Functions of the organ
The pancreas is responsible for the synthesis of enzymes necessary for the normal functioning of digestive processes. They ensure the breakdown of proteins, fats and carbohydrates, and also contribute to the formation of a food bolus, which then enters the intestines. If there is a malfunction in the pancreas, all these processes are disrupted and serious health problems arise.
But in addition to digestive enzymes, the pancreas produces hormones, the main of which is insulin, which controls blood glucose levels. Its deficiency causes the development of diabetes mellitus, which, unfortunately, cannot be treated and requires the patient to constantly take medications, which also negatively affects the overall functioning of the body. And the patient cannot do without them, since a sharp jump in blood sugar can lead to sudden death.
There are a large number of factors that can lead to disruption of the pancreas. But most often the culprit of problems with these organs is the person himself, who eats unhealthy foods and alcoholic drinks. As a result, pancreatitis develops, characterized by inflammation of the pancreatic parenchyma and disruption of its functionality.
Since this organ is so important to the human body, is the pancreas removed? People with pancreatitis are mainly treated with medication. But this disease is a provocateur of more serious pathologies, such as the formation of malignant tumors on the surface of the gland, cysts, stones in the ducts, or the development of necrosis. In all these cases, the only correct method of treatment is surgery. However, doctors are in no hurry to resort to it, since the pancreas is an important organ in the human body and it is almost impossible to predict the consequences that may arise after its removal.
Even if partial resection of the gland is planned during the operation, this does not provide a 100% guarantee that inflammation will not recur. If we are talking about pancreatic cancer, then in this case the chances of a complete cure after surgery are only 20%, especially if the disease has affected nearby organs.
Medication support after surgery
People who have had their pancreas surgically removed need complex enzyme and insulin therapy. The main goal of enzyme therapy is to help the body produce enzymes to digest food. For this purpose, drugs are prescribed that contain pancreatin. For example, Mikrasim, Vestal, Creon. These drugs improve digestion, eliminate nausea and stomach discomfort and have virtually no side effects.
Insulin injections are also required for patients who have had their pancreas removed. Today there are several types of insulin, which are very similar to the hormone that is produced in the human body.
Indications for removal
The pancreas can be removed if the following diseases develop:
- acute pancreatitis complicated by necrosis;
- oncology;
- cysts;
- deposition of stones in the gland ducts;
- pancreatic necrosis;
- abscess;
- hemorrhages inside the cyst.
There are many indications for pancreatic removal, but most often the operation is performed for oncology and necrosis
Diet after pancreatectomy
After discharge, a patient who has had the pancreas or parts thereof removed is prescribed a special diet - table No. 5. This diet provides for a strict diet, the key points of which are:
- complete rejection of salty, fried, spicy and fatty foods;
- split meals in small portions (at least 5–6 times a day);
- inclusion of healthy products in the menu;
- drink plenty of water (1.5–2 liters of water per day);
- complete abstinence from alcohol.
The list of prohibited products includes:
- sweets, pastries, bread;
- spices and seasonings;
- some vegetables and fruits (radish, onions, cabbage, spinach, sour apples, garlic);
- canned food, sausage;
- fast food and convenience foods;
- fatty meats and fish;
- coffee and carbonated drinks;
- smoked meats and pickles.
You can live a long time without a pancreas if you follow a diet
Removal method
For partial or complete resection of the pancreas, a method such as pancreatectomy is used. If it is necessary to completely remove an organ, the operation is performed laparotomically, that is, access to the affected gland is gained through an incision in the abdominal cavity. After all the measures have been taken, the incision site is stitched or secured with staples.
Sometimes during such an operation, drainage tubes are installed in the abdominal cavity, which allow the fluid that accumulates in the area of the surgeon to be removed. In some cases, doctors also place drainage tubes in the intestines. As a rule, this is done only when the need for probed nutrition arises.
If the gland is not completely removed (only part of it), then in this case pancreatectomy can be carried out using the laparoscopic method - access to the organ is gained through punctures in the abdominal cavity by introducing into the abdominal cavity a special device equipped with a camera, which allows you to monitor all the actions taking place on a computer monitor. This operation is less traumatic and requires a shorter rehabilitation period. But, unfortunately, not in all cases it is possible to use this method of surgical intervention.
During the operation, not only the pancreas can be removed, but also other organs located near it, for example:
- gallbladder;
- spleen;
- upper part of the stomach.
During and after the operation, there is a high probability of serious complications occurring. In this case, it speaks not only about the possibility of developing inflammation or infection, but also about the further work of the entire body. Indeed, quite recently, operations during which the gland was completely removed were not carried out in medical practice, since it was believed that without this organ people could not live even one year.
The final stage of pancreatectomy
However, today the situation has completely changed, and the prognosis after such operations is favorable, but only if all the doctor’s instructions are followed. How the body will recover during the rehabilitation period and how long a person can live after this depends on several factors:
- the patient’s weight (people with excess body weight have a harder time recovering from surgery and live less);
- age of the patient;
- nutrition;
- a person has bad habits;
- state of the cardiovascular system;
- the patient has other health problems.
Is it possible for a person to live without a pancreas? Of course! But it should be understood that the more negative factors affect the body, the greater the likelihood that complications will arise after surgery, which may lead to a reduction in life expectancy. After removal of the pancreas, you can live long and happily only if you lead a healthy lifestyle and follow all the doctor’s recommendations.
Technique of the operation
Removal of the pancreas, as already mentioned, is indicated for such pathological changes as the development of benign or malignant neoplasms, as well as the appearance of cysts. Surgical intervention on this organ can also be used in the case when it is detected when the development of a strong inflammatory process in it is diagnosed, or the presence of parasitic larvae is detected. When performing surgery on this organ, general anesthesia and muscle relaxants (drugs that relieve spasms of smooth muscles) are used for pain relief. The pancreas can be removed using the following technique:
To treat gastrointestinal diseases, people successfully use Galina Savinova’s method. Read more >>>
- Direct opening of the pancreas.
- Freeing the omental bursa from the blood accumulated in it.
- Stitching of gaps existing on the surface of the organ.
- Opening and dressing hematomas.
- In case of significant ruptures of the pancreas, separate sutures are applied, as well as parallel suturing of the pancreatic duct.
- The last stage of the operation is drainage of the omental bursa.
If the pancreas is significantly damaged and the patient has all the signs of severe internal bleeding, surgery should be an emergency, and in all other situations, planned surgical treatment is prescribed.
Patients often ask their attending physicians which surgical interventions are most often used in clinical practice for resection. This, according to experts, depends on what exactly will be removed, the entire organ, or a certain part of it. In the case when removal of the head of the pancreas is required, an operation called pancreaticoduodenectomy is performed, and if the body of the pancreas or its tail is damaged, a distal resection is performed. Dead tissue is removed by necrectomy, and if cysts or abscesses are detected, drainage is performed.
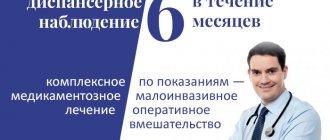
Rehabilitation period
After removal of the pancreas, a person’s life changes dramatically. Even if only the tail of the organ or another part of it was removed, and the operation itself went without complications, the patient will need a lot of time and effort to fully recover.
If the patient follows all the doctor’s recommendations, the rehabilitation period in 90% of cases proceeds without serious complications
If the pancreas is removed, the patient will have to follow a strict diet, take special medications and use insulin injections to ensure control of blood sugar levels.
Many patients complain for a long time that they have pain in the operated area, and the pain is severe. And to minimize them, doctors usually prescribe painkillers as additional therapy. Full recovery of the body after pancreatic surgery takes about 10–12 months.
What are the reasons for organ removal?
Why do doctors offer patients surgery and who is at risk? As a rule, for those who suffer from pancreatitis, doctors prescribe enzymes to maintain a normal state, and also recommend a strict diet. But it also happens that the disease progresses, the pancreas begins to literally digest itself. As a result, irreversible necrosis (death) of the gland tissue occurs. Such a process can affect the functioning of neighboring organs and change the composition of the blood for the worse. To avoid relapse, the surgeon will suggest partially or completely removing the organ.
The second reason is stones in the ducts of the organ, and the third is a cancerous tumor. In these two cases, surgery is almost inevitable.
Possible consequences in the postoperative period
The consequences of removing the pancreas can vary. Any surgical intervention has a high risk of developing inflammatory or infectious processes in the tissues of the body in the postoperative period. And to avoid them, the doctor prescribes a course of antibiotics before and after the operation. If the patient takes them strictly according to the prescribed regimen, the risks of such complications are reduced several times.
After removal of the gland, diabetes mellitus develops, because after the operation there is an acute lack of insulin in the body, which is why the person is forced to constantly take insulin injections. If you skip them or use them incorrectly, this is also fraught with various consequences, among which is hypo- and hyperglycemic coma.
In addition, even the removal of a small part of the pancreas disrupts its exocrine functions responsible for digestion. Therefore, the patient will also have to constantly take enzyme preparations (they are prescribed on an individual basis).
Drugs used as replacement therapy after removal of the pancreas
Features and consequences of pancreatic tail removal
Reasons for removing the tail of the pancreas:
- Mechanical damage to an organ
- Cyst in the tail
- Focal pancreatic necrosis,
- Complication of chronic pancreatitis,
- Pathologies,
- Suppuration of the tail of the pancreas,
- Cancerous swellings in the tail area that need to be removed.
If indicated, an incomplete distal pancreatotomy is performed. The operation is performed under general anesthesia. The surgeon opens the abdominal part, exposing the pancreas, and all connective tissues of the tail with the spleen and abdominal cavity are removed. If an abscess or tumor has leaked into the spleen, it also has to be removed.
The consequences are minimal:
- There is no risk of developing diabetes
- There are no prerequisites for the development of carbohydrate metabolism disorders,
- Minor digestive problems are possible.
The prognosis for tail removal worsens if the spleen is removed along with it. A person becomes less resistant to infectious diseases:
- Pneumonia,
- Malaria,
- Hepatitis A,
- Hernia,
- Suppuration of sutures,
- Meningitis.
Removal of stones from the pancreas: prognosis, features of the operation.
Stones in the pancreatic ducts are rare. But over the years, the number of patients with this problem is only growing. Not only stones in the pancreas can interfere with the outflow of digestive secretions, but also gallstones that are stuck in the common canal.
Medicine was unable to identify the exact cause of the pathology.
It is rational to perform surgery only when the size of the stone exceeds one centimeter; in other cases, treatment is carried out with medication or with ESWL.
To remove a stone from a gland or duct, the muscle tissue is cut at its location. Next, the stone is pushed into the intestine, from where it is excreted naturally.
In more than 85% of cases it has a favorable outcome.
Removal of a cyst on the pancreas: consequences, features.
In most cases, surgery is prescribed when a potentially dangerous false cyst of the pancreas is detected; it does not have its own walls and adheres to the gland.
If the false cyst grows rapidly, it is removed along with the affected gland tissue, and the remaining parts are stitched together.
Complications:
- Postoperative pancreatitis,
- Circulatory failure
- Bleeding.
Tumor removal
A pancreatic tumor can be described as a release of uncontrollably growing cells that form a tumor.
The malignant neoplasm is removed only before the size reaches 2 cm and it begins to release mestases. Benign tumors are always removed promptly.
In medicine, there are four ways to remove a tumor:
- Partial removal of the pancreas. It is prescribed only if it is localized in the tail area,
- Enucleation of the tumor. Recommended if you have a hormonal tumor that produces hormones,
- Pancreatoduodenal surgery. It is carried out when the tumor is located in the head of the gland. Along with the tumor, part of the duodenum is removed.
- Blockage of blood vessels - used in the presence of a benign neoplasm, which is located in the canal or blood vessels of the gland.
Consequences of the operation if part of the pancreas was removed:
- Digestive disorder
- Postoperative pancreatitis,
- Bleeding
How to gain weight after removal?
Those who had to say goodbye to this vital organ once and for all suffer not only from a lack of enzymes and diabetes, but also from sudden weight loss.
A person begins to lose weight because substances are poorly absorbed, and a specific diet that prohibits most high-calorie foods also contributes to this.
The diet allows you to eat low-fat protein cottage cheese, meat and fish. To get better you need to increase the quality and quantity of protein. Just eat more meat, fish, and sometimes you can eat bread made from wheat flour.
Why is the pancreas removed?
No matter how dangerous the procedure is, there are cases when the pancreas is no longer able to recover and can lead to death.
Causes:
- Cancer tumor,
- Serious damage to the pancreas,
- Pancreatic necosis.
The whole danger of the operation lies in the enzymes that can go beyond the organ and begin to destroy other tissues and organs.
The operation has the greatest danger for:
- People suffering from heart and lung diseases,
- Those who are accustomed to eating improperly,
- Smoking,
- People who are overweight
- Those who are over 40 years old.
Consequences and life after
After the operation, the patient’s life does not change for the better - he lost a vital organ and now he will have to artificially compensate for the lack of substances.
Complications:
- Diabetes,
- Digestive metabolic disorders
- Bleeding,
- Infections.
What the patient should do regularly:
- Follow a therapeutic diet for life
- Drink enzyme preparations (pancreatin, mezim),
- Give insulin injections
- Perform hygiene procedures in accordance with the doctor’s recommendations.
What operations are performed for chronic pancreatitis?
Some patients believe that with diabetes mellitus, along with the concomitant destabilization of the gland due to chronic pancreatitis, only surgery will help. But experts warn that with such a pancreatic condition, one can only hope for relief, and not for a complete recovery without the risk of relapse.
To help victims of the chronic form of such a dangerous disease, doctors have developed several surgical practices:
- drainage of ducts, which is necessary in case of pronounced problematic patency;
- resection with drainage of the cyst;
- resection of the head, which is characteristic of obstructive jaundice, duodenal stenosis;
- pancreatectomy for large-scale lesions.
The stones that are deposited in the ducts deserve special attention. They partially or completely block the passage of secretions, which provokes acute pain. In case of severe pain and the impossibility of reducing its manifestations with the help of pharmacological substances, there is no other option other than classical surgery.
This technique is called virsungotomy. This means cutting the duct to remove the stone, or draining above the level of obstruction.
Operative technique
After the doctor has referred you to a surgeon, you can begin to prepare for surgery. The method of removing the pancreas in surgery is called “pancreatectomy”.
To gain access to the dysfunctional organ, the surgeon must cut into the abdominal cavity. Then medical manipulations occur and the affected gland is removed from the body.
The incision is stitched with medical threads.
Interesting! In some cases, the surgeon may need drainage tubes during a pancreatectomy. They are used to remove fluid accumulated in the abdominal area. Sometimes intestinal drainage occurs.
There is also laparoscopy - a surgical method in which access to the organ is gained through 4 punctures in the abdominal area.
Typically, such manipulation occurs on the operating table if the patient needs to have the gallbladder removed.
In case of gland dysfunction, laparoscopy is performed only for the purpose of incomplete, but partial removal of the organ.
In this case, a special camera is inserted into the patient’s gastrointestinal tract through one of the punctures, thanks to which the surgeon receives an image.
Is it possible to live without a pancreas? Of course, because otherwise, pancreatectomy would never have been performed.
However, after such a surgical intervention, the risk of complications is extremely high.
An important rule: to reduce the likelihood of postoperative complications, you need to follow all the advice of your doctor. . This operation is characterized by a fairly long recovery period.
Most often, the patient encounters postoperative complications such as inflammation of the abdominal organs or their infection.
This operation is characterized by a fairly long recovery period. Most often, the patient encounters postoperative complications such as inflammation of the abdominal organs or their infection.
However, the development of medicine does not stand still. Today, the likelihood of complications occurring after pancreatectomy if patients comply with medical instructions is extremely low.
Factors that influence the duration of postoperative recovery:
- Compliance with dietary nutrition by patients.
- Patient's weight category. Overweight people recover more slowly.
- Bad habits.
- Age category of the patient.
- Pathologies of the functioning of internal organs.
- Stability of the heart muscle.
Important! You should not be afraid that, if you are left without a gland, you will not be able to live happily and long. On the contrary, your life will remain the same, however, to maintain health you will have to adhere to some rules regarding medication and diet.
What surgery is indicated for abscesses?
If a person has been confirmed to have an abscess, then sending him to the operating room cannot be delayed. Especially when the abscess was a direct consequence of limited necrosis after exposure to an infectious pathogen. Sometimes the provocateur of the deviation is a long-term period of suppuration of the pseudocyst.
People usually ask what can be done in such a serious situation, other than surgery, but without an autopsy with drainage, a person’s life is unlikely to be saved. Depending on the affected area, it will depend on which technology the gastroenterologist will prefer:
- open;
- laparoscopic;
- internal.
The first combination is based on laparotomy, which involves opening the abscess with drainage of its cavity until the area is completely cleared.
When a verdict is made in favor of laparoscopic drainage, a laparoscope is required, with the help of which the problem point is opened carefully. Next, the expert removes non-viable tissue and installs channels for proper drainage to function.
A difficult and at the same time productive technique is internal drainage, the difficulty of which lies in opening the abscess through intervention through the posterior wall of the stomach. For a successful outcome, laparotomy or laparoscopic access is used.
The result is presented in the form of the release of malicious content through an artificially created fistula. Over time, the cyst becomes obliterated, and the fistula opening closes.