. The latter is covered in front by a portion of the left lobe of the liver. Along the lower part of the thoracic part of the esophagus, the posterior vagus trunk of the X pair is adjacent to its posterior surface, and the anterior vagus trunk is adjacent to the anterior surface.
The lumen of the esophagus is not the same. Throughout its entire length, it is customary to distinguish three narrowings and two expansions. The first narrowing is at the junction of the pharynx and the esophagus, the second is where the esophagus is adjacent to the aortic arch, and the third is at the point where the diaphragm passes through the esophageal opening. Between these narrowings there are two expansions. The wall of the esophagus has three membranes: mucous, muscular and adventitial (see Fig. 447, A; 490); the abdominal part is covered with a serous membrane. The mucous membrane, tunica mucosa, is covered with stratified squamous epithelium. The thickness of the mucous layer is formed by loose fiber and a developed muscular plate of the mucous membrane, lamina muscularis mucosae, consisting of smooth fibers, the role of which is to reduce the mucous membrane when the lumen of the esophagus decreases. On a cross section, the lumen of the esophagus has the appearance of a star-shaped fissure due to the compressed walls and well-defined longitudinal folds. The size of the folds is due to the significant development of loose connective tissue that forms the submucosa, tela submucosa. The latter lies between the mucous and muscular membranes. In the submucosa there are many vessels, glands of the esophagus, glandulae esophageae (Fig. 492), the ducts of which open on the surface of the mucous membrane, and single lymphatic follicles. The muscular layer, tunica muscularis, consists of two layers: internal - circular and external - longitudinal. In the intermuscular layer, in its loose connective tissue, there are vascular networks and nerve plexuses. In the upper third of the esophagus, the muscle layers are represented by striated muscles, which in the middle third become smooth; the lower third of the esophagus consists exclusively of smooth muscle fibers. The muscle layers are unevenly developed. Thus, the longitudinal layer is made up of fibers that separate in the upper part of the esophagus into the cricoesophageal tendon, tendo cricoesophageus, paired, which is attached to the lower edge of the plate of the cricoid cartilage of the larynx. Therefore, in the initial part of the esophagus there remains an area without a longitudinal layer. The circular layer of the wall of the esophagus in the upper sections is a continuation of the muscles of the pharynx, and below it passes into the circular and oblique fibers of the muscular wall of the stomach. In certain areas of the esophagus one can see an underdeveloped longitudinal layer lying inward from the circular one. At the level of the hilum of the lungs, the paired pleuroesophageal muscle, m. pleuroesophageus, consisting mainly of smooth muscle fibers. On the left, the muscle connects the aorta and esophagus with the mediastinal pleura at the level of the bronchial bifurcation, and on the right it departs from the lower third of the thoracic part of the esophagus and approaches the right mediastinal pleura. The adventitial membrane, tunica adventitia, is formed by loose connective tissue containing a small amount of elastic fibers. Through this membrane, the esophagus is fixed to other organs lying around it in the posterior mediastinum. The thickness of this membrane contains the main blood vessels that supply blood to the esophagus, lymphatic vessels that carry lymph from the walls of the esophagus, as well as the nerve trunks of the vagus nerves, which form plexuses here. Innervation: plexus esophageus (n. vagus and trancus sympathicus) is the source of powerful intramural plexuses of the esophagus. Blood supply: cervical part - rr. esophageales from a. thyreoidea inferior; chest part - rr. esophageales from aorta thoracica, abdominal part - rr. esophageales from a. gastrica sinistra and a. phrenica inferior sinistra. Venous blood flows from the cervical region into the v. thyreoidea inferior, and then in v. brachiocephalica; from the thoracic part - in v. azygos and v. hemiazygos; from the abdominal part - in v. gastrica sinistra, and then in v. portae. Lymph flows from the cervical part in the nodi lymphatici tracheobronchiales superiores et inferiores, paratracheales and paravertebrales; from the thoracic part - in the nodi lymphatici tracheobronchiales inferiores and mediastinales posteriores; from the abdominal part - into the anulus lymphatici cardii.
Structure of the human esophagus
The structure of the esophagus is divided into three sections:
- cervical is located behind the larynx, average length 5 cm - the most mobile part of the organ;
- thoracic, about 18 cm long, at the entrance to the diaphragmatic opening is hidden by the pleural layers;
- abdominal with a length of no more than 4 cm is located in the subdiaphragmatic region and connects to the cardia.
The organ is equipped with two sphincters: the upper one limits the return of food into the pharynx, the lower one blocks the return of gastric acid and food masses back.
The peculiarity of the organ is its anatomical narrowings:
- pharyngeal;
- diaphragmatic;
- bronchial;
- aortic;
- gastric.
The muscle layer - the basis of the organ wall - is designed in such a way that it allows the fibers to significantly expand and contract, transporting the food bolus. On the outside, muscle fibers are covered with connective tissue. The inside of the organ is lined with mucous epithelium, into which the lumens of the secretory ducts open. This structure allows for several important functions in the digestive process.
Achalasia of the human esophageal cardia
This is a chronic disease that is characterized by insufficient reflex relaxation of the esophageal sphincter or its absence, as a result of which intermittent symptoms of esophageal obstruction appear, which is caused by a narrowing of its section. The disease can develop at any age.
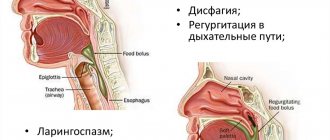
Symptoms of the disease
Dysphagia is the earliest and most permanent symptom, which has its own characteristics, for example, difficulty in passing food does not appear immediately, but after 2-4 seconds from the start of swallowing; the retention of the food bolus is felt by the patient not in the throat or neck, but in the chest; Dysphagia with achalasia cardia occurs when consuming both solid and liquid foods. In most cases, with achalasia cardia, the manifestations of esophageal dysphagia gradually intensify, although this process can last for quite a long time.
Regurgitation is the entry of undigested food back into the oral cavity, otherwise this symptom can be called regurgitation. Chest pain occurs in 60% of people with this disease.
Functions of the esophagus
In the human esophagus, structure and function are closely related, and the central nervous system plays the role of coordinator.
There are several main tasks:
- Motor – moving food and transporting it to the stomach. Motor activity is ensured by the work of skeletal muscles, which form the basis of the upper third of the wall of the esophagus. The gradual contraction of muscle fibers causes a wave-like movement - peristalsis.
- Secretory is due to the work of special glands. During passage, the food lump is abundantly moistened with enzymatic liquid, which facilitates transportation and starts the digestion process.
- The barrier, performed by the work of the esophageal sphincters, prevents food particles from entering the oropharynx and the respiratory tract.
- The protective effect is provided by the production of immunoglobulin by the mucous membrane of the esophagus, which has a detrimental effect on pathogenic microflora accidentally ingested by a person.
Methods for studying the esophagus and diagnosing its pathology are based on the characteristics of its structure and functioning. The organ is the initial link in digestion, and disruption of its activity causes a malfunction in the entire gastrointestinal tract system.
Physiological functions of the esophagus
The movement of food through the esophagus is the last phase in the complex mechanism that organizes the entry of the bolus of food into the stomach. The act of food passing through the esophagus is an active physiological phase that occurs with certain interruptions and begins with the opening of the entrance to the esophagus. Before the opening of the esophagus, there is a short period of delay in the act of swallowing, when the entrance to the esophagus is closed, and the pressure in the lower part of the pharynx increases. At the moment of opening of the esophagus, the food bolus is directed under pressure to its entrance and slips into the reflexogenic zone of the upper part of the esophagus, in which peristalsis of its muscular apparatus occurs.
The entrance to the esophagus opens as a result of relaxation of the pharyngo-cricoid muscle. As the food bolus approaches the cardia, the diaphragmatic opening of the esophagus also opens, partly reflexively, partly as a result of the pressure that the esophagus exerts on the food bolus in its lower third.
The speed at which food moves through the esophagus depends on its consistency. The movement of food is not smooth, but is slowed down or interrupted by stops as a result of the occurrence of zones of muscle contraction and relaxation. Typically, dense products are delayed for 0.25-0.5 s in the area of aortobronchial constriction, after which they are further advanced by the force of a peristaltic wave. Clinically, this narrowing is characterized by the fact that it is at its level that foreign bodies are more often retained, and with chemical burns, deeper damage to the walls of the esophagus occurs.
The muscular system of the esophagus is under constant tonic influence of the nervous sympathetic system. It is believed that the physiological significance of muscle tone lies in the tight coverage of the food bolus by the wall of the esophagus, which prevents air from entering the esophagus and entering the stomach. Violation of this tone leads to the phenomenon of aerophagia
- swallowing air, accompanied by swelling of the esophagus and stomach, belching, pain and heaviness in the epigastric region.
Esophagus length
The size of the organ is individual and depends on age, height, build and individual characteristics. On average, the length of the esophagus in an adult is 28–35 cm. Its weight depends on the total body weight and is on average 30–35 g.
The diameter varies depending on the department in question. The smallest lumen is observed in the cervical segment - about 1.7–2 cm. It reaches the largest diameter in the subdiaphragmatic part - 2.8–3 cm. Such data were established in a calm (collapsed) state.
Symptoms
Depending on the degree of cardia insufficiency, the symptoms of the pathology appear and intensify. You need to pay attention to them immediately in order to start treatment on time.
These include:
- frequent belching of air or sour;
- heartburn not associated with food intake;
- pain behind the sternum (similar to an angina attack) and in the epigastric region;
- nausea, vomiting (possibly with bile);
- dizziness and weakness during physical activity;
- rumbling in the intestines;
- severe night cough.
Frequent belching due to ongoing reflux and heartburn, regardless of the last meal, are the main symptoms on the basis of which insufficiency (chalasia) of the esophageal cardia is diagnosed.
To confirm the correctness of the diagnosis, instrumental methods are used: endoscopy, fluoroscopy, pH-metry, esophagomanometry. They are necessary because there may be too many or too few symptoms, and they are characteristic of several types of pathology at the same time. It is important to correctly differentiate them by establishing the correct diagnosis.
Sections of the esophagus
In the generally accepted classification, there are 3 sections of the human esophagus:
- Cervical. The upper border is the 6th cervical vertebra, the lower border is the 1st–2nd thoracic vertebrae. Its length varies between 5–7 cm. The segment is adjacent to the larynx and the upper part of the trachea, on both sides there are the lobes of the thyroid gland and the trunks of the recurrent nerves.
- Chest. This is the longest section of the esophagus, in an adult it is about 17 cm. In addition, this is the most complex topographic section, since it also contains: the aortic arch, the area of the nerve plexus and branches of the vagus nerve, and the division of the trachea into bronchi.
- Cardiac, otherwise called distal. The shortest segment, no more than 4 cm long. It is this segment that is susceptible to the formation of hernial sacs when passing through the diaphragmatic opening.
Some sources distinguish 5 sections of the esophagus:
- upper, corresponding to the cervical;
- chest;
- lower thoracic;
- abdominal;
- lower, corresponding to the cardiac segment.
In the topographic classification there is a division into segments according to Brombar, where 9 zones are distinguished.
general information
The human esophagus and stomach are two successively located sections of the gastrointestinal tract. The second one is below. The first is located in the area from the 6th cervical to 11th thoracic vertebrae. What is the structure of the human esophagus? It consists of three parts. The department includes the abdominal, thoracic and cervical zones. For clarity, a diagram of the human esophagus is presented below. The department also contains sphincters - upper and lower. They act as valves that ensure unidirectional passage of food through the gastrointestinal tract. Sphincters prevent the penetration of aggressive contents from the stomach into the esophagus, and then into the pharynx and oral cavity. There are also narrowings in the department. There are five of them in total. Two narrowings - pharyngeal and diaphragmatic - are considered anatomical. Three of them - bronchial, cardiac and aortic - are physiological. This is, in general, the structure of the human esophagus. Next, we will take a closer look at what the organ membranes are.
Anatomical and physiological narrowings of the esophagus
Constrictions are areas of the smallest diameter; they differ in anatomical and physiological. There are 5 natural constrictions in total. These are high-risk areas, since this is where obstruction occurs when a foreign object enters or food accumulation occurs during dysphagia (a functional disorder of the passage of food).
Anatomical narrowings are determined both in the body of a living person and during a pathological examination. There are 3 such areas:
- cervical region at the lower edge of the pharynx;
- in the thoracic segment – the place of contact with the left bronchial tree;
- transition to the distal section when crossing the diaphragmatic window.
Physiological narrowing of the esophagus is caused by the spastic action of muscle fibers. These areas can only be detected during a person’s lifetime; these are the aortic and cardiac segments
Cardiospasm
This condition accompanies the expansion of the esophagus. This anomaly is characterized by a gigantic increase in its cavity with morphological changes in the walls against the background of a sharp narrowing of its cardiac part - cardiospasm. Enlargement of the esophagus can develop as a result of a variety of external and internal pathogenic factors, embryogenesis disorders, and neurogenic dysfunctions leading to atony.
Serrated line of esophagus
Z-line of the esophagus - the border determined by the endoscopic method is located at the junction of the esophagus and the stomach. Normally, the inner layer of the organ is stratified epithelium, which has a pale pinkish color. The gastric mucosa, represented by columnar epithelium, is distinguished by its bright red color. At the junction, a line resembling teeth is formed - this is the demarcation of the epithelial layer and the internal environment of the organs.
The outer boundary of the dentate line is the gastric cardia - the confluence of the esophagus. The outer and inner boundaries may not coincide. Often the dentate line is located between the cardia and the diaphragm.
Anatomy of the human esophagus
The section has a wall built from the mucosa, submucosa, as well as adventitial and muscular layers. The latter in the upper part of the section is formed by striated fibers. In approximately 2/3 (counting from the top), the structures are replaced by smooth muscle tissue. There are two layers in the muscular layer: the inner circular and the outer longitudinal. The mucous membrane is covered by squamous stratified epithelium. In the thickness of this membrane there are glands that open into the lumen of the organ. The mucous membrane is of the cutaneous type. Flat stratified epithelium lies on fine connective fibers. This intrinsic layer of the shell consists of collagen structures. The epithelium also contains connective tissue cells and reticulin fibers. The proper layer of the membrane enters it in the form of papillae. In general, the anatomy of the human esophagus is quite simple. However, it is not so much important as the tasks that are implemented in this section of the gastrointestinal tract.
Blood supply to the esophagus
The blood supply to the esophagus depends on the general circulatory system of the segment.
- In the cervical region, blood circulation is provided by the thyroid artery and vein.
- The thoracic region is supplied with blood by the aorta, bronchial branches and azygos vein.
- The abdominal part is supplied by the diaphragmatic aorta and gastric vein.
Lymph flow is carried out towards the following large nodes:
- cervical and tracheal;
- bronchial and paravertebral;
- large abdominal lymph vessels.
Structure and functions of the esophagus
The esophagus is a hollow organ that looks like a narrowed and movable tube up to 30 cm long, connecting the larynx and stomach.
The rudiments of the esophagus appear already in the 1st month of embryo formation, and by birth it is practically formed, the diameter of its gap is up to 0.8 cm, and its length is up to 15 cm.
Location
Experts distinguish between the beginning and end of the esophagus and correlate it with visible and permanent bone formations in the skeleton:
- starts from the 6th cervical vertebra;
- ends near the 10-11 thoracic vertebra.
It is customary to distinguish 3 departments of the organ in question:
- Cervical. Above is the lower part of the cricoid cartilage, below is the jugular notch of the sternum. The length of this section is small and is approximately 50 mm in adulthood. Descending downwards, the esophagus bypasses the windpipe, and from the sides there are the carotid arteries and recurrent nerves.
- Chest. It departs from the jugular notch and ends approximately near the 10-11 thoracic vertebrae in the area where the esophagus exits the sternum cavity through the lumen in the diaphragm. The longest section of the organ in question. It is closely interconnected with the rest of the chest organs: the trachea, aorta, left bronchus, pericardium with the heart are located in front of it; behind it is the thoracic lymphatic tract, spine, azygos vein; on the side – pleura, vagus nerve.
- Abdominal. It is the shortest section, approximately 20 mm long. It begins from the lumen of the diaphragm, and ends at the point of transition into the stomach.
Innervation
Ensuring the functionality of the organ occurs due to the work of both types of nervous regulation: sympathetic and parasympathetic. The connections of nerve fibers form plexuses on the anterior and posterior surfaces of the esophagus. The thoracic and abdominal regions are more dependent on the work of the vagus nerve. The innervation of the esophagus in the cervical region is provided by the trunks of the recurrent nerves.
The nervous system regulates the motor function of the organ. The greatest response is given by the pharyngeal and gastric zones. This is the location of the sphincters.
Prevention
Humans are designed in such a way that preventing disease is not about them. Most often, you have to first treat the disease, and even in an advanced form, and then think about prevention. Diseases of the esophagus and the entire gastrointestinal tract are easy to prevent with the help of proper, moderate nutrition, normal drinking regimen, active lifestyle, giving up bad habits, and timely, regular medical examination. But from theory to practice in matters of such prevention there is an abyss.
I read somewhere that the fear of not having enough to eat and eating for future use is a genetically embedded fear in the subconscious of the descendants of those generations who experienced long times of famine. And, nevertheless, when it comes to health and quality of life, it is worth making an effort and gradually correcting eating behavior by reducing portions and giving up unhealthy foods. It is even more difficult to avoid frequent stress and maintain emotional calm. But these are important factors in maintaining the health of many organs and systems of the human body. This means that issues of strengthening mental health and the nervous system also need to be given constant attention.
We recommend: What exercises can you do to strengthen the diaphragm with GERD?
X-ray anatomy of the esophagus
During X-ray irradiation, the esophagus does not produce a shadow, so studies are carried out using contrast agents. X-ray anatomy of a healthy esophagus reveals a shadow in the form of a band of varying diameters depending on the section in question. In the supradiaphragmatic region, the contrast agent appears as a pear-shaped extension. This is due to the fact that when inhaling, the progress of the barium solution, as well as the food mass, is interrupted.
Normally, the esophagus has a clear contour and smooth boundaries. The speed of peristalsis is 3–5 cm per second. In the presence of dysphagic disorders or ingestion of a foreign body, an x-ray gives a clear idea of the location and scale of the situation.
Varicose veins of the esophagus
Depending on the symptoms of the disease, the patient may be monitored in the gastroenterology or surgery department. The task of the gastroenterologist is to treat the underlying disease and prevent the development of bleeding. For this, the patient receives hemostatic drugs, antacids, and vitamins. Prevention of esophageal reflux is mandatory. Strict adherence to proper diet, rest and physical activity is recommended.
If bleeding develops, hemostatic therapy is carried out - calcium supplements, vitamin K, and fresh frozen plasma are prescribed. An emergency esophagoscopy is performed to determine the source of hemorrhage and endoscopic clipping of the bleeding vein, application of an adhesive film and thrombin, and electrocoagulation of the vessel. To stop bleeding, a Blackmore probe is used - it has special balloons that, when inflated, block the lumen of the esophagus and compress the vessels. However, even after these manipulations, in 40-60% of cases a positive effect is not achieved.
After stopping the bleeding and stabilizing the condition, surgical treatment methods are used - their effectiveness is much higher than that of conservative methods. Typically, surgical treatment consists of placing shunts between the portal vein and the systemic bloodstream, due to which the pressure in the portal vein is reduced and the likelihood of bleeding becomes minimal. The safest and most popular method is the endovascular transjugular method of applying a shunt (access through the jugular vein); portacaval and splenorenal anastomoses are also applied, the removal of the spleen, ligation of the azygos and portal veins, the splenic artery and suturing or embolization of the esophageal veins are practiced.
Forecast and prevention of varicose veins of the esophagus
The prognosis of the disease is unfavorable - esophageal varicose veins are incurable; when this disease appears, all measures must be taken to prevent the progression of the pathology and fatal bleeding. Even bleeding that occurs for the first time significantly aggravates the prognosis, reducing life expectancy to 3-5 years.
The only method of preventing esophageal varicose veins is the prevention and timely treatment of diseases that provoke this pathology. If there is a history of liver disease, which can lead to cirrhosis and increased portal vein pressure, the patient should be regularly examined by a gastroenterologist to promptly detect dilation of the esophageal vessels.
If varicose veins have formed, you should follow a strict diet: food should be steamed or boiled, it is advisable to puree food and not eat dense foods in the form of large pieces. You should not take dishes that are too cold or hot, coarse and hard foods to prevent injury to the esophageal mucosa. To prevent reflux of stomach contents into the esophagus, the head of the bed is raised during sleep. To avoid bleeding, it is recommended to avoid heavy physical activity and heavy lifting.
Bends
Despite the comparison with a “tube,” the esophagus is a fairly mobile organ. Several bends and displacements are visible in its location, which is due to its proximity to vital organs. In the initial position, it is determined along the midline, repeating the location of the spinal column. At the level of the 3rd thoracic vertebra, a shift occurs to the right side, bypassing the area of the heart. When meeting the aorta, the esophagus bends anteriorly. Passing through the diaphragmatic window, another forward shift is observed.
The bends of the esophagus, its elasticity and mobility allow surgical intervention to be performed with minimal damage to the functionality of the organ itself and those adjacent to it.
Anatomy and physiology of the esophagus
Home > For patients > Esophagus > Anatomy and physiology of the esophagus
The esophagus (Latin esophagus - esophagus) is a hollow muscular tube connecting the pharynx to the stomach. The wall of the esophagus has a three-layer structure: the outer layer is adventitia, the middle layer is muscular, and the inner layer is mucosa. Its thickness is only 3-4 mm. The length of the esophagus of an adult reaches an average of 24-25 cm, the width of the lumen is 2.0-3.0 cm.
In the neck region, the upper part of the esophagus is located behind the trachea. The physiology of the esophagus is such that the place of transition of the pharynx into the esophagus in an adult corresponds to the level of the VI cervical vertebra or the lower edge of the cricoid cartilage. The esophagus then descends along the spine into the chest cavity, lying deep in the posterior mediastinum. The trachea and left main bronchus are adjacent to it in front, and the aorta and spine are located behind it. And finally, through its own opening in the diaphragm, the esophagus penetrates into the abdominal cavity, where it almost immediately passes into the cardiac part of the stomach. The junction of the esophagus with the stomach is projected at the level of the XI thoracic vertebra (anatomical cardia). Accordingly, the topography of the esophagus distinguishes three sections: cervical (5-8 cm), thoracic (15-18 cm) and abdominal (1-3 cm).
The esophagus has three permanent narrowings, called “physiological”. Upper (14 mm in diameter) - at the level of the pharyngoesophageal junction, middle (16 mm in diameter) - in the posterior mediastinum at the level of the tracheal bifurcation in the place where the aorta and left main bronchus are adjacent to the esophagus, lower (16-19 mm in diameter) - corresponds to the esophageal diaphragm hole. Physiological narrowings of the esophagus can become a place for foreign bodies to get stuck, causing strictures and diverticula.
The function of the esophagus is to move the bolus of food from the pharynx to the stomach. In its provision, the main role is played by the muscles of the esophagus, which has its own peristaltic activity. After food enters the esophagus, the pharyngoesophageal sphincter closes, and the cardiac sphincter ( physiological cardia ) relaxes. Regulation of the function of the cardia is carried out both by the central nervous system (the so-called pharyngeal-cardiac reflex) and peripheral (centers in the cardia itself and the distal third of the esophagus). In addition, gastrointestinal hormones influence the tone of the cardia.
Other areas: peptic ulcer of the stomach and duodenum, gastric surgery, symptoms of hiatal hernia, hernia of the anterior abdominal wall, umbilical hernia in children.
Wall structure
The structure of the esophageal wall is focused on performing basic functions. Histologically, four cellular layers are distinguished:
- internal epithelium;
- submucosa;
- muscle layer;
- adventitia.
Muscle tissue makes up the bulk of the wall of the esophagus. She is different. In the upper and thoracic region it is represented by striated muscles with a ring arrangement, which ensures efficient transportation of food. Closer to the abdominal segment, replacement occurs with smooth muscles that are prone to stretching.
In the submucosal layer there are endocrine glands that produce secreted fluid into the organ cavity. The integumentary tissue (adventitia) is represented by the pleural layers in the thoracic region and the peritoneum in the cardiac part of the esophagus. The diaphragmatic ring and the junction with the stomach are completely hidden by the adventitia.
STRUCTURE OF THE ESOPHAGUS
In Fig. 1 shows the esophagus. The human esophagus (E) is a tubular organ 25 cm long, located between the laryngeal part of the pharynx (G) and the stomach (G). To show the structure of the human esophagus in detail, the organ is cut into levels A, B and C and the resulting sections are presented in perspective in Fig. 2. To visualize the organization of the muscular lining of the esophagus, part of its wall is removed, and some structures are drawn above the level of the section.
=»»>
The membranes of the esophagus replace each other in the following order:
• the mucous membrane (SM) consists of stratified squamous non-keratinizing epithelium (E), which is attached to the underlying lamina propria (LP) with the help of numerous connective tissue papillae. A layer of smooth muscle cells arranged longitudinally, the so-called muscularis mucosa (LPM), is drawn partially above the level of the slice. Thanks to this layer, the mucous membrane forms longitudinal folds (C);
• the submucosa (SC) consists of loose connective tissue, which contains many venous vessels and scattered mucous glands of the esophagus (EG) with excretory ducts (arrowheads) opening on the surface of the mucous membrane;
• muscularis propria (MT) - a layer of muscle tissue organized in two layers: internal circular and external longitudinal, which intersect approximately at right angles.
At level A, i.e. in the upper third of the esophagus, the muscular coat consists exclusively of striated muscle fibers united in bundles. The internal circular (IC) and external longitudinal (LP) muscle layers have a slightly spiral course. Along the entire length of the esophagus, between the layers there are numerous ganglia of the intermuscular nerve plexus (NS). These ganglia are responsible for controlling the peristalsis of the organ.
At level B, smooth muscle bundles (SM) are located among striated muscle fibers (MF).
At level C, only smooth muscle tissue forms the muscularis propria. At this level, the submucosal veins form the submucosal venous plexus;
• outer (adventitial) membrane (UT) - a thin layer of loose connective tissue surrounding the esophagus and connecting it to neighboring organs.
The short intra-abdominal segment of the esophagus, 2 cm long (see arrow in Fig. 1), has a subserosal base and a serosa instead of an adventitia. This area is not covered in this table.
The 1:1 image scale is typical only for the upper surface of slice A.
Esophageal epithelium
The basis of the inner wall is made up of stratified squamous non-keratinizing epithelium. It originates in the pharynx and continues to the dentate line. The mucous membrane consists of 20–22 layers of cells, the total thickness of which is about one and a half centimeters. The esophagus is lined with epithelium, which differs in structure from the mucous tissue of the gastrointestinal tract. Regular reflux of stomach contents due to reflux can cause changes in the mucous layer and the development of metaplasia.
The esophagus is an important link in the transportation, processing and absorption of nutrients. Disruption of its functioning affects the entire digestive system. In a healthy body, some topographical features are possible that do not affect the overall functionality of the body.
Anatomy
The wall of the esophagus consists of a mucous membrane (covered with stratified epithelium), a submucosa (in which mucus-producing glands are scattered), a muscular layer (consists of an inner and outer layer) and a connective tissue membrane.
On the one hand, the structure of this organ is not so complex, but it is not so much the structure that is important as the functions that the esophagus performs.