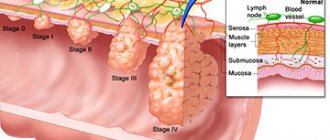
Types and stages of the disease
In clinical practice, the following stages of diverticular disease are usually distinguished:
- Diverticulosis is asymptomatic. In half of the cases, the pathology does not have pronounced clinical manifestations for a long period and is discovered accidentally, after contacting a specialist for another reason.
- Diverticulosis is acute. Characteristic signs are spasms of the walls of the sigmoid colon, a high content of pathogenic microflora in the affected area and nearby parts of the intestine, and disturbances in digestive activity.
- Complicated diverticulosis. The extreme stage of the disease, which is characterized by critical states of the patient’s well-being. Requires immediate medical intervention.
Complicated diverticulosis, in turn, is divided into the following categories:
- Diverticulitis of the sigmoid colon. It develops as diverticula are filled with feces, which creates favorable soil for the proliferation of pathogenic bacteria, as a result of which the threat of infection increases;
- Peri-intestinal infiltrate. Occurs when the abdominal cavity is subject to extensive inflammation, and the surface of the diverticulum itself is significantly damaged;
- Intestinal fistula. It is characterized by spontaneous opening of the abscess, affecting neighboring tissues and organs, which entails the formation of external and internal fistulas. This form requires urgent surgical intervention;
- Intraintestinal hemorrhage. Occurs due to damage to the intestinal mucosa through exposure to hardened feces. Vessels are damaged, and significant volumes of blood are lost both during and independently of defecation;
- Diverticulum perforation. If perforation affects the peritoneal area, this threatens the occurrence of peritonitis; if the mesentery of the sigmoid colon is affected, the patient runs the risk of getting retroperitoneal phlegmon.
Diverticulosis and its types
To adequately assess the patient’s condition, proctologists have developed a classification of diverticular disease of the sigmoid colon. It has 3 main forms:
- Diverticulosis without pronounced symptoms.
- Diverticular disease with clinical signs.
- Advanced stage, accompanied by complications.
Asymptomatic course of the disease
Most cases of sigmoid colon diverticulosis are diagnosed incidentally when patients are being examined for other pathologies. A person sometimes feels a slight pain that radiates in the abdomen, specifically in the lower left part. The patient attributes this to poor quality food, because everything goes away after a bowel movement or with the release of gases. The doctor recommends following a diet for this form of diverticulosis, and in case of constipation, prescribes laxatives.
- Cucumber salad for the winter without sterilization
- Champignon soup: recipes with photos
- Ultrasound of the mammary glands
With clinical manifestations
A gradual worsening of the symptoms of such a pathology of the sigmoid colon if the doctor’s recommendations are not followed leads to more serious consequences. This is how diverticulitis develops, which can lead to complications of the disease. The severity of symptoms depends on the number of diverticula in the intestine, concomitant ailments and the age of the patient. The pain becomes more acute, becomes stronger after meals and spreads to the buttocks and even the lower back. This form of sigmoid colon diverticulitis requires medical or even surgical treatment.
Causes of diverticulosis of the sigmoid colon
Diverticulosis develops due to a combination of factors that occur in older people. Over time, certain areas of the walls of the sigmoid colon begin to weaken, as a result of which, first, minor protrusions are formed, and then full-fledged diverticula. The main reason for the appearance of areas of intestinal weakening is a violation of innervation.
The aging process predisposes to the appearance of diverticula. As we age, dystrophic changes are observed in the tissues of all organs, including the intestinal muscles. Among other things, older people experience a decrease in the level of nutrients in the body, which predisposes to the appearance of protrusions in the intestines.
Another common cause of diverticula is weakness and underdevelopment of connective tissue. It should be noted that such developmental disorders, as a rule, do not lead to the appearance of diverticula at a young age, but almost always provoke protrusion of sections of the sigmoid colon in the elderly. Underdevelopment and weakness of connective tissue is a congenital defect characterized by a failure in the synthesis of collagen fibers.
In addition, an increased risk of diverticula occurs in older people with signs of incoordination of intestinal motility. The fact is that chronically increased intraintestinal pressure causes stretching of the muscle fibers of the walls of the sigmoid colon and, over time, leads to the appearance of a full-fledged diverticulum.
In some cases, severe spasms of the intestinal walls can provoke the appearance of a sigmoid colon diverticulum. During a spasm, intrawall blood vessels are compressed, which leads to disruption of blood microcirculation. Impaired tissue nutrition irreversibly leads to the appearance of areas of muscle tissue degeneration and stretching of the perivascular spaces.
Improper nutrition also contributes to the development of diverticulosis of the sigmoid colon. Diverticular disease of the colon almost never occurs in people who prefer plant-based foods rich in fiber. At the same time, among people living in developed countries and who prefer to eat soft foods rich in animal fats, the incidence rate is extremely high.
Hereditary predisposition also plays a role in the process of damage to the sigmoid colon by diverticula. Currently, there are no known genes that can be transmitted and lead to weakening of the muscles of the intestinal walls, but, according to statistics, people who have relatives suffering from diverticulosis in old age often experience the appearance of a similar disease.
Diagnostic methods
On x-ray, diverticula are visible as sac-like protrusions connected to the intestinal lumen
When performing a colonoscopy, you can detect the mouths of diverticula opening into the intestinal lumen
Computed tomography allows us to see not only diverticula, but also inflammatory changes in the intestinal wall and surrounding tissues, abscesses, etc. (The arrow points to the sigmoid colon diverticulum)
The clinical picture of diverticulosis is nonspecific. In addition, the symptoms of the disease are similar to those of other colon pathologies: Crohn's disease, colorectal cancer, irritable bowel syndrome. Therefore, to find out the true cause of the patient’s suffering, they resort to instrumental diagnostic methods:
- Irrigography (irrigoscopy) – taking an x-ray after contrast injection into the large intestine. Diverticula are visualized as pouch-like protrusions associated with the intestinal lumen. They are especially noticeable with double contrast, i.e., the introduction of not only a contrast agent, but also air into the intestine. You can detect the flow of contrast into neighboring organs in the presence of fistulas or the abdominal cavity in case of perforation.
- Colonoscopy can detect the openings of diverticula. However, this method is less accurate than irrigography and requires experience from the doctor performing the examination. The entrance holes of diverticula are clearly visible at the stage of insertion of the device, when the intestinal loops have not yet been straightened. There is swelling and redness of the mucous membrane around the mouth.
- Ultrasound. This study allows you to detect diverticula, inflammatory thickening of the intestinal wall and adjacent structures. The method requires high professionalism from the diagnostician. The accuracy of the result is significantly influenced by the severity of flatulence. Large amounts of gas in the intestines make it difficult to visualize the internal organs.
- Computed tomography (CT) with contrast is a highly informative method that allows one to judge the number, location, size of diverticula, the condition of the intestinal wall and surrounding structures. During the examination, you can see inflammation, abscesses, including intramural ones, and narrowing of the intestinal lumen.
- Virtual colonoscopy is a non-invasive procedure to obtain a 3D image of the large intestine based on CT data. It is a good alternative to conventional colonoscopy. Allows you to assess the condition of the intestinal walls and identify pathological formations in its lumen.
Attention! Irrigography and colonoscopy are not performed for diverticulitis, as they can cause complications such as perforation or bleeding. In this case, CT becomes the method of choice; if it is not possible, ultrasound becomes the method of choice.
Symptoms of diverticulosis of the sigmoid colon
In most patients, diverticula of the sigmoid colon do not manifest themselves in any way. A person may not know about his problem for years until a complication arises, or he turns to a proctologist in connection with another pathology. A fifth of patients complain of periodic abdominal pain of the colic type. The pain is blurred or localized in the left iliac region; upon palpation, the abdominal wall is not tense. The pain syndrome can go away on its own, sometimes relief occurs after bowel movement. In addition, there is bloating, constant constipation, which is periodically replaced by diarrhea. All these symptoms fit into the clinical picture of irritable bowel syndrome, which makes diagnosis much more difficult.
Symptoms change and become more pronounced when complications occur. The most common of these is diverticulitis, or inflammation of the diverticula of the sigmoid colon. It occurs due to stagnation of feces in the intestinal lumen and in the diverticulum itself, the action of intestinal flora and increased permeability of the weakened walls of the sigmoid colon. Abdominal pain intensifies, its localization is often unclear. On palpation, there is some tension in the anterior abdominal wall and increased pain in the left iliac region. The patient's temperature rises and symptoms of intoxication appear.
The further course of the disease can lead to the formation of an infiltrate. Inflammation spreads to the mesentery, omentum and surrounding tissues. On palpation, a painful lump with limited mobility is felt in the left lower abdomen. An abscess may form at the site of the infiltration. The patient's condition deteriorates sharply, the temperature rises to high levels, the fever is hectic in nature with large daily fluctuations. On palpation, strong local tension in the abdominal wall and sharp pain are noted.
Perforation or perforation of diverticula of the sigmoid colon is the most severe complication. The process can develop against the background of diverculitis or without its signs. Patients complain of severe pain, weakness, and fever. The consequence of perforation is always peritonitis or retroperitoneal phlegmon (if perforation of the sigmoid colon diverticulum occurs in its mesentery). The patient's condition is severe, weakness, fever are noted, and symptoms of an acute abdomen are observed. If a perforation hole opens into a hollow organ or onto the surface of the skin of the abdomen, a fistula is formed. Most often, fistulas open into the lumen of the small intestine, bladder, and less often into the lumen of the vagina.
Violation of the integrity of the vessels of the intestinal wall leads to open bleeding. It may be the first and only symptom of sigmoid colon diverticula. Blood appears in the stool; it hardly mixes with the feces and does not change its color. Bleeding is rarely profuse, but can be repeated, since lumps of feces constantly injure the intestinal wall. Frequent bleeding ultimately leads to anemia.
Symptoms of a complicated disease
Diverticulitis is inflammation of the wall of a diverticulum. The provoking factor is impaired bowel movement and retention of intestinal contents. This contributes to traumatization of the mucous membrane, the introduction of infectious agents and the development of inflammation.
The main symptom of diverticulitis is pain. In contrast to the usual exacerbation of diverticular disease, muscle tension is often noted when palpating the abdomen. The patient’s body temperature also rises and inflammatory changes appear in the general blood test: acceleration of ESR, increase in the number of leukocytes and the predominance of band forms among them.
The transition of inflammation from the diverticulum to surrounding tissue is called peridiverticulitis. Clinically, this complication differs little from that described above. However, it should be remembered: the spread of inflammation increases the likelihood of perforation.
Perforation is the formation of a defect in the wall of the diverticulum with the release of intestinal flora into the abdominal cavity. This complication has several outcomes: intestinal abscesses, fistulas, peritonitis.
An abscess is a localized area of inflammation in the abdominal cavity. Clinically, it manifests itself as intense abdominal pain. The localization of pain depends on the location of the abscess. In this case, there are signs of impaired intestinal motility: flatulence, constipation. The patient has an elevated body temperature, and the above-described signs of inflammation are detected in the blood. The abdomen is tense in the area where the abscess is located.
Opening an abscess can result in the formation of a fistula or the development of peritonitis. However, an unopened abscess poses a serious danger, since it can compress the intestine and provoke the development of intestinal obstruction.
A fistula is a pathological anastomosis between the lumen of the intestine and the cavity of an adjacent internal organ. Such a connection can occur between intestinal loops; intestines and bladder, uterus, vagina. In some cases, a fistula opens on the skin of the abdominal wall, connecting the intestine with the external environment.
The most common are connections between the intestine affected by diverticula and the bladder in men and the vagina in women:
- An enterovesical fistula can be suspected by frequently recurring urinary infections. The diagnosis is confirmed by an x-ray taken after contrast injection into the bladder or intestines. The x-ray will show the leakage of the drug outside the organ being studied.
- Intestinal-vaginal fistula causes severe vaginitis. The release of feces and gases through the vagina allows you to quickly establish the correct diagnosis. However, this does not always happen. If the formed anastomosis is narrow, the described symptoms may not occur. In this case, the woman will complain of purulent discharge, pain, burning and itching in the genital tract. Detection of intestinal flora in vaginal discharge will allow one to suspect the cause of the disease. The diagnosis is confirmed by X-ray examination with contrast.
Peritonitis is characterized by a serious condition of the patient. The abdominal pain is diffuse, the anterior abdominal wall is sharply tense. Severe fever and intoxication are noted. Peritonitis is an extremely dangerous complication that can lead to death.
Another life-threatening condition with diverticulosis is intestinal obstruction. The reasons for this are as follows:
- Compression of the intestine by an abscess or inflammatory infiltrate resulting from diverticulitis or perforation.
- Adhesions in the abdominal cavity (the result of inflammation of diverticula).
- Cicatricial changes in the intestinal wall, resulting from frequent relapses of diverticulitis, contribute to deformation and narrowing of its lumen.
Symptoms of this complication include delayed passage of stool and gas, bloating, nausea and vomiting, and abdominal pain. Obstruction is often incomplete, and can be resolved with conservative methods. However, if the intestinal lumen is completely closed, surgery may be required.
Bleeding from diverticulosis is rarely severe. A characteristic sign of this complication is the appearance of blood in the stool. In this case, melena (black loose stool) is not observed. When bleeding from the lower part of the large intestine - the sigmoid colon - unchanged blood is detected, sometimes in the form of clots, evenly mixed with feces. The patient may experience weakness and dizziness, and a decrease in hemoglobin levels is observed in a general blood test.
Complications of diverticulosis of the sigmoid colon
In the absence of appropriate treatment, developing diverticula in the sigmoid colon can lead to the following complications:
- Bleeding from the rectum. It occurs due to damage to the vessels surrounding the diverticulum, and is characterized by blood in the stool after defecation. The severity of bleeding varies depending on the size of the damaged vessels;
- Diverticulitis is inflammation of the diverticula of the sigmoid colon. The cause is bacteria that, together with feces, are retained in diverticula. Manifested by abdominal pain, mucus in the stool, increased body temperature;
- Perforation (breakthrough) of a diverticulum, with the release of the contents of the sigmoid colon into the peritoneal cavity and the development of peritonitis (inflammation of the peritoneum).
What are the types of diverticula?
Diverticular disease of the sigmoid colon is a special case of diverticulosis of the large intestine. A distinctive feature of the disease is the presence of diverticula, protrusions of the intestinal wall. They can be single or multiple, congenital and acquired. Depending on which structures of the intestinal wall are involved in the pathological process, true and false (complete and incomplete) diverticula are distinguished.
| True diverticulum | False diverticulum |
| The anatomical structure of the protrusion wall is similar to that of the intestinal wall, i.e., it includes the mucous membrane, submucosal layer, muscular and serous membranes. | The wall of the formation contains only the mucous membrane and submucosal layer. A false diverticulum that penetrates into the muscular lining of the intestine, but does not extend beyond its limits, is called incomplete. A false diverticulum extending beyond the intestinal wall is called complete. |
| It is a congenital anomaly. | It is an acquired pathological formation. |
| Emptying of the diverticulum is not impaired. | Emptying is difficult. |
| It is most often localized in the right parts of the colon. | It is most often localized in the left parts of the colon. |
In the vast majority of cases, diverticula are found in the left half of the colon (descending colon and sigmoid colon), which accounts for 90% of cases of diverticular disease. In 10% of patients, total damage to the large intestine is observed. The favorite localization of diverticula is the sigmoid colon (50–65% of cases).
Diagnosis of diverticulosis of the sigmoid colon
When examining a patient, a specialist pays attention to a number of factors: characteristic complaints, the patient’s age, lifestyle, diet, and tendency to constipation. The doctor examines the patient, using palpation to identify painful areas characteristic of the disease.
A detailed history will help clarify the clinical picture and suspect diverticulosis. To confirm the diagnosis, the patient is prescribed a series of laboratory tests and hardware examinations.
- Colonoscopy. A research method that allows you to assess the condition of the intestines from the inside. The procedure is carried out using a special flexible probe with a video camera at the end, which is inserted into the intestines through the anus. The image from the camera is displayed on the monitor, and the doctor can visually assess the condition of the intestinal walls, the presence of diverticula, and even take a piece of tissue for examination.
- Irrigoscopy. During the examination, an X-ray of the intestine is taken, previously filled with a contrast agent. If diverticula are present in the intestine, the contrast agent will fill them, and these pouch-like protrusions will be clearly visible on the image.
- Laparoscopy. It is both a diagnostic and treatment method. During the examination, the surgeon makes three punctures in the abdominal wall, through which a miniature camera is inserted, allowing you to examine the surface of the intestine and, under magnification, notice the slightest changes on its walls. If necessary, your doctor may remove an uncomplicated diverticulum. The procedure is performed under general anesthesia.
In some difficult cases, the patient may be prescribed a survey radiography of the abdominal organs or visual examination methods such as computed tomography and MRI. A method such as ultrasound in this case is not informative and is not used to clarify the diagnosis.
Diagnosis of the disease
If diverticulosis of the sigmoid colon is suspected, treatment begins only after a thorough diagnosis. The doctor takes an anamnesis, learns about hereditary factors, lifestyle and nutrition. Only after this the patient needs to undergo a laboratory and instrumental examination, which includes:
- X-ray (irrigoscopy) with a contrast agent is carried out using a special probe with a camera;
- colonoscopy to monitor the internal condition of the intestines;
- laparoscopy as an additional examination and for the possibility of removal if there are few diverticula and they are uncomplicated.
Ultrasound
At the discretion of the attending physician, additional magnetic resonance imaging and plain radiography are prescribed. Ultrasound is not prescribed for this disease, since the data obtained will not give a clear picture.
Treatment of diverticulosis of the sigmoid colon
The choice of treatment methods for diverticulosis of the sigmoid colon is influenced by a number of factors, which the doctor performing the therapy must take into account. The most important among them are age, form of the disease, general health of the patient, tendency to various kinds of complications, lifestyle and nutrition. The early stage of the disease can be treated with conservative methods and means. For patients with complicated and extremely severe forms of this intestinal pathology, surgical intervention is indicated.
Conservative treatment is carried out comprehensively, and the patient is shown:
- products that restore a healthy environment in the intestines;
- special laxatives that contain lactulose;
- antibiotics with a wide spectrum of effects;
- prokinetics that activate intestinal muscle motility;
- antispasmodics, pain relievers and eliminate spasms of intestinal muscles;
- drugs that eliminate diarrhea and bloating;
- some enzymes aimed at improving the quality of digestive activity.
If diverticular disease is in an extremely advanced form, treatment consists of the following therapeutic measures:
- the intestines are unloaded using a siphon enema;
- gastric lavage is performed;
- inflammation is eliminated using fresh frozen plasma;
- infusion therapy is carried out using crystalloid agents.
Surgical intervention should be resorted to in the following cases:
- formation of fistulas in the rectum;
- extreme aggravation with incessant spasms;
- high probability of formation of a malignant tumor of the rectum.
The surgical operation is carried out in two stages. In the first of them, resection is performed, i.e., the affected tissue of the sigmoid colon is removed. At the second stage, an anastomosis is formed, in which parts of the remaining intestinal tissues are fastened. In addition, the abdominal region is drained, after which antibiotics administered intravenously complete the treatment process.
Types of sigmoid colon diverticulitis
There are several types of diseases. They are classified into stages, and the stages, in turn, can also be divided into certain categories.
Types of diverticulosis, depending on the clinical picture, can be divided as follows:
- Asymptomatic diverticulitis , which is characterized by the absence of any clinical manifestations. Most often, this stage of diverticulosis and characteristic bags in the colon are detected during a general diagnosis of the body or suspicion of gastrointestinal diseases.
- Acute diverticulitis manifests itself through uncontrolled compression of the walls of the colon, as well as problems with the digestive processes and disturbances in the intestinal environment.
- The complicated form of the disease is characterized by uncontrollable pain, a dangerous health condition and requires immediate medical intervention.
The forms of the disease also depend on the type of diverticula. They can be either congenital or acquired. Congenital is characterized by mutations and changes that occurred either to the mother or to the fetus as a result of intrauterine development.
Acquired ones are neoplasms that are formed or formed throughout a person’s life, or over a certain period. There are true and false diverticula.
They are distinguished by the participation of the mucous membrane in the formation process:
- true ones give rise to a disease that occurs as a result of protrusion of two or more membranes;
- false is characterized by protrusion of one mucous membrane.
Diverticula can also be classified according to the progression of the disease. They can be rational, that is, formations that were formed due to the influence of the external environment, and tractional - these are new formations, the formation of which was influenced by constant or periodic stretching of the food walls.
Acquired disease is the most common form of the disease affecting people aged 40 and above. According to recent data, approximately a quarter of the population suffers from colonic diverticulosis.
Traditional medicine recipes for the treatment of diverticulosis of the sigmoid colon
Often, folk methods are used to treat diverticulosis, of which the most common and effective are the following:
- Flaxseed or olive oil. Take 1 tablespoon of oil once a day before bed. Helps relieve inflammation and normalize stool during constipation. During the day you can season various salads with this oil.
- Decoction of slippery elm bark. A teaspoon of dry crushed bark is poured into two glasses of boiling water and heated for 20 minutes over low heat. Then the broth should be cooled, strained and taken cold.
- An infusion of a mixture of herbs. Take motherwort herb, stinging nettle, dill and rose hips, and chamomile flowers in equal proportions. A tablespoon of this mixture should be placed in a thermos, pour a glass of warm (not hot!) water and leave for 1.5 hours. Then you need to strain the infusion and drink 0.5 cups in the morning and evening. The course of treatment is a month.
Treatment
Treatment methods for diverticulosis of the sigmoid intestine depend on the patient’s age, well-being, lifestyle and nutritional specifics, stage of the disease, and the presence of complications. If the diverticulum is single, not inflamed and does not cause discomfort, therapy may be limited to the prevention of constipation and a therapeutic diet.
Can diverticular disease be cured? Diverticulosis without complications is treated with conservative therapy.
Complex drug treatment consists of:
- antibiotics that have a wide spectrum of action on the intestines (penicillins, cephalosporins);
- painkillers and antispasmodics that reduce muscle spasms (No-shpa, Drotaverine);
- prokinetics that stimulate intestinal motor function and have antibacterial, antidiarrheal and antiemetic effects (Motilium, Ganaton);
- laxatives (Microlax, Duphalac);
- enzyme preparations that normalize digestive functions and reduce stress on the intestines (Festal, Mezim);
- drugs to restore intestinal microflora (Bifidumbacterin, Linex);
- medicines for flatulence and diarrhea (Sulgin, Biseptol).
In severe cases of the disease, in addition to drug treatment, the following medical procedures are carried out:
- Gastric lavage.
- Colon cleansing with enemas.
- Infusion therapy is carried out (crystalloid solutions are administered intravenously).
- Fresh frozen plasma is used.
Surgery is performed in cases where there are severe complications that are life-threatening to the patient.
Indications for surgical intervention are:
- heavy bleeding;
- intestinal obstruction;
- peritonitis;
- frequent exacerbation with severe pain;
- rectal fistulas;
- the likelihood of developing rectal cancer and other malignant tumors.
The surgical operation consists of two stages. First, a resection is performed (the inflamed parts of the intestine are removed), then an anastomosis is formed - the remaining parts of the intestine are connected. In addition, according to indications, the abdominal cavity is drained and antibiotics are administered intravenously.
Timely, competent treatment saves the patient from severe complications and allows for a favorable prognosis for subsequent life.
Diet
The diet for diverticulosis of the sigmoid intestine should include foods high in fiber. It is necessary to adhere to fractional meals - eat small portions 5-7 times a day. It is recommended to include boiled, baked and steamed dishes in the daily menu.
Table of products that are allowed or prohibited for intestinal diverticulosis:
| Authorized products | Prohibited Products |
| fruits: apples, persimmons, figs, mangos | berries: raspberries, strawberries |
| vegetables: cucumbers, pumpkin, tomatoes, zucchini, beets, eggplants | baked goods and white bread, confectionery |
| cereals: rice (brown), buckwheat, oatmeal | cereals: semolina, white rice |
| vegetable soups or low-fat meat broth | sausage, smoked meats, canned food |
| kefir, cottage cheese, fermented baked milk, natural yogurt | pasta |
| bran bread | alcoholic drinks |
| dried fruits: prunes, dried apricots | strong tea, coffee, cocoa |
Folk remedies
The patient's condition can be alleviated using traditional medicine. It is necessary to use such drugs as an addition to the main treatment and under the supervision of the attending physician.
The most effective and efficient recipes:
- flaxseed or olive oil. Relieves constipation and relieves inflammation. Drink 1 tbsp. spoon of oil overnight. It is recommended to use olive oil for dressing vegetable salads.
- You will need equal quantities of nettle and motherwort leaves, rose hips, chamomile flowers and dill seeds. Pour 1 tbsp into a thermos. spoon of the mixture, pour 250 ml. boiling water and leave for 2 hours. Drink 100 ml for a month. twice a day.
- one teaspoon of elm bark is poured into a glass of hot water and simmered over low heat for 15 minutes. The broth is cooled, filtered and taken half a glass a day.
- take 150 gr. aloe leaves, chop them and add 300 ml. honey. The mixture is infused for 24 hours, filtered and taken 1 tbsp. spoon an hour before meals.
You should not treat diverticulosis yourself at home using folk remedies, as there are high risks of serious complications of the disease.
Video on the topic:
Dietary nutrition for diverticulosis of the sigmoid colon
It is impossible to completely get rid of existing diverticula.
But each patient has the opportunity to minimize the likelihood of developing an inflammatory process around them.
To do this, there is no way to do without establishing the correct nutrition process - diet.
This needs to be taken extremely seriously.
It is better to entrust the selection of the right diet to a gastroenterologist.
After a detailed examination, he will check the following indicators:
- The patient's intestinal condition;
- Level of muscle tone;
- Degree of development and number of diverticula;
- The presence and magnitude of the inflammatory process;
- Study of the patient's intestinal microflora
To do this, the patient undergoes a series of special examinations. Based on the research data, the specialist makes the final decision.
The selected diet must fall within certain rules:
- You need to eat often, but in small portions;
- All products must be well chopped. This is necessary so that all food is well coated with digestive enzymes, without raising intestinal pressure;
- The basis of the diet should consist of soups - purees or milk porridges;
- The diet must include a large number of foods that contain a large amount of fiber (fruits, bran, berries, vegetables, etc.);
- The patient should take plenty of fluids between meals. Ideally, these should be herbal decoctions, jelly, compotes;
- If a patient often experiences constipation, it is better not to abuse laxatives, but to drink laxative herbal decoctions: rose hips, prunes, etc.;
- Eliminate from the diet alcoholic drinks, cigarettes, spicy and smoked, sour and salty foods, as well as foods that contain caffeine;
- It is better to replace baked goods made from white bread with those containing bran;
- Avoid sweets and replace them with berries or bananas;
- Instead of apple juice, it is better to eat a raw apple with peel;
- Eat as many baked vegetables and fruits as possible without peeling them;
- Eat bran with kefir or milk;
- Eat vegetarian soups – purees, which include barley groats – once a day;
- It is better to replace beef with beans.
Specialist nutritionists and gastroenterologists recommend that when choosing a diet for patients who have developed diverticula of the sigmoid colon, treatment and diet should not include foods (berries, fruits) that contain seeds. Under no circumstances should you eat strawberries or grapes, nuts or raspberries.
Description of diverticulosis
Diverticula are unusual protrusions (growths) that resemble a hernia, a hemorrhoid based on the intestinal walls. They can arise in a person throughout his entire existence, without manifesting himself in any way. The appearance of diverticula is called diverticulosis. If these growths become inflamed, a pathology such as diverticulitis occurs. There may be single or multiple intestinal protrusions. Diverticulosis affects people over 60 years of age, but there are cases of the disease developing at an earlier age.
Alcohol abuse, eating fried, fatty foods, and poor nutrition can cause the formation of diverticulosis of the sigmoid colon.
The disease is not congenital. Often this is the impact of unfavorable, irritating factors. Protrusions are not always based on the mucous membrane; they can come out and be located on the outer walls of the intestine. Diverticulosis does not pose a significant danger, but if certain rules are not followed, an exacerbation is possible, which in this situation threatens not only health.
Prevention of diverticulosis of the sigmoid colon
The most important condition for the prevention of this disease is normal intestinal motility, that is, the absence of constipation.
To maintain regular bowel movements you need to:
- perform physical exercises aimed at the abdominal muscles;
- eat enough fiber. The norm recommended by American nutritionists is 20-35 g of fiber. This is exactly what every person should strive to consume. Fiber-rich foods: whole grain bread, berries, vegetables, fruits, brown rice, bran, beans and peas. Thanks to such food, you can prevent constipation and improve your health, lower blood pressure, reduce cholesterol in the blood and the likelihood of developing certain types of intestinal disorders;
- drink enough fluids. If there are no contraindications, the daily norm is at least 8 glasses of water;
- get proper rest and sleep.
About sigmoid diverticulosis
Diverticulosis is an acquired disease, although there are also cases of congenital disease. Divericulum is a small protrusion of the intestine of a hernial nature. If there are a lot of them, we are talking about diverticulosis, but if the walls of the protrusion are inflamed, we are talking about diverticulitis. Doctors gave this disease a general name - diverticular, this also includes all complications and gave the code K57 in ICD 10. Congenital diverticula received a different code in ICD 10 - Q43.8. Diverticula in other parts of the intestine have a different ICD 10 code, but most often they are still found in the sigmoid colon, that is, the left part of the colon. The main cause of the disease is considered to be a lack of fiber in our diet: indeed, every 10 years the diet of Americans and Europeans becomes increasingly poor in this element, while in almost vegetarian India and Africa with its vegetable menu, symptoms of diverticular disease are much less common. By the way, Africans are more likely to have diverticula of the right half of the intestine rather than the left, but that’s a different story. But the history of colon diverticulosis is relatively young: not 10 years, however, after all, humanity has been moving towards such a harmful diet for more than a century, but in the 18-19 centuries such symptoms were less common. Most often, diverticula occur in people over 80 years of age, but in young (under 50) patients - less than 10 percent.
Causes and consequences
Diverticula develop against the background of impaired collagen synthesis and connective tissue dysplasia. With a congenital disease, diverticula form not only in the small and large intestines, but also in other organs of the abdominal cavity and retroperitoneal space.
Acquired intestinal diverticulosis is largely promoted by the patient’s irrational diet, when the diet is dominated by:
- Flour;
- Sweet;
- Fatty meats;
- Semi-finished products;
- Fast food.
There is a deficiency of fiber (vegetables and fruits) in the human menu. He eats irregularly and eats large portions. Due to minimal amounts of plant foods and clean drinking water, persistent constipation occurs, sometimes accompanied by flatulence. Frequent constipation leads to increased intraintestinal pressure, stretching of the intestinal walls and injury to the mucous membrane from solid feces.
In addition to irrational nutrition, the causes of intestinal diverticulosis are:
- Physical inactivity;
- History of intestinal infections;
- Obesity;
- Hypovitaminosis;
- Uncontrolled and frequent use of laxatives.
Acquired intestinal diverticulosis often develops in old age: in people over 45-60 years old in 25-35% of cases, in people over 75 years old - in 65% of cases. By localization, diverticulosis occurs in the colon (70%), sigmoid colon (sigmoid colon) and rectum. In the small intestine, a pathological process develops only in 1% of cases.
How dangerous is intestinal diverticulosis?
Its complications include:
- Extensive inflammation (diverticulitis);
- Recurrent intestinal bleeding;
- Perforation of diverticula with release of feces into the peritoneal cavity;
- Interintestinal abscess;
- Adhesive bowel disease;
- Peritonitis (local or diffuse).
With perforation of diverticula, the clinical picture of an “acute abdomen” develops, caused by infection of the peritoneum with feces.
Diverticula are not prone to malignancy (malignant degeneration).
Causes of sigmoid diverticulosis: course of the disease and complications
The cause of the disease is poor nutrition
It was noted above that the incorrect menu of our contemporaries is to blame for the disease, and any nutritionist will agree with this. But excess weight, as well as physical inactivity, can affect the development of the disease. But most often it is nutrition that is to blame for the formation of dense feces, which stretches the intestinal wall and injures it. The peristalsis of the large intestine (and not only) is disrupted; its mucous membrane is pushed through the intestinal muscles and submucosal layer. This is how protrusions with a thin neck appear in the colon, which stretch and grow over time. The disease can be asymptomatic, have pronounced symptoms, or be complicated.
Pain in the left side of the abdomen
Typically, people do not know about diverticulosis until the diverticula become inflamed or the disease is “found” simply by examination. The only symptoms are pain in the left side of the abdomen that goes away after gas or bowel movements. But usually people believe that this is just an accumulation of gases and a doctor is not needed, and sometimes they are saved by folk remedies.
If the diverculae are inflamed, symptoms such as pain may be observed, which intensify when pressing on the area of the colon and when turning on its side, which does not hurt. Only one point hurts, but for several days. The usual symptoms of diverticulitis are constipation alternating with diarrhea, fever, bloated abdomen, and slight nausea. In this case, the doctor may suspect not only diverticulitis, but also appendicitis or renal colic. Treatment, and urgent treatment, is necessary in all cases.
If the diverculum ruptures, peritonitis or an abscess may occur, because in this case the contents of the inflamed intestine will be released into the abdominal cavity.
If the contents of the diverculum enter the large intestine, more precisely, between its mesenteries, symptoms such as severe weakness and pain are possible. This is a paracolic abscess. Also, if there is a rupture, you can get bleeding (if there is an ulcer in the diverculum) or a fistula.
A case of ultrasound diagnosis of colon diverticulitis
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Introduction
According to the literature, the prevalence of colon diverticulosis in different countries reaches 30% in the entire population and 40% among people over 70 years of age [1, 2, 4].
Diverticula are localized in different parts of the colon with different frequencies: in the sigmoid colon - in 60-85% of patients, in the descending colon - in 13-24%, in the transverse colon - in 5%, in the ascending colon - in 6-17%, in the cecum intestine - in 3% of patients. Total damage to the colon is quite rare and, according to statistical data, its frequency does not exceed 5% [3].
The highest incidence of diverticula formation in the sigmoid colon is explained by the fact that the diameter of its lumen is smaller, therefore the wall tension during peristaltic movements, as well as the intraluminal pressure, is greater.
A diverticulum occurs as a result of protrusion of the mucous membrane through the muscular layer of the intestinal wall at its weakest points. Modern ideas about diverticular disease are based on the leading role of the vascular factor in its development: with spasm of the muscle layer, intrawall vessels are compressed with impaired microcirculation - ischemia and slowing of venous outflow. All of the above leads to dystrophic changes and expansion of the perivascular spaces, which subsequently become the mouths of diverticula. Thus, diverticula are the final manifestation of a disease of the intestinal wall, fiber disintegration of the circular muscle layer, atrophy and its expansion in weak areas (in the area of perforating vessels).
In most cases, the disease occurs without any clinical symptoms; complications develop in 10-20% of patients. Among the complications, acute diverticulitis predominates (60%), less common are peridiverticular infiltrate (11.9%), abscess (7.1%), intestinal bleeding (15.1%), perforation (4.9%) and intestinal obstruction (1). .0%) [3].
The most common symptoms of diverticulitis are a sudden onset of abdominal pain and abnormal bowel movements. Since diverticula and, accordingly, diverticulitis can occur in any part of the colon, the symptoms of diverticulitis can resemble a variety of diseases: from gastric and duodenal ulcers, acute appendicitis, intestinal ischemia, intestinal obstruction, colon cancer to renal colic and adnexitis. Signs of inflammation, such as fever and leukocytosis, help distinguish diverticulitis from the cramping pain of irritable bowel syndrome [5].
In addition to clinical and laboratory tests, instrumental studies play an important role in diagnosing diverticulitis, usually listed in the following order: plain radiography of the abdominal organs, irrigoscopy, computed tomography, ultrasound and endoscopy. However, in recent years, marked by the accumulation of experience in ultrasound examination of hollow organs, this sequence may be revised. In connection with the above, we consider it necessary to present the following clinical observation.
Clinical observation
Patient B., born in 1944, contacted a gastroenterologist at the clinic with complaints of constant aching pain of moderate intensity in the left lower abdomen, lasting for 2 days after an error in diet, an increase in body temperature to 38.5°C, general weakness, malaise . Medical history: 10 years ago - combined treatment for stage I right breast cancer (RME+RT+HT), stage 2 hypertension, moderate type 2 diabetes mellitus, diabetic polyneuropathy, chronic gastroduodenitis, condition after extirpation uterus with appendages due to fibroids.
Upon examination, the patient's condition is relatively satisfactory. The skin and visible mucous membranes are of normal color. The abdomen is soft on palpation, painful along the descending part of the colon, in the left iliac region. The liver is not enlarged and not palpable. “Bubble” symptoms are negative. Constipation for 2 days. Pasternatsky's symptom is negative on both sides. There is no dysuria. An urgent general blood test showed moderate leukocytosis (9700).
With suspicion of diverticulitis, the patient was sent for an urgent ultrasound examination of the abdominal organs, kidneys and pelvic organs. The study was performed on a modern device with a 3.5 MHz convex probe, a 7.5 MHz linear probe and an endovaginal probe with a variable frequency of 5.0-7.5 MHz using color and power Doppler mapping.
Ultrasound revealed diffuse changes in the liver and pancreas, signs of chronic acalculous cholecystitis, angiomyolipoma of the left kidney (without dynamics for several years), and a condition after extirpation of the uterus and appendages. In the left iliac region, corresponding to the zone of maximum palpation pain over a distance of 9 cm, thickening of the walls of the colon to 6-7 mm was noted (Fig. 1). There was no intestinal peristalsis, haustration was weakly expressed, while several painful protrusions of low echogenicity, painful when pressed with a sensor, ranging in size from 7 to 20 mm (Fig. 2, a, b) with a thin wall up to 0.9-1.1 mm and the presence of in some of them there were fragments of intestinal contents and gas (Fig. 3, a, b).
Rice. 1.
Sonographic picture of diverticulitis. Transabdominal examination with a 7.5 MHz linear sensor.
"Symptom of an affected hollow organ."
Rice. 2.
Sonographic picture of diverticulitis. Transabdominal examination with a 7.5 MHz linear sensor.
A)
Longitudinal section.
b)
Cross section.
Rice. 3.
Sonographic picture of diverticulitis. Transabdominal examination with a 3.5 MHz convex probe.
A)
Longitudinal section.
b)
Cross section.
Transvaginal ultrasound (Fig. 4) also visualized a fragment of the colon with thickened hypoechoic walls and several rounded diverticula up to 1 cm in diameter. The contours of one of the diverticula were uneven and had a star-shaped shape. There was thickening and increased echogenicity of the peri-intestinal fatty tissue compared to the contralateral side. When examined using ultrasound angiography, the thickened intestinal wall and diverticula were avascular, and the surrounding tissue was hypervascular.
Rice. 4.
Sonographic picture of diverticulitis. Transvaginal examination with a 7.5 MHz convex probe.
With suspicion of acute diverticulitis, the patient was hospitalized in the proctology department of the Central Clinical Hospital. 4 days after treatment with antispasmodics and antibiotics, the pain syndrome was relieved and the patient was discharged for a routine outpatient follow-up examination.
During irrigoscopy, performed 4 weeks after the patient was discharged from the hospital (Fig. 5), the colon was examined under double contrast conditions. All sections and the usually located vermiform appendix were filled with barium suspension and air. The barium suspension did not penetrate into the small intestine. The sigmoid colon was lengthened. The location of the loops is normal, the contours are smooth, clear, the walls are elastic. Haustration is well expressed, uneven in the left half. In the left half, mainly in the sigmoid colon, multiple diverticula of different sizes were identified, in the area of the hepatic flexure - single small diverticula. No intestinal deformations, narrowing of the lumen, or intraluminal formations were detected. Bowel emptying is incomplete and uneven. Conclusion: diverticulosis of the colon with a predominant lesion of the left parts.
Rice. 5.
X-ray picture of colon diverticulosis. Irrigoscopy under double contrast conditions.
During a control ultrasound examination after 6 months, when examining the left iliac region, the thickness of the walls of the descending colon and sigmoid colon did not exceed 3-5 mm (Fig. 6, a, b); during observation for 1 year, no signs of relapse were noted.
Rice. 6.
Sonographic picture of the colon. Control transabdominal study with a 3.5 MHz convex sensor after 6 months.
A)
Longitudinal section.
b)
Cross section.
Discussion
Predisposing factors for the development of diverticulitis are considered to be old age (the most significant factor), corticosteroid and immunosuppressive therapy, and chronic renal failure.
As a rule, the examination of such patients begins with a survey radiography of the abdominal organs, which can detect intestinal obstruction, intestinal paresis, tumor formation, signs of ischemia and intestinal perforation. Thus, the method is actually effective in the event of complications of acute diverticulitis.
Irrigoscopy can lead to an exacerbation of the disease and be more harmful than useful, since barium entering the abdominal cavity in case of perforation of the diverticulum can cause chemical peritonitis. However, special studies have confirmed that barium enema may not harm the patient and can actually be of great benefit when using water-soluble contrast agents. For mild to moderate diverticulitis, when the diagnosis is not completely clear, fluoroscopy with a water-soluble contrast agent is safe and of great help; In case of severe disease, it is advisable to postpone the examination for 6-8 weeks. Thus, the method has a number of limitations associated with the acute period of the disease.
Colonoscopy, in addition to determining the presence of diverticula, makes it possible to clarify the extent of inflammatory changes in the intestinal lumen, the location of diverticula and the condition of their mucous membrane: hyperemia and swelling of the mucous membrane in the area of diverticula, the presence of pus in the intestine. However, acute diverticulitis is a relative contraindication to endoscopic examination, since manipulation of the endoscope and inflating the intestine with air can lead to perforation of diverticula and the development of an abscess or peritonitis. Colonoscopy should be performed only in cases where the diagnosis is unclear and the differential diagnosis is between occlusive tumor, intestinal ischemia, inflammatory bowel disease and infectious colitis. Thus, the method has almost the same limitations as X-ray contrast studies.
Computed tomography is performed in all cases of diverticulitis with a palpable tumor formation in the abdomen or clinically significant intoxication, in the absence of the effect of conservative therapy; it is the method of choice for diagnosing complicated diverticulitis. Computed tomography allows you to carefully examine not only the intestinal wall, but also organs and tissues beyond it, and helps to detect diseases not associated with diverticulitis, such as ischemic colitis, mesenteric thrombosis, tubo-ovarian abscess and pancreatitis. Diagnostic criteria for acute diverticulitis on computed tomography are local thickening of the colon wall (more than 5 mm), inflammation of the peri-intestinal fatty tissue, or the presence of a peri-intestinal abscess. Although the method does not have limitations associated with the acute period of the disease, it still cannot compete with ultrasound in terms of accessibility to the population.
Ultrasound scanning is the safest non-invasive method for diagnosing acute diverticulitis, which can be used at any stage of the disease. The lack of information content of this study is a consequence of the large amount of gases in the intestine. False negative results are observed in 20-25% of observations in the absence of false positive conclusions. The result of the test largely depends on the skill of the doctor: when performed by an experienced researcher, the sensitivity is 74.2%. The results of an ultrasound examination are close to the results of a computed tomography scan. In this case, in patients with diverticulitis, thickening of the intestinal wall with the presence of saccular or triangular formations extending beyond the contour of the altered segment of the intestine, infiltration of peri-intestinal fatty tissue, intramural fistulas, stenosis of the colon with characteristic changes in the diameter of the lumen: narrowing at different lengths with a thickened due to the muscular layer of the wall and suprastenotic expansion. Intestinal strictures that develop as a result of a malignant tumor are characterized by sharp boundaries on both sides, while strictures that develop as a result of diverticulitis are characterized by smoother contours and greater extent [4, 6, 7].
In the above observation, ultrasound visualized multiple protrusions of the thinned intestinal wall. In areas of the thickened wall between the diverticula and in the diverticula themselves, the vascular pattern was depleted or not visualized, which confirms the role of the vascular factor in the development of the disease: compression of intramural vessels with impaired microcirculation, the presence of ischemia and slowing of venous outflow. Some diverticula were filled with homogeneous avascular contents of moderate echogenicity, without signs of intraluminal movement, so that the contents merged with the image of the wall. In other diverticula, gas bubbles, acting as a natural contrast, made it possible to examine in detail the intestinal wall, thinned to 0.9-1.1 mm, devoid of a hypoechoic muscle layer. The shape of these diverticula was close to spherical; the orifice was smaller than the diameter of the diverticulum. However, there were also protrusions in the shape of cones, with orifices exceeding the size of the diverticulum itself; in them, a continuation of the hypoechoic muscular layer of the wall could be traced.
Obviously, this difference in the ultrasound image of diverticula reflects the stages of their formation: rounded ones with a thinned wall and the absence of a muscle layer in it are formed diverticula, while others in which the muscle layer or its fragments are still visible are diverticula at the stage of formation.
Thus, gas in the intestine can not only be an obstacle to adequate visualization, but also, being a natural contrast agent, significantly enriches the ultrasound picture.
conclusions
For abdominal pain syndrome, ultrasound is the safest non-invasive diagnostic method that can be used at any stage of the disease, it provides important information and should be used if diverticulitis is suspected, in particular, in an outpatient setting in all cases.
Literature
- Vorobyov G.I., Zhuchenko A.P., Achkasov S.I. and others. Prediction of the development of repeated inflammatory complications after an episode of acute diverticulitis // Materials of the Second Congress of Coloproctologists of Russia with international participation “Current Issues of Coloproctology”. Ufa, 2007. pp. 405-406.
- Timerbulatov V.M., Fayazov R.R., Mehdiev D.I. and others. Own experience in the treatment of complicated forms of diverticular disease of the colon // Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2009. N5. pp. 68-71.
- Khalilov Kh.S., Khadzhimukhamedov N.A. Results of diagnosis and treatment of complicated forms of colon diverticulosis // Sat. abstract First International Conf. in thoracoabdominal surgery. M., 2008. pp. 42-43.
- Vorobyov G.I., Orlova L.P., Zhuchenko A.P., Kapuller L.L. Ultrasound signs of diverticular disease of the colon // Coloproctology. 2008. N1. pp. 7-8.
- Murphy T., Hunt RH, Fried MD et al // Diverticular disease. WGO-OMGE Global Guidelines. 2005. P. 44-49.
- Orlova L.P., Trubacheva Yu.L., Markova E.V. Ultrasound semiotics of diverticular disease of the colon and its chronic inflammatory complications // Ultrasound and functional diagnostics. 2008. N3. C. 18-25.
- Satsukevich V.N., Nazarenko V.A. Clinical and ultrasound diagnosis of colon diverticulitis and its complications // Surgery. 2005. N5. pp. 47-50.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.