Indications for use
Esophagoplasty surgery is prescribed in the following cases:
- Esophageal atresia - when there is a large diastasis. If a delayed anastomosis could not be performed or it was performed but unsuccessfully (occurrence of esophagostomy).
- For a caustic burn of the stomach, if bougienage did not give the desired result.
- Injury to the esophagus due to prolonged presence of a foreign object in it.
- Tumors of the esophagus.
- Motor dysfunction.
There are 4 types of surgery:
- colonic transplant;
- gastric tube;
- jejunal transplant;
- mobilization of the stomach into the sternum.
The last method is the most popular these days. This method has a number of advantages over others. The scheme and technique of surgical intervention are selected by the doctor based on the type and severity of the disease, as well as the individual characteristics of the patient.
Types
As mentioned earlier, surgical methods are divided into several types. In general, they can be divided into two groups - radical and palliative.
Radical
Completely eliminate the affected areas. There are several methods of radical surgery:
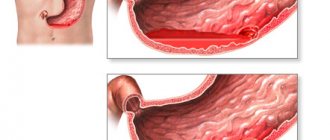
- Extirpation of the esophagus - complete removal. Extirpation of the esophagus is appropriate for cancer, large scar formations or Barrett's disease.
- Resection is the partial removal of the esophagus in case of cancer, which has affected only a separate part of the organ; it begins to gradually close; with a hiatal hernia and cicatricial narrowing, inflammation of the rosette of the mucous membrane of the cardia. There are two types of plastic - immediate or secondary.
- Lewis technology - partial excision with immediate replacement with a tube made from stomach tissue.
- Tunnel method of extirpation of the esophagus - the operation is performed through two incisions in the neck and in the epigastrium, a gaping passage is made under the skin that connects them.
Palliative
Necessary to maintain the functioning of the esophagus, necessary to improve the patient’s well-being. They are divided into several subspecies:
- Gastrostomy placement - if esophageal plastic surgery and resection are not possible, a gastric fistula is inserted into the patient, bypassing the esophagus itself, for nutrition.
- Stenting is the insertion of a special tube into the esophagus to keep the passage open.
- Sclerosis of the esophageal veins is important for liver cirrhosis. The Casino X welcome bonus will allow beginners and experienced players to hit the jackpot! Essentially, this is the use of substances that shrink veins - ethoxysclerol or medical acrylic glue. Substances are administered until complete sclerosis of the veins occurs.
- Ligation of varicose veins is a procedure similar to the previous method, but lasts a little longer.
Contraindications
Surgery on the esophagus cannot be performed in the following cases:
- the presence of acute infectious diseases or exacerbation of chronic pathologies;
- poor clotting;
- decompensated diabetes mellitus;
- diseases of the cardiovascular, respiratory system, liver, kidneys (especially with vascular and respiratory failure);
- postoperative period after abdominal surgery;
- pregnancy (if the pathological condition does not threaten the life of the expectant mother);
- in the case of a malignant neoplasm, contraindications include inoperability of the tumor;
- when the patient is over 60 years old;
- excess weight or, conversely, excessive exhaustion.
Patient preparation
Before the operation, the following diagnostic examinations are mandatory:
- general analysis of urine and blood;
- biochemical analysis;
- coagulogram;
- ECG;
- fluorogram;
- consultations with a therapist and a specialist in a chronic disease.
To select the method of operation and its volume in severe pathological conditions, it is necessary to do the following studies:
- radiography;
- FGDS;
- study of the acidity of the bolus of food in the esophagus and stomach throughout the day;
- manometry;
- endoscopic ultrasound;
- CT or MRI.
For the operation to be successful, before it is carried out, all existing chronic pathologies must be put into remission. Before surgery, it is prohibited to undergo treatment with blood thinning drugs and medications to reduce the tone of muscle fibers. You also need to stop smoking a month before the operation.
Prognosis for esophageal cancer
Is there any point in having surgery? If you don't remove the esophageal tumor, you have less than a 5% chance of surviving the five-year mark. In turn, if you receive adequate treatment even for locally advanced esophageal cancer, when there are metastases to regional lymph nodes, you can survive the five-year mark with a 20% probability.
The individual prognosis largely depends on the stage. For those patients whose cancer is completely confined to the lining of the esophagus, the five-year survival rate exceeds 80%. Involvement of the submucosal layer reduces it to 50%. The spread of the tumor to the muscular lining of the esophagus implies a 20% five-year survival rate, and its germination into structures adjacent to the esophagus - 10%. In patients with distant metastases, the five-year survival rate is within 5%.
Quite often, patients with esophageal cancer at an advanced stage come to foreign clinics in the hope of help. The minimally invasive surgical techniques used, which make it possible to carry out chemoradiation treatment for esophageal cancer, provide an increase in the survival rate of such patients.
While there is no surefire way to prevent esophageal cancer, Israeli oncologists recommend the following to reduce your risk:
- Quit smoking. This is one of the most significant risk factors for the development of esophageal cancer and other types of cancer.
- Stop drinking alcohol or try to reduce the amount of alcohol you drink.
- Contact your doctor if you experience persistent heartburn, which may be a symptom of gastroesophageal reflux disease (GERD).
- Exercise regularly and avoid gaining extra pounds.
By following simple recommendations and undergoing preventive examinations in the hospital, there is always a chance to prevent the disease or detect it at an early stage of development.
Stages of implementation
Progress of surgery:
- Laparotomy is performed. An elliptoid incision of an esophagostomy or a “low” transverse right-sided, left-sided one is made on the neck to isolate the cervical esophagus. In some cases, a thoracotomy may be necessary.
- The stomach is removed through the incision. The hole is sutured. The stomach is mobilized along the greater and lesser curvature. In this case, the arcades of the right gastroepiploic and gastric arteries are not affected.
- The movement continues proximally. In this case, the short vessels between the fundus of the stomach and the spleen, the left gastric artery and vein are ligated and crossed.
- For large diastasis, the stump of the distal esophagus is mobilized from the posterior mediastinum by dividing the diaphragmatic-esophageal membrane. The anterior and posterior trunks of the vagus nerve ending are crossed. The esophagus is cut off at the level of the esophagogastric junction and the defect in the stomach is sutured.
- Pyloroplasty is performed. Esophagogastroanastomosis is located at the “top” of the fundus of the stomach. 2 seams are made using different threads.
- The esophagus is mobilized from the cervical incision. The recurrent laryngeal nerve is not affected.
- The mediastinal tunnel is created from the prevertebral fascia. The discharge is made from above in the posterior mediastinum posterior to the trachea and downwards, from below in the prevertebral space behind the cardiac organ.
- Using suture holders as guides, the stomach is brought up through the esophageal hiatus and the tunnel in the posterior mediastinum until its bottom becomes visible.
- A single-row anastomosis between the cervical esophagus and the fundus of the stomach is performed with a thread using a special instrument. Before completing the suturing of the anterior lip of the anastomosis, a nasogastric tube is inserted into the stomach. Stitches are applied. A soft rubber drainage is installed on the neck
The operation is successful in most cases. The death rate is only 5%.
Diagnostics
The presence of basic symptoms cannot be an essential prerequisite for surgical intervention; the basis for surgical intervention is a specific diagnosis, based on which the doctor determines the need for radical measures.
To clarify the diagnosis, a thorough examination is performed, which includes the following diagnostic procedures:
- fluorography of the esophagus - determines the expansion of the lumen of the esophagus, restructuring of the relief of the mucous membrane, unevenness of the outline;
- esophagomanometry - determines displacement of the cardia into the posterior mediastinum (cardia insufficiency);
- endoscopy;
- biopsy;
- analysis for the presence of tumor markers;
- endoscopic optical coherence tomography.
Postoperative period
In the first week of rehabilitation, the patient is weakened. He cannot feed himself. He is fed through a special tube. For the first few weeks, the person operated on is under the supervision of medical personnel. This helps avoid complications.
If doctors note that the patient is recovering, soft and then hard food is added to his diet. Between meals, you need to do special breathing exercises to restore the tone of the cardiac sphincter. The patient is given a stimulus spirometer. This way you can track the load and increase it if necessary.
Possible complications
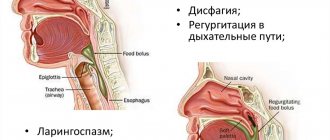
After surgery on the esophagus, you need to be prepared for the fact that surgery can lead to the following adverse consequences:
- blood clot formation;
- hemorrhage;
- penetration of infectious microorganisms;
- heart failure during surgery;
- allergies to anesthetic medications;
- disturbances in the respiratory process.
With open surgery on the esophagus, the risk of complications is slightly lower. However, the following may occur:
- damage to the pulmonary organ;
- infection in the chest cavity;
- mechanical damage to neighboring organs;
- closing the passage between the esophagus and the stomach.
The intestines may begin to reject food. This is due to the fact that after surgery gastric insufficiency occurs (loss of the ability to absorb fats and glucose). This pathological condition is called dumping syndrome. He is being treated by a nutritionist. As a rule, six months is enough for the body to adapt to a new way of life.
Selected species
In addition to the main types, there are several separate types of surgical methods.
Complete removal
It is performed under conditions of complete opening of the chest cavity. The postoperative prognosis is often unfavorable; such treatment is prescribed only for severe pathologies of the esophagus. In this case, the organ is replaced with an implant made from gastric tissue - immediately or during a second surgical intervention.
The latter minimally invasive technology causes less damage, is longer lasting, but has a more positive prognosis, making it the most desirable treatment alternative. It is performed by penetrating the tissue with medical instruments through a subcutaneous tunnel, which then easily closes and grows together. The esophagus is cut off through the upper and lower incisions and removed through the subcutaneous passage.
Resection
Resection of the esophagus is necessary in the presence of Barrett's disease, cardiospasm, or if the child was born with an enlarged esophagus. The procedure involves partial removal of an organ from a child or adult followed by its immediate replacement - Lewis surgery.
Laparoscopic interventions
Prescribed for diseases of the lower esophagus and upper esophageal opening of the diaphragm, dysfunction of the rosette of the mucous membrane of the cardia. Among them are sewing in the hernia openings, strengthening them, reducing the volume of the stomach by sewing in (bypass surgery), and plastic surgery of the organ, in particular the lower cardiac region.
Endoscopic manipulations
In this way, benign tumors on the mucous membrane, polyps, are removed by ligating varicose veins, sclerotherapy, laser irradiation, cauterization or exposure to low temperatures on the affected areas.
The main instrument, the endoscopic probe, consists of a mini-video camera, a set of magnifying lenses and lighting devices. The lumen of the esophagoscope allows you to insert the necessary instruments into the hole.