Description of the organ
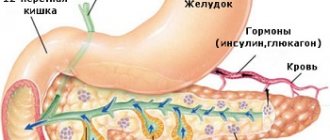
Let's look at the structure and functions of the pancreas. It is located in the retroperitoneal space between the duodenum and the upper lumbar vertebrae, above the kidneys, and looks like an elongated “comma”. The weight of an adult human organ ranges from 80-90 g.
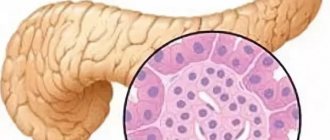
The structure of the pancreas is a combination of glandular lobules through which blood vessels pass and excretory ducts. The lobules produce pancreatic juice, the enzymes of which (lactase, amylase, trypsin, invertase, lipase) affect the processes of breakdown of food. Throughout the gland there is a channel through which the juice penetrates the duodenum, where it mixes with bile and ensures the process of intestinal digestion. Complexes of cells between the lobules with a developed capillary network are called islets of Langerhans. These formations of alpha, beta and delta cells synthesize hormones (insulin and glucagon).
Functions of the organ
The pancreas, as already mentioned, produces pancreatic juice. In the duodenum, food is broken down to the state necessary for absorption. This occurs under the action of hydrolytic digestive enzymes of the pancreas, which are responsible for the interaction of food substances with water.
Pancreatic juice consists of hydrolases that perform separate functions. They are divided into four categories:
- Lipase is an enzyme that breaks down fats into complex elements: glycerol and higher fatty acids. It also ensures the absorption of vitamins A, E, D, K.
- Proteases (chymotrypsin, carboxypeptidase, trypsin), activating enzymes that break down proteins into amino acids.
- Carbohydrases (amylase, maltase, lactase, invertase), necessary for the breakdown of carbohydrates into glucose.
- Nucleases are enzymes that break apart nucleic acids and form their own genetic structures.
The principle of functioning of the pancreas is very complex. Enzymes begin to be produced in the required quantities 2-3 minutes after food enters the stomach. It all depends on the concentration of fats, proteins and carbohydrates present in it. In the presence of bile, the production of pancreatic juice with enzymes can last up to 12 hours.
Types of deficiency and signs
There are 4 types of pancreatic pathologies.
- Insufficiency of external secretion of pancreatic enzymes.
- Exocrine pancreatic insufficiency.
- Enzyme deficiency in gastric juice.
- Decreased production of the hormones glucose, lipocaine and glucagon with endocrine deficiency of the organ.
Due to external secretory insufficiency of the pancreas, there is a decrease in the activity of special secretion elements that break down eaten foods into substances that are easily absorbed by the body, or the secretory waste of digestive juice into the intestines changes due to narrowing of the ducts due to existing tumors and fibrosis. When enzyme activity is disrupted, the secretion becomes thick and viscous, and food is poorly broken down. If there is a narrowing of the passages into the intestines, an incomplete volume of enzyme elements arrives, which do not cope with their task as needed.
The main features include:
- inability to tolerate fatty and spicy foods;
- feeling of heaviness in the stomach area;
- stool disorder;
- colic in the abdominal area, bloating.
colic in the stomach
Due to a decrease in protein fermentation content, this leads to the formation of:
- shortness of breath;
- anemia;
- weaknesses in the body;
- fatigue;
- tachycardia.
Exocrine pancreatic enzyme deficiency is manifested by a decrease in the productivity of pancreatic juice, which is responsible for the natural working process of the gastrointestinal tract.
The disease is formed by the following symptoms:
- indigestion;
- nausea;
- heaviness in the stomach area;
- excess gases in the intestines;
- intestinal dysfunction.
Exocrine pancreatic deficiency occurs:
- relative - characterized by an irreversible course, the integrity of the pancreas does not change, malaise is often a consequence of immaturity of the pancreas or impaired secretion. Often observed in childhood;
- absolute disorder - accompanied by necrosis of the acini, fibrosis of organ tissue, and decreased production of pancreatic enzymes. Develops as a result of chronic and acute pancreatitis, cystic fibrosis, Shwachman-Diamond syndrome.
Inferiority of organ enzymes is manifested by indigestion.
- Flatulence.
- Nausea.
- Vomit.
- Feces have an unpleasant odor.
- Loss of fluid in the body.
- Weakness.
flatulence
The most significant symptom of enzyme deficiency is a change in stool. The patient's frequency of bowel movements increases, the feces have excess fats that are difficult to wash off, the stool has a gray tint and a putrid odor.
In the case of endocrine disruption, this type is dangerous because it leads to the development of organ dysfunction in the body and irreversible consequences. When insulin production changes, diabetes mellitus develops. The main symptoms that indicate a lack of insulin hormones include:
- increased blood glucose after eating;
- feeling of thirst;
- frequent urination;
- itching in the genital area in women.
When the production of glucagon decreases, the patient complains of weakness, dizziness, cramps in the limbs, impaired mental state, and loss of reason.
Exocrine pancreatic insufficiency
It is one of the most common consequences of organ inflammation, especially if such a pathology is characterized by a chronic course.
A distinctive sign of exocrine pancreatic insufficiency is a decrease in the absorption of nutritional components (malabsorption) against the background of the development of maldigestion - a violation of the breakdown of food into components acceptable for the digestive process. This pathology is also called enzyme deficiency. Despite the prevalence of such pathologies among all groups of people, insufficiency of enzyme production is considered a serious condition that can lead to depletion and even death of the patient if left untreated.
Diagnosis of pathological changes in the pancreas
First of all, the attending physician conducts a survey of the patient and finds out the symptoms that distinguish pancreatic enzyme deficiency. To diagnose the disease, laboratory blood tests are performed (for the content of hemoglobin and biochemical substances, for sugar levels), studies of the presence of enzymes in the urine, stool analysis and coprogram for fat content (normally no more than 7%), elastase-1 and the state of absorption and processing food by the body.
To identify degenerative changes in organs, abdominal ultrasound, CT and MRI are prescribed. An important diagnostic method is endoscopic retrograde cholangiopancreatography (examination of the pancreatic ducts and bile ducts for their patency and the presence of keloid formations). To clarify the diagnosis, a method of direct study of secretions obtained from the pancreas by aspiration of the pancreas is used, which allows one to determine the content and volume of pancreatic juice.
Important information: How to make your pancreas work better
Endocrine insufficiency is tested by glucose tolerance testing—blood collected on an empty stomach and blood collected 2 hours after a meal or 75 g of glucose. This test shows the body's ability to produce insulin and process glucose.
The following indicators indicate a disturbance in glucose metabolism: blood glucose level of at least 6.7 mmol/l; 2 hours after taking 75 g of glucose - 7.8-11.1 mmol/l. Normally, the blood glucose level should not exceed 6.4 mmol/l. If the blood glucose level taken on an empty stomach is 7.8 mmol/L or more than this value, then diabetes occurs.
Varieties
Exocrine pancreatic insufficiency can be congenital (a genetic defect that disrupts or blocks the secretion of enzymes) and acquired type. In addition, pathology can be primary or secondary, absolute or relative.
Primary exocrine insufficiency is caused by damage to the gland and a decrease in its exocrine function. In the secondary type of disease, enzymes are produced in sufficient quantities, but their activation does not occur in the small intestine.
Reasons for the development of pathology
The main causes of the development of exocrine pancreatic insufficiency of the primary type include all forms of chronic pancreatitis, cystic fibrosis, pancreatic cancer, pancreas degeneration due to obesity, surgical interventions on the gland, Shwachman syndrome, congenital enzyme deficiency, agenesis or hypoplasia of the organ, as well as Johanson-Blizzard syndrome.
Pathogenetic causes of the formation of exocrine gland insufficiency include:
- fibrosis and atrophy of the organ (as a result of alcoholic, obstructive, non-calculous or calculous pancreatitis, atherosclerosis, malnutrition, age-related changes, hemosiderosis, diabetes mellitus);
- pancreatic cirrhosis (considered the outcome of some forms of pancreatitis: fibrous-calculous, alcoholic, syphilitic);
- pancreatic necrosis (death of gland cells);
- formation of stones in the pancreatic ducts.
Secondary exocrine insufficiency develops with lesions of the mucous membrane of the small intestine, after operations on the stomach and intestines, with gastrinoma, decreased secretion of enterokinase, pathologies of the hepatobiliary system, protein-energy deficiency.
Absolute enzyme deficiency of the gland is caused by suppression of the secretion of bicarbonates and enzymes against the background of a decrease in the volume of the organ. Relative insufficiency is caused by a reduced flow of pancreatic juice into the intestine due to obstruction of the lumens of the gland ducts by a tumor, stone, or scars.
Scars on the pancreas occur as a result of the death of parenchyma cells of the organ. Dense scar tissue forms in these areas. A similar process in medicine is called fibrosis, and it also leads to the development of exocrine insufficiency.
Types of enzyme deficiency in the body
Doctors divide this problem into 4 main types. Each of them has its own characteristics and symptoms; treatment is also based on the type of pancreatic insufficiency. Types of pancreatic enzyme deficiency:
- Exocrine.
- Exocrine.
- Enzymatic.
- Endocrine.
Each type requires detailed consideration, since symptoms and therapy may differ significantly. Of course, the question of treatment is decided only by the attending physician, but you also need to know the general concepts that show the patient the picture of the disease.
We invite you to read: Treatment of diabetes mellitus in children in Israel
In medicine, pancreatic enzyme deficiency is usually divided into 4 main groups. Each of them has its own characteristics and clinical picture.
These include:
- exocrine form;
- exocrine form;
- enzyme form;
- endocrine form.
Before starting treatment, it is necessary to understand the patient’s complaints and compare them with symptoms.
Exocrine pancreatic insufficiency was previously diagnosed in people over 50 years of age. But nowadays, this form of the disease can also be found in patients aged 20-30 years. This develops against the background of the fact that the number of cellular structures for secretion production has greatly decreased.
The causes of the pathological phenomenon lie in the following:
- decrease in the mass of pancreatic parenchyma due to endocrine diseases;
- disruption of the outflow of contents into the lumen of the small intestine;
- sluggish nutrient processing.
Symptoms of pancreatic insufficiency are accompanied by:
- soreness in the abdomen;
- rejection of fatty and salty foods;
- feeling of heaviness in the gastric cavity;
- diarrhea;
- bloating;
- the appearance of colic and aching, painful feeling in bone tissue;
- increased heart rate;
- development of convulsive syndrome;
- shortness of breath;
- blood clotting disorder;
- dryness and itching of the skin;
- nausea and vomiting.
Such symptoms signal a fat deficiency.
To restore external secretory function, it is necessary to begin treatment as soon as possible. It is based on compliance with certain recommendations.
- Eat properly. Portions should be small, and you should eat as often as possible.
- Fatty and fried foods are excluded from the menu.
- The last meal is at 6-7 pm. Night snacks are completely excluded.
- Alcohol-containing drinks are prohibited.
- The list of permitted products is prescribed only by a doctor based on individual indications.
An important point in case of exocrine insufficiency is that food of animal origin must be replaced with plant food. It should make up 70-80% of the entire menu.
Since the body cannot produce the required amount of enzymes and does not receive fats, carbohydrates will quickly leave it. Products rich in their content include confectionery and flour products. But they are banned. Therefore, it is recommended to replace them with vegetables and fruits. But such a menu also adversely affects the functioning of the body - it reacts with increased formation of gases. But bran helps reduce it.
Enzyme deficiency of the pancreas is compensated by taking medications:
- Mezim,
- Creon,
- Pancreatin,
- Festal.
The first sign of proper treatment is the normalization of stool and the disappearance of other unpleasant symptoms.
Exocrine pancreatic insufficiency is characterized by a violation of the production of digestive juice for the complete processing of the food bolus.
Doctors identify several main reasons for this phenomenon:
- malfunction of the pancreas;
- diseases of the gastric cavity;
- gallbladder diseases;
- problematic condition of the duodenum;
- unbalanced diet;
- chronic alcoholism;
- long fasting.
We suggest you read: Low lower pressure: causes and treatment, what low lower pressure means
Symptoms of pancreatic enzyme deficiency are characterized by:
- poor digestion of food;
- increased formation of gases;
- difficulties with bowel movements;
- nausea and vomiting;
- heaviness in the stomach.
The exocrine type of disorder can only be confirmed using laboratory diagnostics. A mandatory test for this pathology is checking blood sugar, since there is a high probability of diabetes mellitus.
Treatment is based on eliminating the root cause. If alcohol or diet has disrupted the production of pancreatic juice, the patient should reconsider his life principles. Mono-diets and prolonged fasting lead to a lack of important elements: proteins, fats and carbohydrates. This process adversely affects not only the pancreas, but also the entire body as a whole.
The diet should be rich in vitamins in the form of ascorbic acid, alpha-tocopherol, retinol. They have a positive effect on the digestive organs. In some cases, the doctor prescribes enzymes.
Enzyme deficiency is accompanied by constant pain. In this case, there is a serious enzyme deficiency.
The causes of the pathological process are:
- excessive use of medications;
- infectious diseases;
- injury to the pancreatic duct;
- the presence of congenital pathologies in the pancreas;
- intestinal dysbiosis.
Often, enzyme deficiency manifests itself as acute or chronic pancreatitis. The clinical picture of these diseases is the same and is accompanied by:
- irregular bowel movements. Patients often complain of diarrhea. Feces have a fetid odor;
- lack or worsening of appetite;
- general weakness;
- bloating due to a large amount of gas;
- weight loss;
- painful sensations in the abdomen.
The pancreas is responsible not only for the functioning of the digestive tract, but also helps the endocrine system. Inside this organ, insulin, glucagon and lipocaine are produced. Such components are responsible for blood sugar levels.
- Insulin lowers glucose levels.
- Glucagon is necessary to increase blood sugar.
- Lipocaine. Inhibits the occurrence of fatty infiltration in the liver and stimulates the effect of lipotropic substances.
If the production process is disrupted, adverse consequences may develop. The problem primarily concerns the islets of Langerhans, as they are responsible for the production of hormones.
A disorder of the endocrine function of the pancreas is characterized by some symptoms such as:
- release of gases and unpleasant odor;
- nausea and vomiting;
- foul-smelling, loose stools;
- increasing the number of bowel movements per day;
- bloating;
- abnormalities in blood counts. They can be lower or higher depending on the work of a particular hormone;
- weaknesses;
- dehydration of the body.
Treatment is based on following certain recommendations.
- Adhering to a strict diet. Fatty and fried, spicy and salty foods are excluded from the diet. Various sweets, sugar, coffee, smoked foods, and marinades are prohibited.
- Constantly monitoring blood sugar. The patient needs to purchase a special device that will help measure sugar levels. It's called a glucometer. Manipulations must be carried out in the morning on an empty stomach and after meals.
- Taking pills to normalize blood sugar.
We invite you to read: Atherosclerotic cardiosclerosis - causes, symptoms, treatment
If it is not possible to normalize the functioning of the pancreas, it means that diabetes mellitus will occur. This is one of the serious and dangerous diseases. But you can learn to live with it. In severe cases, the patient is prescribed insulin injections, otherwise everything will end in death.
Symptoms
Let's figure out where a person's pancreas hurts. The greatest significance in the clinical picture of this pathology is maldigestion syndrome, which is characterized by inhibition of digestive processes in the intestines. Undigested fats in the colon stimulate the production of colonocytes - diarrhea and polyfecal matter develop, stool acquires a foul odor, gray color, its surface is shiny and oily. There may also be undigested food particles in the stool.
Maldigestion of proteins contributes to the appearance of protein-energy deficiency, which is manifested by dehydration, progressive weight loss, deficiency of microelements and vitamins, and anemia. Weight loss is greatly influenced by adherence to a diet low in carbohydrates and fats, as well as the fear of eating, which develops in many patients with chronic pancreatitis.
The symptoms of exocrine pancreatic insufficiency are quite unpleasant. Impaired gastric motility (dyspeptic disorders, feeling of fullness) can be caused by both exacerbation of pancreatitis and the influence of exocrine insufficiency of the gland due to changes in gastrointestinal regulation and the occurrence of duodenogastric reflux.
Chronic pancreatitis. Treatment
The basis for successful treatment of chronic pancreatitis is:
- complete exclusion of the causative factor of the disease,
- treatment of concomitant diseases of the digestive system,
- individual construction of conservative treatment.
- All patients should avoid alcoholic beverages and smoking!
Basic principles
- relief of pain, prevention of the development of complications of the disease (surgical) and creation of functional rest for the pancreas, reduction and removal of intoxication,
- correction of enzymatic insufficiency of the pancreas, disorders of digestion and absorption of food (fats, proteins, vitamins and minerals),
- correction of the intrasecretory function of the pancreas (pancreatogenic diabetes mellitus).
Relief and relief of pain with antispasmodics
Relief of pancreatic pain is a difficult task of conservative therapy. Approaches to the combination of various drugs are decided individually, based on the characteristics of the course and nature of pancreatic disorders in each patient.
It is important for patients to stop drinking alcohol!
To relieve pancreatic pain, medications of various pharmacological groups are used:
- analgesics (eg paracetamol) or non-steroidal anti-inflammatory drugs,
- antispasmodics (No-spa, Duspatalin, etc.), which normalize the outflow of bile and pancreatic juice (which reduces the pressure inside the pancreas),
- antisecretory drugs that reduce the acidity of gastric juice and thereby reduce the stimulated secretion of pancreatic juice (for example, Omez, Nexium, Kvamatel, etc.),
- in order to increase pain relief, treatment includes antidepressants and tranquilizers, which themselves have an analgesic effect and also enhance the effect of analgesics,
- pancreatic enzyme preparations (pancreatin groups), which cause a decrease in pancreatic secretion, reduce pressure inside the pancreatic ducts and reduce pain (Pancreatin, Mezim-forte, Creon, etc.)
If pain relief in chronic pancreatitis is ineffective, narcotic analgesics can be used or serve as an indication for surgical treatment.
Pancreatitis as a cause of pathology
Chronic pancreatitis is the main factor leading to enzyme deficiency. This is a lesion of the pancreas of inflammatory-destructive origin, leading to disruption of its functions. Few people know what the consequences of pancreatitis are. With an exacerbation of the disease, pain occurs in the abdomen and left hypochondrium, dyspepsia, yellowness of the sclera and skin are observed.
The main causes of the development of pancreatitis in adults (ICD-10 code K86) are cholelithiasis and alcohol abuse, which is quite toxic to the parenchyma of this organ. In case of cholelithiasis, the inflammatory process becomes a consequence of the transfer of infection from the bile ducts to the gland through the lymphatic vessels, the development of hypertension of the biliary tract, or the reflux of bile into the gland.
Conservative treatment of this disease includes a set of measures. The therapy is based on the following principles:
- diet is required;
- pancreatic insufficiency is subject to correction;
- pain syndrome must be eliminated;
- complications must be prevented.
When treating pancreatitis, it is necessary to avoid drinking alcohol, taking medications that can have a damaging effect on the pancreas (antibiotics, antidepressants, sulfonamides, diuretics: hypothiazide and furosemide, indirect anticoagulants, indomethacin, brufen, paracetamol, glucocorticoids, estrogens and many others).
The consequences of pancreatitis can be different: exocrine gland insufficiency, obstructive jaundice, portal hypertension, infections (parapancreatitis, abscess, retroperitoneal cellulitis, inflammation of the biliary tract), internal bleeding. With the development of this disease, diabetes mellitus, weight loss, and pancreatic cancer may also occur.
Chronic pancreatitis. Clinical manifestations
Chronic pancreatitis in a quarter of patients is asymptomatic, especially in the initial period.
Stomach ache
Subsequently, in 80-90%, the main characteristic symptom is abdominal pain syndrome (abdominal pain).
The pain is of the nature of recurrent (repeating) attacks - “pancreatic colic” and often becomes permanently debilitating.
The localization of pain depends on the damage to different parts of the pancreas, so when the head is affected - pain in the right hypochondrium, the body - pain in the epigastric region, when the tail of the pancreas is damaged - pain in the left hypochondrium. When the entire gland is affected, “girdling” pain is observed, which occurs in 30-35% of patients.
Often there is irradiation of pain to the left shoulder blade, to the left half of the chest, to the heart area.
Pain usually occurs 30-40 minutes after eating a large, fatty meal, drinking alcohol, cold fizzy drinks, spicy seasonings, large amounts of raw vegetables, citrus fruits.
Pain can last from 30 minutes to 3 or more hours.
Pain can be provoked by psycho-emotional stress, heavy physical work, and hypothermia.
Hunger pains that occur 4-6 hours after eating are often observed.
In case of pain, patients take a forced position, they cannot lie on their backs, relief is found only in the knee-elbow position or on the stomach, patients switch to fasting and drinking alkaline waters.
The first years in the initial stage of the disease are intense. frequent, requiring intensive therapy, after 5-10 years the pain is aching, dull, without clear localization and irradiation. This is a sign of disease progression with the development of pancreatic enzymatic insufficiency. During the period of development of complications, after 7-15 years (but can happen at any stage of the disease), pain becomes rare and not pronounced and in clinical manifestations, manifestations of enzymatic deficiency (exocrine pancreatic insufficiency) and disturbances of intrasecretory function - carbohydrate disorders metabolism, may be diabetes.
Dyspeptic disorders
Dyspeptic disorders (dysmotor gastroduodenal dyspepsia syndrome) are observed 3-5 years from the onset of the disease and include:
- dry mouth, nausea,
- vomiting, often at the height of pain, repeated, not bringing relief to the patient,
- heartburn, belching,
- flatulence, feeling of fullness in the stomach.
Exocrine insufficiency syndrome
The pancreas produces few digestive enzymes, the processes of food digestion and absorption of food components are disrupted, and as a result of this the following appear:
- diarrhea, which may alternate with constipation,
- increase in stool volume up to 500 g or more,
- stool up to 2-6 times a day, often after meals, the stool is gray, oily, difficult to wash away, foul-smelling, unformed (steatorrhea is observed in 5-15% of cases),
- dryness and flaking of the skin,
- stomatitis, glossitis (inflammation of the tongue, swelling with teeth marks),
- bone pain,
- decreased or complete loss of appetite (anorexia),
- weakness.
Intrasecretory pancreatic insufficiency syndrome
They manifest themselves in the form of diabetes mellitus (thirst, dry mouth, increased urination) in 3-10% of patients with chronic pancreatitis.
Signs of pancreatogenic diabetes usually appear late - 15 or more years from the onset of chronic pancreatitis. Sometimes this may be the only manifestation of painless pancreatitis.
Syndrome of vegetative and mental disorders
- emotional lability,
- irritability,
- sleep disorders,
- depressive state.
Diagnostics
The main role in identifying enzyme deficiency in pancreatitis in adults (ICD-10 code K86) is played by special tests (probeless and probe), which are often combined with x-ray, ultrasound and endoscopic methods. Tube diagnostics are considered more expensive and may cause discomfort to patients, but its results are more accurate. Tubeless procedures are cheaper, they are easily tolerated, but they make it possible to determine this pathological process in the body only in the complete absence or significant decrease in pancreatic enzymes.
The direct secretin-cholecystokinin probe test is considered the gold standard for diagnosing exocrine pancreatic insufficiency. This technique is based on stimulation of gland secretion by introducing cholecystokinin and secretin, with further sampling of duodenal contents with a time interval of 10 minutes. The samples examine the rate and activity of pancreatic secretion, the level of zinc, bicarbonates, and lactoferrin.
Indirect Lund probe testing is similar to the previous method, however, gland secretion is stimulated by introducing food into the probe.
Tubeless techniques are based on the introduction into the body of certain substances that can interact with pancreatic enzymes in the blood and urine. The study of the metabolic products of such interaction provides an opportunity to evaluate the exocrine functions of the gland. Probeless tests include: pancreato-lauryl, bentiramide, triolein, iodolipol and others.
The level of pancreatic activity can also be determined in some indirect ways: by the level of absorption of plasma amino acids by the pancreas, through qualitative analysis of the coprogram, determination of the volume of fat, trypsin and fecal chymotrypsin, and elastase-1 in the feces.
Instrumental methods for diagnosing the disease are: x-ray of the peritoneum, CT, MRI, ultrasound of the pancreas, ERCP.
Treatment of pathology
Treatment of exocrine pancreatic insufficiency is usually complex. It includes correction of nutritional status, replacement and etiotropic therapy, as well as symptomatic treatment. Etiotropic therapy is aimed at preventing the progression of gland cell death. Lifestyle correction involves eliminating alcohol consumption and smoking. It is also planned to increase the amount of protein in the diet, reduce the amount of fat, and take vitamins.
The main method of treatment for chronic pancreatitis is enzyme replacement (lifelong). The indication for enzyme replacement therapy is steatorrhea with a loss of more than 15 g of fat per day, and progressive protein-energy deficiency.
The most effective are microgranulated enzyme products in acid-resistant shells and in gelatin capsules, which dissolve in the stomach, providing conditions for uniform mixing of medication granules with food. The dosages of such drugs are selected individually and depend on the severity of the disease and the activity of pancreatic secretion.