In pathologies of the digestive tract, a significant proportion is due to diseases of the esophagus, the symptoms and treatment of which depend on the nature of the process. Essentially, the esophagus is a narrow tube of muscle fibers, the sequential contraction of which evacuates food into the stomach. In the upper and lower parts of this tube there are ring-shaped muscle sphincters - a kind of valves that prevent the reverse movement of nutritional masses. Pathologies of the esophagus and disruption of the well-functioning mechanism for transporting food lead to a malfunction of the entire system.
Accepted classification of esophageal diseases
For diseases of the esophagus, classification involves dividing pathologies into groups with similar etiology, nature of development, type of danger and approach to treatment.
Let's look at the groups and the violations related to them.
| Group | Similar features | Pathologies |
| 1 | Anomalies of intrauterine development |
|
| 2 | Diseases leading to functional disorders |
|
| 3 | Inflammatory diseases |
|
| 4 | Vascular changes |
|
| 5 | Changes at the cellular level |
|
| 6 | Traumatic injuries |
|
Diseases of the esophagus: symptoms and signs
Regardless of the etiology of the disease of the esophagus, symptoms and signs characteristic of a specific organ allow us to establish the exact localization and direction of diagnosis. There is a triad of specific manifestations that are found in all groups of diseases:
- Heartburn - burning sensations in the epigastrium or retrosternal region are caused by the contents of the stomach entering the esophageal mucosa. The culprit is a weakened cardiac sphincter. Heartburn worsens when consuming large amounts of food, consuming fried or smoked foods, or when bending over or lying down. Belching is the return of air through the oral cavity.
- Feeling of a “lump”, heaviness in the esophagus, difficulty swallowing. Most often, it is difficult for dense foods to pass through, but sometimes there is difficulty passing liquids.
- Pain when swallowing or moving food masses. Moreover, pain in the area of the organ can occur either episodically, for example, after ingestion of food, or constantly.
Diseases of the esophagus have separate symptoms and endoscopic manifestations for each group of pathology.
Esophageal ulcer
Esophageal ulcer: symptoms and treatment
An esophageal ulcer is an area of the mucous membrane damaged by the ingress of gastric juice.
Ulceration can be acute or chronic. A mucosal defect occurs as a result of gastroesophageal reflux, so treatment is aimed at eliminating the causes of gastric juice reflux into the esophagus. Sometimes the disease can also be associated with pathology of the esophageal vessels. The prognosis for maintaining working capacity is favorable; the disease does not pose a threat to the patient’s life, but reduces its quality. An ulcer of the esophagus is treated by a gastroenterologist or therapist.
Causes of the disease
There are symptomatic and peptic (true) ulcers.
Causes of peptic pathology:
- Gastroesophageal reflux disease (GERD).
- Diaphragmatic hiatal hernia.
- Stomach operations.
- Systemic scleroderma.
- Insufficiency of the cardiac part of the stomach.
Diseases of the digestive tract, leading to a decrease in the tone of the gastric wall.
Symptomatic ulcers are less common than peptic ulcers and are diagnosed in the absence of GERD. Possible causes of the pathology:
- Viral infection (tuberculosis, HIV, cytomegalovirus, herpes, etc.).
- A tumor of the esophagus that causes mechanical compression of the organ.
- Autoimmune processes (Behcet's syndrome, Sjögren's disease).
- Deep burns of the mucous membrane, sepsis.
- Prolonged use of a gastric tube.
The causes of acute esophageal ulcers are most often operations and illnesses with profuse vomiting. Chronic pathology develops against the background of other systemic health problems.
Symptoms of esophageal ulcers
The disease has a characteristic clinical picture. Symptoms of esophageal ulcers include chest pain, heartburn, impaired swallowing function, and nausea. As a result of malnutrition, the patient loses weight. When the defect is localized near the cardiac sphincter, pain in the esophagus is often confused with symptoms of angina pectoris. If ulceration exists for a long time, narrowing of the lumen and frequent regurgitation of food immediately after eating are possible.
Severe heartburn is one of the characteristic symptoms of an esophageal ulcer in the early stages of development. The reflux of acidic gastric juice is high. Many patients report relief from heartburn only after vomiting.
If left untreated, the defect grows and complications arise. The most dangerous condition is perforation of the esophageal wall into the mediastinum (mediastinitis), into the abdominal cavity (acute abdomen condition), into the pleural cavity (pleurisy), into the aorta (rarely, profuse bleeding).
Diagnosis of esophageal ulcer
You should consult a doctor immediately after the first symptoms appear. Early diagnosis of ulcers is the key to successful treatment.
The patient is prescribed a comprehensive examination:
- X-ray with contrast. The image shows signs of ulceration of the mucous membrane, and concomitant pathologies are determined: hiatal hernia, esophagitis.
- Endoscopy. The main method for diagnosing esophageal ulcers. Using a video camera, the doctor examines the esophageal mucosa and performs a marginal biopsy for differential diagnosis of cancer. Based on the results of endoscopy, the type of ulcer is determined: focal (up to 10 mm in diameter, without changes in peristalsis and motility), deep (up to 10 mm, high edges), flat-infiltrative (the borders are hyperemic, fibrin is at the bottom of the defect).
- Daily measurement of acidity. The examination results suggest GERD.
- General blood analysis. Data are needed to determine comorbidities.
- Coprogram. A stool test is ordered to check for occult blood.
Treatment of esophageal ulcers
Diet
The patient's meals should be divided, in small portions, without overeating. It is recommended to adhere to therapeutic diet No. 1a or No. 1b according to Pevzner, but the doctor can make adjustments to the menu taking into account the characteristics of a particular clinical case. All food should be boiled or steamed. Avoid spicy, sour, fried foods, and any food that can cause irritation to the mucous membranes.
Drug treatment
The patient is prescribed a complex of drugs aimed at protecting and healing the mucous membrane:
- Antacids that reduce the activity of H+ ions.
- Drugs that normalize the acidity of gastric juice.
- Prokinetics, which increase the tone of the gastric wall, eliminate congestion.
- Antibacterial drugs (if H. Pylori was detected).
- Vitamins and restoratives.
Soothing herbal preparations if the ulcer is associated with prolonged stress.
Diagnosis and treatment of esophageal ulcers in Nizhny Novgorod
We invite you to undergo a full examination at the modern Alfa Health Center clinic. We use the latest digital equipment and our own laboratory complex to accurately diagnose esophageal ulcers. You can make an appointment with a doctor by calling the number listed on the website.
Functional disorders: clinical picture
Functional diseases of the esophagus are pathologies that lead to disruption of the main function of the organ - motor:
- Achalasia is a chronic spastic condition of the lower sphincter, which prevents food from leaving the esophagus completely.
- Dyskinesia is a disruption of the coordinated functioning of muscle fibers, caused by a disorder in the regulatory nervous system.
Main symptoms of the disease:
- dysphagia;
- sensation of a lump in the throat or chest area;
- feeling of fullness;
- air burp.
Symptoms intensify when consuming foods rich in fiber or during nervous stress. The pain in the chest area is pressing, reminiscent of an angina attack, so the disease requires differential diagnosis.
Inflammatory diseases and their signs
Chronic esophagitis is most common in this group. Prolonged irritation of the lower esophagus by gastric contents leads to the development of an inflammatory process.
Main features:
- heartburn that gets worse in a certain body position;
- pain during swallowing movements;
- frequent painful hiccups;
- sour belching.
In the upper sections, the cause of inflammation is catarrhal phenomena in the pharynx or candidiasis. In this case, the following symptoms are added to the listed symptoms:
- heaviness when moving food masses;
- soreness and burning in the retropharyngeal space and behind the sternum;
- the occurrence of erosions on the esophageal mucosa.
Candidal esophagitis: symptoms and treatment
Crohn's disease of the esophagus and stomach is considered a chronic inflammatory disease. The pathology has a genetic predisposition and can affect any part of the digestive tract. Endoscopically, characteristic signs are revealed - small ulcers, which are clinically manifested by episodic bleeding. Laboratory tests may reveal anemia.
Diseases of the esophagus and their symptoms
Motility disorders of the esophagus include diseases such as achalasia cardia , esophageal spasm of the esophagus , peptic esophagitis , chalasia cardia and diaphragmatic hernia . These diseases have slightly different course patterns and symptoms.
Achalasia cardia , or cardiospasm, is a neuromuscular disease. This is a violation of the reflex opening of the lower esophageal sphincter during the passage of food. The reasons for the development of this disease of the esophagus are not known; it manifests itself at the age of 20-40 years, more often in women. Complications of this disease are most often caused by prolonged retention of food in the esophagus. In adults, a common complication is inflammation of the esophagus, which in turn can cause cancer of both the esophagus itself and the upper part of the stomach. Children more often experience complications such as bronchopneumonia, lung abscesses and other respiratory diseases caused by food getting into them.
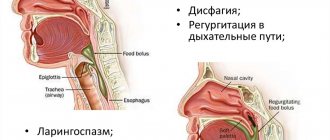
Symptoms of achalasia are triadic. The first manifestation of this disease of the esophagus is difficulty swallowing, or dysphagia . This symptom can occur suddenly or gradually, intensifying after nervous excitement. In some cases, paradoxical dysphagia is observed, when hard and dense foods pass normally, but liquids do not. Swallowing problems may also depend on the temperature of the food. The second symptom of achalasia is regurgitation , which occurs when the esophagus is full, when a sharp muscle contraction occurs. The third symptom is pain caused by spasm of the esophageal muscles when it is full. The pain behind the sternum goes away after food passes into the stomach. These symptoms are also accompanied by nausea, belching of air , burning in the esophagus, and increased salivation.
Esophageal spasm - spasm of the walls of the esophagus, not accompanied by dysfunction of the lower alimentary sphincter, occurs due to a nervous disorder. Esophagospasm most often occurs in middle-aged and elderly men, and may also be a symptom of other digestive tract disorders.
A symptom of esophageal spasm of the esophagus is chest pain, which is often mistaken for manifestations of angina pectoris . Pain can occur not only during meals, but also in the interval between meals. They come in varying intensity and duration. In addition to pain, this disease is characterized by a paradoxical swallowing disorder; the inconstancy of this symptom distinguishes esophageal spasm from other diseases and neoplasms of the esophagus.
Peptic esophagitis , or reflux esophagitis of the esophagus, is caused by insufficiency of the lower alimentary sphincter, which leads to the reflux of stomach contents back into the esophagus. Chalazia cardia has the same course, but it is more often caused by hiatal hernia. Due to such emissions of gastric juice, bile, and pancreatic juice, the mucous membrane of the esophagus suffers. Inflammation and ulcers occur, with scarring of which the esophagus narrows. This disease of the esophagus proceeds very slowly, in frequent cases it can be found in infants.
Symptoms of reflux esophagitis are burning behind the sternum, heartburn, pain, belching. Some symptoms worsen when bending over, lying down, smoking or drinking alcohol. Belching can cause aspiration pneumonia. This happens when gastric contents enter the respiratory tract, especially during night regurgitation, which is accompanied by coughing. Complications of the disease may include bleeding and scarring.
Diaphragmatic hernia is the movement of an organ from the abdominal cavity into the chest cavity. Hernias can be congenital, acquired or traumatic defects; most often, patients experience hiatal hernias; they can be sliding or paraesophageal . This disease has very few symptoms. The main symptoms of a diaphragmatic hernia are anemia and hidden bleeding.
Benign tumors of the esophagus grow slowly and are practically asymptomatic. Most often they are discovered by chance; in some cases, the patient may experience an increasing difficulty in swallowing, which develops over several years.
Unlike benign tumors and cysts, esophageal cancer has more pronounced symptoms and is diagnosed many times more often than other esophageal diseases. Cancer accounts for 60-80% of all diseases of the esophagus, it is the sixth most common disease at the age of 50-60 years, and is more common in men of this age group who abuse smoking and alcohol. Here are a few more reasons that cause esophageal cancer: complications of impaired motility of the organ, namely achalasia, Barrett's esophagus, papillomas and scars, which can also occur after a burn of the esophagus with caustic substances.
First, esophageal cancer manifests itself as a feeling of discomfort and chest pain in the patient, dysphagia, increased salivation, and weight loss. For the first one or two years, symptoms of esophageal cancer are practically not observed, until the tumor begins to narrow the esophagus, dysphagia gradually increases, and pain intensifies.
Vascular pathologies
Signs of vascular disease of the esophagus are often low-contrast at the initial stage. The patient may experience periodic general symptoms of malaise. But varicose veins are dangerous due to sudden bleeding.
How does a person feel:
- aching generalized pain in the chest;
- dryness and sore throat;
- salty taste of saliva.
Without treatment, varicose veins can last a long time, for years. Factors that provoke bleeding include heavy lifting, high fever due to colds, and trauma to the esophagus.
Clinical manifestations and symptoms of neoplasms
About 40% of esophageal diseases are tumors, more than half of them are precancerous diseases of the esophagus and benign formations.
Benign processes
Formations are formed from tissues inherent in a given organ:
- adenoma is based on glandular epithelial cells;
- leiomyoma is formed from muscle tissue;
- formations that are not capable of degeneration include polyps and cysts.
Benign diseases of the esophagus develop slowly, without manifesting themselves for a long time. Symptoms appear when the tumor, reaching a significant size, disrupts the transport of food. The person begins to be bothered by the sensation of a foreign object behind the sternum, discomfort when swallowing, and nausea after eating.
Borderline conditions – precancer
Precancerous pathologies include the disease Barrett's esophagus. The exact cause has not been established, but the condition occurs against the background of chronic reflux disease. Systematic irritation of the esophageal mucosa by gastric contents leads to the replacement of the esophageal epithelium with cells characteristic of other parts of the gastrointestinal tract (stomach or intestines). Metaplasia occurs - a borderline condition that, under favorable conditions, can develop into a malignant tumor.
Main patient complaints:
- constant heartburn;
- pain of unclear localization;
- tickling and dry cough;
- change in voice timbre.
Malignant tumors
Cancers of the esophagus can develop either as a consequence of the disease described above or independently. They are distinguished by long (up to 2 years) painless development; symptoms appear when the tumor reaches a significant size. Dysphagia appears - a violation of the act of swallowing and passage of the food bolus into the stomach.
First, difficulties arise with the promotion of solid food, then liquid food. A characteristic symptom is the sensation of a foreign body when swallowed. At a late stage of development, pain occurs: generalized, radiating to the scapula or shoulder. The general condition worsens: there is a sharp loss of weight, apathy, and weakness. People who abuse alcohol and nicotine are more at risk of developing cancer.
Congenital abnormalities
Congenital anomalies are associated with impaired intrauterine development, therefore the following diseases of the esophagus are more often detected in children in the newborn period:
- Atresia is characterized by fusion of a section of the esophagus or its incomplete formation. Often combined with other developmental pathologies. It is detected in the first hours of life, since the child cannot eat, and milk pours out.
- Diverticula are formations in the form of a sac in the thickness of the esophageal wall. Leads to retention of food in this “pouch” and compression of the lumen of the esophagus. Characteristic signs: belching rotten food, difficulty swallowing, the presence of a swollen area on the neck. With esophageal diverticulum, there is no pain reaction syndrome in the first stages of the disease. Pain and complications manifest in the third stage of the disease.
- Congenital stenosis develops due to hypertrophy of muscle tissue or compression of the esophagus by neighboring organs. It is detected in the first hours of a baby’s life, as food does not pass well through the esophageal tube and pours out through the nose. The child is choking and coughing.
Diagnostic stages
A preliminary diagnosis is made by a doctor based on clinical data. But basic and accurate information is provided by instrumental examination methods.
- X-ray diagnostics is a long-proven effective and simple method. To check the patency of the esophageal tube, a radiopaque substance is used - barium sulfate or other contrasts.
- Ultrasound is also a widely used method for detecting stenoses, formations, and tissue ruptures.
- CT is an examination using x-rays that gives a complete picture of the organ in three dimensions.
- MRI – allows you to create a visual image of an organ based on reflected radiation. Vascular MRI is used when esophageal varices are suspected.
- Endoscopic diagnosis is the most accurate method for detecting pathology. Allows you to see the changed mucosa and assess the degree of the disease; it is used if esophagitis, Barrett's disease, or mucosal ulcers are suspected.
- Manometry evaluates muscle functionality and sphincter pressure.
- Impedancemetry allows you to assess the pH environment of the esophageal mucosa and draw a conclusion about the refluxed contents. Provides information about esophageal peristalsis.
The purpose of diagnostic methods goes from simpler and harmless to more complex. Suspicion of malignant formations requires special care.
Diagnostics
Diseases of the stomach and esophagus are diagnosed using various methods using high-tech equipment. The necessary information about the course and causes of the disease is obtained by applying the following procedures and techniques:
- X-ray examination - contrast fluoroscopy. X-rays are taken before and after the administration of a contrast agent (barium sulfate). Using this method, it is possible to characterize the position of the esophageal tube in the chest, its size, the diameter of the internal canal, the general condition of the walls, and the filling of the organ. The images reveal the reasons for the difficulty in passing food particles and deformation. Provocative tests are carried out - fluoroscopy is done in standing, lying and bending positions. Using this method, you can diagnose gastroesophageal reflux, paraesophageal hernia, polyps, diverticula, and ulcers.
- Esophagoscopy. An endoscopic procedure is performed on an empty stomach using a fibroesophagoscope in a specially equipped room. A targeted biopsy is performed and foreign objects are removed. Anesthesia is first used, and the patient is placed on a special table. Using the device, the mucous membrane is examined for inflammation and erosion. The size and position of the affected area are noted, and a piece of tissue is cut off from it (a biopsy is performed). Next, the resulting material is examined using a microscope, describing individual cells. This method allows you to establish obstruction of the esophagus in any area or non-opening of the sphincters. If there are scars on the walls of the organ, the lumen of the esophageal tube must be expanded using rigid or flexible rods. Esophagoscopy helps to establish the causes of dysphagia, diagnose tumors, and detect foreign bodies in the cavity.
- Esophageal pH-metry. A pH probe is used to record the acid-base balance at the bottom of the tube. Since values can fluctuate during the day, the study is carried out throughout the day. The results are processed using a computer. The nature of gastroesophageal reflux is revealed. It can be acidic (gastric), alkaline (pancreatic) or bile. The duration of this phenomenon is recorded.
- Computed tomography. Used to diagnose tumor diseases. At the same time, the condition of nearby organs, blood and lymphatic vessels is noted.
- Functional X-ray diagnostics. It is used for negative changes in the motility of the muscles of the esophageal tube, increased or decreased tone of the sphincters.
- Esophagotonocymography, esophagomanometry. Complex research methods using probes. By measuring the pressure in its different parts and in the area of the sphincters, areas with impaired tone are found. Indicators at rest and during swallowing are recorded.
- Functional testing for the diagnosis of gastroesophageal reflux. Includes Stepenko test, Baker and Bernstein acid test, reflux acid test. The stomach is probed using methylene blue dye.
- Radioisotope research. The 32P isotope helps to diagnose malignant tumors of the esophagus.
Article on the topic: Symptoms and signs of polio in children and adults - prevention and vaccination
What is found during endoscopic examination
Diseases of the esophagus: symptoms and signs of the disease are clearly reflected during endoscopy.
With esophagitis: hyperemic and swollen mucosa, small, easily bleeding ulcerations are possible.
With Barrett's syndrome, there is a clear distinction between healthy pale pink mucosa and bright red dysplasia.
The study determines the clear boundaries of tumors growing into the lumen of the esophagus, the presence of submucosal formations and foreign bodies.
With achalasia, a spastically closed cardiac sphincter and an enlarged portion of the esophagus above it are visible.
When the lumen of the organ narrows, the passage of the endoscope is difficult, but no changes in the mucous membrane are observed.
Causes and course of the disease
Foreign bodies in the esophagus occur in almost all age categories.
This mainly happens when a person eats very hastily, talks while eating, or has the habit of holding any objects in the mouth. Quite often, foreign bodies of the esophagus occur in people who have low sensitivity of the oral mucosa due to the fact that they wear dentures, as well as in elderly people who do not have teeth. In some cases, foreign bodies enter the esophagus from the respiratory tract and stomach. Foreign bodies found in the esophagus are varied, but most often they are fish bones, buttons, badges, coins, etc. Children often come across parts of children's toys, coins, etc.
A foreign body can slip through the esophagus into the stomach or get stuck in the lumen of the esophagus. Whether a foreign body remains in the esophagus depends on its size, nature and shape, consistency, as well as the presence of pathological changes in the lumen of the esophagus.
Most often, foreign bodies get stuck in the cervical esophagus. This happens much less frequently in the thoracic esophagus.
Treatment options
There is no universal treatment method for all pathologies of the esophagus. The vastness of the etiology and development of diseases implies an individual approach to therapy:
- For inflammation, antacids (protect the mucous membrane from the aggressive effects of acid thrown from the stomach) and decongestants are used.
- In case of achalasia in the initial stage, bougienage and expansion with special balloons are prescribed.
- Diverticula are sutured surgically.
- Strictures and adhesions after burns are dissected.
- In the treatment of Barrett's pathology, innovative methods of radiofrequency ablation and argon coagulation of the affected mucosa are used.
Damage to the esophagus as a result of trauma and extensive tissue ruptures require surgical intervention, in some cases plastic surgery.
Treatment with folk remedies does not provide complete healing, but can maintain the body in a state of remission. This treatment is aimed at maintaining a normal level of acidity in the esophagus and preventing reflux. Flax seeds and oats are brewed as antacids. To maintain a normal pH level, drink the following infusion as tea:
- St. John's wort;
- chamomile;
- rosehip;
- calendula.
Compliance with diet and food processing rules is important. You should reduce your consumption of fried, fatty foods and avoid overeating. Stick to a strict diet during an exacerbation period.
For diseases of the esophagus, symptoms and treatment are specific. Most of them are curable; it is important to correctly identify the disease and select individual therapy.
Treatment
Photo: med-explorer.ru
Correct nutrition and an appropriate diet play an important role in treatment. It is necessary to observe fractional meals, that is, meals should be taken in small quantities 5 - 6 times a day. It is not recommended to eat food that is too hot or, conversely, too cold. Products that negatively affect the tone of the lower esophageal sphincter are excluded from the diet. Foods with high fat content, spices, black coffee, mushrooms, and white cabbage have this effect. In addition, it is necessary to exclude the use of foods that irritate the mucous membrane of the esophagus, for example, onions, garlic, tomatoes, sorrel, fried foods, and so on. Rye or any fresh bread, as well as flour products made from puff pastry or butter dough, are completely excluded. When consuming meat and poultry, preference should be given to low-fat varieties. Dairy products have a beneficial effect on the mucous membrane of the digestive tract, but do not forget that it is strongly recommended to avoid consuming dairy products with high acidity. It is important to remember that the last meal should be no later than 3 hours before expected sleep. If a person has problems with the cardiac sphincter, it is recommended not to take a horizontal position immediately after eating. To avoid the reflux of stomach contents into the cavity of the esophagus, after eating, it is necessary to remain in a sitting position for at least 30 minutes; only after this time is it possible to assume a horizontal position. For the same purpose, it is strongly recommended to refrain from using tight belts and belts, which contribute to an increase in intra-abdominal pressure. In addition, you should avoid intense physical activity, while not forgetting the importance of the presence of physical therapy in the life of every person. Also, do not forget about the importance of giving up bad habits, in particular smoking and drinking alcohol, which have an extremely aggressive effect on the mucous membrane of the esophagus.
Drug treatment consists of prescribing medications that can normalize acidity in the esophagus and stomach. In addition, to prevent the reflux of gastric contents into the esophageal cavity, drugs are prescribed that improve the motility of the digestive tract. To quickly eliminate a defect in the mucous membrane of the esophagus, agents that promote tissue healing can be used.
Indications for surgical intervention are:
- lack of the desired effect from the use of conservative treatment methods;
- the presence of a hiatal hernia;
- combination of an esophageal ulcer with insufficient closure of the lower esophageal sphincter (the so-called gastroesophageal reflex disease);
- the development of the following complications of the disease: perforation of the ulcer, that is, the formation of a hole in the wall of the esophagus;
- penetration - spread of an ulcer to nearby organs;
- bleeding from an ulcer;
- cicatricial narrowing of the ulcerative defect, which leads to a decrease in the lumen of the esophagus;
- malignancy (malignancy);
- rapid loss of body weight.
In these cases, fundoplication is most often used, which consists of suturing the stomach to the diaphragm around the esophageal opening and then fixing it to the abdominal wall. The manipulation is performed in such a way that an acute angle is maintained between the esophagus and the fundus of the stomach. In most cases, this operation is performed in combination with selective proximal vagotomy, which involves cutting the branches of the vagus nerve, resulting in a decrease in the production of hydrochloric acid.