General information
Gastrointestinal bleeding is the most common complication of acute and chronic pathology of the digestive system, and poses a potential danger to the patient’s life.
The source of blood loss can be in any part of the gastrointestinal tract: esophagus, stomach, intestines (small and large). In abdominal surgery, gastrointestinal bleeding ranks 5th in frequency of occurrence after acute appendicitis , pancreatitis , cholecystitis , and strangulated hernia . ICD-10 code for gastrointestinal bleeding: K92.2 - Gastrointestinal bleeding, unspecified.
Pathogenesis
Gastrointestinal bleeding occurs due to a violation of the integrity of blood vessels when their walls rupture, erosion , increased permeability, aneurysm , thrombosis , embolism , etc. Blood loss can also occur due to changes in the hemostatic (blood clotting disorders, thrombocytopenia , thrombocytopathy ). There are cases when both hemostasiological and vascular components are involved in the bleeding mechanism.
Hemobilia is gastrointestinal bleeding resulting from traumatic injury to the liver. Medical history is extremely rare.
Classification
Depending on the affected part of the digestive tract, bleeding is distinguished:
- From the upper sections (esophageal, gastric and duodenal). It accounts for 80-90% of all gastrointestinal bleeding.
- From the lower sections (from the small or large intestine, from hemorrhoids). The occurrence rate is 10-20%.
According to the etiopathological mechanism:
- ulcerative hemorrhages;
- non-ulcer hemorrhages.
By duration:
- spicy;
- chronic.
According to the severity of clinical symptoms:
- hidden;
- obvious.
By frequency:
- one-time;
- recurrent.
By severity:
- lung;
- average;
- heavy bleeding.
Classification of bleeding according to Forest:
- FI - ongoing bleeding;
- FIA - jet bleeding from an ulcer;
- FII—complete bleeding;
- FIIA - thrombosed vessels at the bottom of the ulcer (high risk of relapse);
- FIIB - blood clot covering an ulcerative defect (low risk of relapse);
- FIIC - ulcer without signs of bleeding;
- FIII - no sources of bleeding were found.
Forest classification is necessary to determine patient management tactics.
Description
Intestinal bleeding.
Leakage of blood from the lower digestive tract. It manifests itself as symptoms of the underlying disease, as well as the presence of fresh blood during bowel movements (mixed with feces or located in the form of clots on the feces). For diagnosis, rectal digital examination, endoscopy of the small and large intestine, angiography of mesenteric vessels, scintigraphy with labeled red blood cells, clinical and biochemical blood tests are used. Treatment is usually conservative, including therapy of the underlying disease and replacement of blood loss. Surgical treatment is required for severe intestinal damage (thrombosis, vascular ischemia, necrosis).
Causes of gastrointestinal bleeding
There are more than 100 known diseases that can be accompanied by bleeding from the digestive tract. Conventionally, all causes of intestinal bleeding can be divided into 4 groups:
- Blood diseases. Such as hemophilia , vitamin K deficiency , hemorrhagic diathesis , acute and chronic leukemia . Predisposing factors may include contact with chemicals, stress, alcohol intoxication , taking corticosteroids or aspirin.
- Portal hypertension. The pathology occurs against the background of chronic hepatitis , liver cirrhosis , constrictive pericarditis , which compresses the portal vein with scars and neoplasms. The reasons may lie in thrombosis of the portal vein system or thrombosis of the hepatic veins.
- Damage to blood vessels. The pathology is associated with scleroderma , rheumatism , atherosclerosis , Rendu-Osler disease , vitamin deficiency C , systemic lupus erythematosus , and thrombosis of mesenteric vessels. Bleeding may begin from varicose veins of the esophagus.
- Damage to the digestive tract. Pathology occurs with peptic ulcer of the digestive tract, Crohn's disease , esophagitis , anal fissure , helminthiasis , neoplasms , injuries ( hemobilia ).
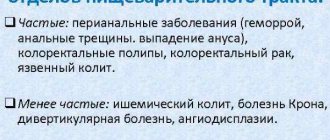
Causes
The cause of bleeding can be a variety of diseases of the intestines and mesenteric vessels. Angiodysplasia of the vessels of the small and large intestines can only manifest as bleeding and have no other clinical signs. Intestinal diverticulosis is the most common cause of bleeding. Also, intestinal bleeding often accompanies chronic (Crohn's disease, ulcerative colitis) and acute inflammatory bowel diseases (pseudomembranous colitis); specific pathology of the small or large intestine (tuberculous colitis). Also, intestinal bleeding can result from lesions of the mesenteric vessels - intestinal ischemia due to spasm or thrombosis of the mesenteric arteries. Massive bleeding results from tumor pathology (cancer, intestinal polyps). The source of intestinal bleeding can be hemorrhoids and anal fissures. In children, foreign bodies in the digestive tract are a common cause of intestinal bleeding. More rare factors that provoke intestinal bleeding include radiation colitis after radiation therapy, aorto-intestinal fistulas, hookworm disease, intestinal syphilis, amyloidosis, and long marathon races in athletes. In less than 10% of cases, the cause of intestinal bleeding cannot be identified.
Symptoms of gastrointestinal bleeding
Direct symptoms of bleeding in the gastrointestinal tract (upper section):
- hematemesis (vomiting blood);
- tarry, black stools.
Vomiting blood often accompanies voluminous blood loss and is combined with melena. With esophageal arterial bleeding, vomiting with practically unchanged blood is observed. Blood loss from the veins of the esophagus is often profuse in nature and is manifested by vomiting with dark cherry-colored blood.
Signs of stomach bleeding
Bleeding in the stomach is accompanied by "coffee ground" vomiting due to the formation of hematin chloride .
Indirect symptoms:
- clinical signs of anemia;
- clinical symptoms of BCC deficiency (including hypovolemic shock ).
Signs of bleeding in the intestines
One of the signs of intestinal bleeding is the appearance of melena approximately 8 hours after the start of bleeding when the volume of lost blood is more than 50 ml. With accelerated transit (less than 8 hours) and a blood volume of more than 100 ml, hematochezia - stool with scarlet blood.
Often, obvious blood loss from the lower digestive tract is moderate and is not accompanied by a drop in blood pressure or other symptoms. Sometimes patients talk about periodically disturbing intestinal bleeding only after careful questioning. It is extremely rare that massive blood loss from the lower gastrointestinal tract is diagnosed, accompanied by acute posthemorrhagic anemia , hypovolemia , tachycardia , and arterial hypotension .
Symptoms of internal bleeding
The color of the released blood is important when bleeding from the gastrointestinal tract. The lighter the blood released from the rectum, the more distal the source of blood loss is located.
Scarlet blood indicates damage to the sigmoid colon. The appearance of dark red blood indicates proximal damage to the large intestine.
Symptoms indicating damage to the perianal area (anal fissure, hemorrhoids):
- discharge of scarlet blood or its drops without fecal impurities;
- feces retain their color and do not contain clots or impurities.
If the source of blood loss is proximal to the rectosigmoid region, then the blood is evenly mixed with the feces.
Pain in the epigastrium that precedes intestinal bleeding indicates the presence of an acute infectious process or chronic inflammatory bowel disease. The reason may lie in acute ischemic lesions of the small or large intestine.
Pain that occurs in the rectal area during defecation or intensifies after it is characteristic of anal fissure or hemorrhoids . The absence of pain with massive blood loss indicates telangiectasis or diverticulosis .
Symptoms
The nature and intensity of rectal bleeding depend on the underlying pathology. With anal fissures, patients complain of intense pain during bowel movements. Blood is separated in small quantities and is found in the form of small bright red smears on toilet paper. With hemorrhoidal rectal bleeding, similar symptoms may be observed, but there is no severe pain during defecation. Some patients experience prolapse of hemorrhoids. The blood is often bright scarlet, although dark clots are also possible. Rectal bleeding with hemorrhoids is more intense, and anemia may develop. With diverticulitis, rectal bleeding develops relatively infrequently, but can be profuse, requiring emergency treatment measures. The type of blood depends on the location of the diverticulum. With damage to the sigmoid colon, the blood is bright red, with diverticula of the right parts of the colon - dark burgundy, sometimes almost black. Patients are concerned about abdominal pain, fever and hyperthermia resulting from inflammation of the mucous membrane of the diverticulum. Rectal bleeding due to diverticulitis may stop on its own and then recur after several months or even years. Rectal bleeding with colon polyps can occur against the background of subjective well-being or abdominal pain and bowel movements. The intensity of such bleeding is usually low, but their frequent repetition can cause the development of anemia, especially with hereditary familial polyposis with the presence of a large number of villous polyps prone to bleeding. Rectal bleeding with colorectal cancer is initially minor; blood can be detected in the stool in the form of clots or streaks. As the tumor disintegrates, the volume of blood released may increase. Along with anemia, abdominal pain and bowel disorders, common manifestations of cancer are observed: weakness, weight loss, lack of appetite, hyperthermia and intoxication syndrome. Rectal bleeding with angiodysplasia is not accompanied by any symptoms. There are no abdominal pains or bowel disturbances. Anemia may develop. The color of blood in polyps and cancer depends on the location of the node. The higher the tumor is located, the darker the blood that is released. With angiodysplasia, this pattern is less pronounced; the blood often has a bright red tint.
Treatment of gastrointestinal bleeding
The first task in acute bleeding is to stop it in a timely manner and prevent emergency surgery. This tactic is due to the high mortality rate when performing surgery at the height of bleeding. Empirical treatment does not require an accurate diagnosis, which requires invasive intervention.
Empirical therapy is started immediately after the patient is admitted to the intensive care unit against the background of infusion treatment. The importance of the event increases when it is impossible to conduct an endoscopic examination for a number of specific reasons.
Empirical treatment for gastric bleeding consists of gastric lavage with as cold water as possible and the use of medications that reduce acidity (parenterally). Ice water allows you to slow down the blood flow in the stomach wall and temporarily stop bleeding . Lavage allows you to empty the stomach of blood clots, which will facilitate gastroscopy.
According to statistics, peptic ulcers occupy a leading position among the causes of blood loss in the upper digestive tract, which is why parenteral administration of proton pump inhibitors and histamine receptor blockers is justified. Pepsin promotes platelet and is inactivated by high acidity of gastric juice , therefore, reducing the acidity of hydrochloric acid increases blood clotting . Properly carried out empirical therapy allows not only to gain time, but also to prepare the patient before endoscopic examination or surgery.
The doctors
Medicines
- Acylok;
- Octreotide;
- Tranexam.
Procedures and operations
The extent of surgical intervention depends on the cause of internal bleeding, the patient’s condition, and the degree of risk of surgical intervention.
Operations are divided into radical and palliative. In case of gastric ulcer, surgery is performed according to Billroth 1 and 2, suturing the bleeding vessel, removing the ulcer with vagotomy according to Jad.
In Boerhave and Mallory-Weiss syndrome, a spontaneous rupture of the mucous membrane or wall of the stomach or esophagus is sutured.
Differential diagnosis
| Diagnosis | Rationale for differential diagnosis | Surveys | Diagnosis exclusion criteria |
| Bleeding from acute ulcers and erosions of the stomach and duodenum | More often, stress, medication use, severe trauma, major surgery, diabetes mellitus, warfarin use, heart failure | CBC, FEGDS, histological examination of biopsy specimens | On FEGDS - Multiple defects of various sizes |
| Hemorrhagic gastritis | More often after prolonged use of drugs, alcohol, against the background of sepsis, acute renal failure and chronic renal failure | CBC, FEGDS, histological examination of biopsy specimens | On FEGDS there is no ulcerative defect. Swelling of the mucous membrane, hyperemia, copious mucus |
| Mallory-Weiss syndrome | Suffers from toxicosis of pregnancy, acute pancreatitis, cholecystitis. More often after prolonged and heavy drinking of alcohol, repeated vomiting, first with food, then with blood | CBC, FEGDS, histological examination of biopsy specimens | The presence of longitudinal ruptures of the mucous membrane in the esophagus and gastric cardia of varying lengths |
| Bleeding from the esophagus and stomach | History of hepatitis, abuses alcohol, suffers from cirrhosis and hypothyroidism | CBC, FEGDS, histological examination of biopsy specimens | The presence of varicose veins of the esophagus and gastric cardia of various diameters and shapes |
| Bleeding from disintegrating cancer of the esophagus, stomach | Presence of minor symptoms: increased fatigue, increasing weakness, weight loss, taste distortion, change in pain irradiation | CBC, FEGDS, histological examination of biopsy specimens | The presence of a large ulcerative defect of the mucous membrane, undermined edges, bleeding on contact, signs of mucosal atrophy |
First aid
Emergency care algorithm for gastric bleeding
After calling an ambulance, the patient must be given first aid:
- Ensure immobility and rest, place the patient on a flat surface. If there is heavy bleeding, it is recommended to elevate your legs slightly.
- Emergency care for vomiting: turn the patient on his side to prevent backflow of vomit.
- Place ice or a bottle of cold water on the stomach area to reduce the severity of pain and slow down bleeding.
- Provide a flow of fresh air, because blood loss is accompanied by severe oxygen starvation.
- Monitor the patient’s condition and do not leave him alone until the team arrives.
- Stomach bleeding is often accompanied by thirst. Under no circumstances should the patient be allowed to drink. You are only allowed to rinse your mouth with cold water.
Hemorrhage into the stomach may be accompanied by loss of consciousness. In this case, it is necessary to return the patient to consciousness using cotton wool with ammonia.
First aid is especially important in severe conditions when a person begins to lose consciousness. In this case, it needs to be “returned” using ammonia (a few drops on a cotton swab and allowed to inhale). Control of pulse and breathing is important. To alleviate the condition, from time to time you need to wipe the patient’s face and neck with a damp cloth.
Treatment
TREATMENT
Tactics before surgery • Emergency hospitalization of the patient in a surgical hospital. Transportation - lying on a stretcher • Complex hemostatic therapy •• Infusion ••• Aminocaproic acid - 5% r - r 200 ml ••• Etamsylate - 250 mg IV ••• Calcium chloride or gluconate - 10% r - r 10 ml IV ••• Fibrinogen - 1-2 g per 250 ml 0.9% solution of sodium chloride ••• Menadione sodium bisulfite - 1% solution - solution 3 ml IM •• Local ••• Cold to the epigastric area ••• Gastric lavage with ice water ••• Insertion of a Sengstaken-Blakemore probe for bleeding from varicose veins of the esophagus, injection of epinephrine or norepinephrine (0.1% p - p 4 ml) into the stomach through the tube, along with 100-150 ml of 5% p - ra aminocaproic acid (or give 1 tablespoon of this mixture to drink every 15 minutes) •• Therapeutic endoscopy. Incision of an ulcer 0.1% p - rum of epinephrine or norepinephrine, electrocoagulation, laser coagulation, suturing of the vessel with a metal clip, application of medical glue MK No. 6, 7, 8 •• Endovascular embolization of a bleeding vessel using superselective injection of an artificial embolus through the femoral artery • Correction volemic disorders •• Replenishment of blood volume. Transfusion of blood and its components: 60–80% of the deficit of bcc, native plasma, dry frozen - 200–800 ml, dextrans, albumin, protein, crystalloids •• Stabilization of hemodynamics •• Elimination of metabolic acidosis - sodium bicarbonate (4% p - p 200 ml) •• Restoration of microcirculation - rheopolyglucin 400 ml IV, pentoxifylline 5-15 ml in 250 ml 0.9% sodium chloride solution • Antiulcer therapy: etiotropic for peptic ulcers and prevention of stress ulcers for other types of bleeding. Antacids, H2 blockers of histamine receptors (famotidine, etc.), proton pump inhibitors (lansoprazole, omeprazole, etc.) are prescribed. • The issue of stopping bleeding is decided on the basis of FEGDS data or a probe test: the patient is given a gastric tube and the stomach is washed to clean water . If persistent rinsing fails to achieve clean water and there is fresh blood in the rinsing water, this indicates ongoing bleeding. If it is possible to wash the stomach, then a thin probe is left for dynamic observation. Resumption of bleeding will manifest itself as the release of fresh blood through the probe.
Surgery
• Indications for surgery •• Emergency surgery - up to 2 hours from the moment of hospitalization: ongoing bleeding of II-III degrees of severity, ineffectiveness of endoscopic hemostasis, recurrent bleeding •• Urgent surgery - the presence of a high risk of recurrent bleeding according to endoscopy •• Planned operations are performed when stabilization of the condition and the presence of indications for surgical treatment without taking into account the fact of bleeding (in the case of duodenal ulcer - the presence of complications requiring surgical correction) •• Patients with grade IV severity require urgent resuscitation care and, when hemodynamics are restored to the level of II-III severity of blood loss (pulse - 120-130 per minute, blood pressure - 60-80 mm Hg), emergency surgery. Preparation for surgery includes the entire range of conservative therapeutic measures (mainly correction of volemic disorders and metabolic acidosis).
• The purpose of the operation is to achieve reliable hemostasis. If possible, a pathogenetically based intervention is performed aimed at eliminating the main cause of bleeding: gastric resection (for ulcers, tumors) or vagotomy for duodenal ulcers. Resection to switch off is not applicable!
• Surgical tactics •• The more severe the patient’s condition, the less traumatic the operation should be. In extremely severe conditions, a bleeding ulcer of the stomach or duodenum on the front wall can be excised and stitched on the back wall. Recurrent bleeding is observed in 20–30% of cases •• If the patient’s condition allows (blood pressure more than 100 mm Hg), for bleeding ulcers of the stomach and duodenum, vagotomy can be performed with excision of the ulcer and pyloroplasty •• For Mallory-Weiss syndrome, perform gastrotomy and suturing of bleeding vessels of the crack (Beye's operation) •• For bleeding from varicose veins of the esophagus and cardial part of the stomach, suturing of veins with chain-shaped sutures from the side of the mucous membrane is indicated •• Bleeding tumors of the stomach - an indication for radical or palliative (in the presence of metastases) resection or gastrectomy.
• Postoperative management of patients is carried out taking into account the severity of blood loss, the volume of surgery and the presence of concomitant diseases •• Patients are in the intensive care unit or intensive care unit •• Bed rest for up to 4–5 days, taking into account the degree of anemia and the volume of surgery •• The volume of infusion therapy depends on the deficiency BCC (usually on the first day is 3000–4000 ml, followed by a decrease to 1.5–2 l by day 5). The number of blood transfusions depends on the degree of anemia. Plasma, protein, albumin 200-400 ml, rheopolyglucin 400 ml, pentoxifylline 5 ml, crystalloids (5% glucose solution, Ringer-Locke solution), vitamins C, B, menadione sodium bisulfite) are transfused daily. • Antiulcer therapy is continued. For ulcers associated with H. pylori, etiotropic therapy is prescribed (amoxicillin, metronidazole) and treatment is continued under the supervision of a gastroenterologist and after discharge from the hospital •• Deficiency of blood volume, central venous pressure, biochemical parameters of blood, urine serve as criteria for the volume and composition of infusion therapy •• Antibiotic therapy is necessary , because anemic patients are prone to infections •• The Meulengracht diet is prescribed to non-operated patients with stopped bleeding one day after admission. After the operation, diet 0 is prescribed from day 3, on days 4-5 - diet No. 1b and by the end of 2 weeks - diet No. 1 •• The gastric tube, after washing, is removed on days 2-3, provided that gastric motility has been restored. On days 2–3, a cleansing enema is performed, since the blood remaining in the intestines (decomposing and absorbing) causes intoxication.