What is mushy stool?
In every healthy person, feces are formed in the large intestine under certain conditions. With normal functioning of the digestive system, the stool is soft but formed. However, if for some reason a malfunction occurs, the feces acquire a characteristic mushy consistency. If such a symptom is the result of an error in diet, then you should not worry, as this is considered a variant of the norm. However, with daily and frequent bowel movements that result in mushy stools, you should think about a more serious reason.
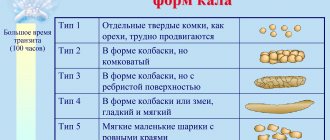
The Bristal stool scale shows normal and pathological options
Varieties: for a long time, frequent, with mucus, in the morning and others
Depending on additional conditions, the following types of this symptom can be distinguished:
- Pasty stools for a long time and accompanied by flatulence. Can appear at any time. Most often accompanied by various gastrointestinal pathologies.
- Frequent. In this case, emptying can occur more than 3 times a day.
- Appears in the morning. May be accompanied by nausea and other digestive disorders.
- With mucus. Mucous streaks may be present in sufficient quantities in the stool.
- Thick with particles of undigested food. Pasty stools may be patchy and have a porous structure. Quite often contains some food fragments.
Types on the Bristol scale
The classification of the main types of feces is presented on a specially developed Bristol scale.
The table shows pictures of types of feces and their descriptions.
It allows the patient to easily and without embarrassment formulate and characterize his own bowel movements, naming the appropriate type to the doctor:
- 1 and 2 are considered signs of constipation, feces do not come out of the intestines for several days, and are hard as a rock. They can cause injury to the anus, hemorrhoids, and intoxication.
- With type 3, defecation is also difficult, but the stool is of a softer consistency. To empty the intestines, you have to make several intense attempts, which can cause cracks. Characteristic of irritable bowel syndrome.
- Types 4 and 5 are considered normal. With the latter, defecation is possible several times a day.
- Type 6 indicates a stool that is not formed. It is regarded as a condition close to diarrhea.
- Type 7 includes loose stools. Stool with the consistency of water is considered a pathological phenomenon that needs treatment.
Causes and provoking factors in adults and children
The main reasons why mushy stool may occur:
- Errors in diet. When consuming large amounts of plant foods, some changes in the structure of stool may occur.
- Gastroduodenitis. When the duodenum and the pyloric zone of the stomach become inflamed, digestion becomes incomplete, as a result of which mushy stool can form.
- Taking medications. Changes in the structure of stool can occur when treated with certain medications. These include Enterol, broad-spectrum antibiotics, glucocorticoids, and choleretic drugs.
- Pancreatitis. During inflammatory processes in the pancreas, an insufficient amount of enzymes is often released for proper digestion of food. As a result, mushy stool is formed.
- Cholecystitis. Inflammation of the gallbladder associated with stagnation of secretions can lead to a similar symptom.
- Decreased appetite. A meager intake of food into the body provokes the formation of mushy stools.
- Inflammatory processes in the intestines. Pathologies of this nature lead to underformation of feces. As a result, absorption in the small intestine deteriorates, and there are not enough enzymes for digestion.
- Dysbacteriosis. An insufficient amount of beneficial microflora gives rise to similar symptoms.
Amount of feces
Normally, an adult excretes approximately 100-250 grams of feces per day.
Reasons for decreased stool output:
- constipation (if feces remain in the large intestine for a long time, maximum absorption of water occurs, resulting in a decrease in the volume of feces);
- the diet is dominated by foods that are easily digestible;
- reducing the amount of food eaten.
Reasons for increased stool output:
- predominance of plant foods in the diet;
- disruption of digestive processes in the small intestine (enteritis, malabsorption, etc.);
- decreased pancreatic function;
- impaired absorption in the intestinal mucosa;
- decreased flow of bile into the intestines (cholecystitis, cholelithiasis).
Diagnostic measures
A timely approach to diagnosis is extremely important to determine the cause and eliminate symptoms. Basic research methods:
- Questioning the patient. It is carried out in order to eliminate errors in the diet. The doctor asks the patient about medications taken that could cause changes in stool.
- FGDS. Endoscopic examination of the stomach and duodenum is carried out by probing. In this case, a thin tube with an optical device at the end is inserted into the esophagus and from there moves towards the stomach and duodenum. In this case, areas of inflammation and other changes in the mucous membrane are determined.
- Colonoscopy. Similar to the previous method, only in this case the probe is inserted through the rectum. In this way, pathologies of the large and small intestines are diagnosed.
- Ultrasound. Ultrasound examination of the abdominal cavity can detect diseases of the pancreas and gall bladder.
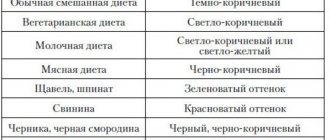
Stool color
Normal color can vary from light brown to dark brown. In pathology, the following may be noted:
1. Light-colored feces with a pale tint (white, gray):
- may indicate that the person ate a large amount of potatoes and rice the day before;
- after X-ray examination using barium sulfate;
- after taking medications that include supplements such as calcium and antacids;
- pancreatitis;
- cholecystitis;
- hepatitis;
- stones in the gall bladder and bile ducts;
- cancer, cirrhosis of the liver.
2. Red feces:
- eating large amounts of beets, red gelatin, tomatoes, fruit juices..;
- disruptions in the functioning of the large intestine;
- the development of foci of intestinal inflammation, the presence of intestinal infection, as well as parasitic lesions (diarrhea, cramps, nausea, vomiting are also characteristic).
Drug treatment
If the cause of mushy stool is gastroduodenitis, then the doctor most often prescribes drugs that regulate gastrointestinal motility and drugs that help restore the mucous membrane of the stomach and duodenum. Such medications include Omez, Nolpaza, Emanera. A drug that affects motor function, Trimedat is able to influence both too fast and, conversely, slow peristalsis, regulating the movement of the food bolus.
For pancreatitis, medications are prescribed that can compensate for enzyme deficiency. These include Mezim, Pancreatin and Creon. Thanks to them, food is better digested and the stool is slightly firmer. If acalculous cholecystitis is present, then a diet is indicated. Prescribing choleretic drugs during exacerbation of symptoms can only worsen the course of the pathology.
For inflammatory bowel diseases, drugs that regulate the functioning of this organ are indicated. Most often, the doctor prescribes Pepsan-R. This drug relieves inflammation and reduces excess gas formation, as well as Kolofort, which regulates intestinal function.
When dysbiosis is present, the best treatment is a prebiotic containing beneficial bacteria. These products include: Linex, Hilak Forte and others. They promote the proliferation of beneficial microflora in the intestines.
Drug treatment - photo gallery
Nolpaza reduces the secretion of gastric juice
Trimedat regulates motor skills
Mezim compensates for the lack of enzymes
Pepsan-R relieves inflammation in the intestines
Linex helps normalize beneficial microflora
Stool consistency
Normally, it has a soft consistency and a cylindrical shape. In pathology, the following types of feces can be noted:
1. Dense feces (sheep) – the cause of such feces can be:
- dysbacteriosis;
- staphylococcus;
- peptic ulcer;
- irritation of the walls of the colon;
- colitis;
- poor circulation in the intestinal walls;
- syndrome of insufficiency of motor and reflex function of the gastrointestinal tract;
- nervous system disorder, stress;
- insufficient fluid intake;
- recovery period after surgery;
- sedentary lifestyle.
If you experience similar bowel movements, you need to consult a specialist, since if you continue to have bowel movements of this nature for a long time, your well-being may deteriorate significantly. Headaches and irritability may appear, intoxication of the body begins, and immunity decreases. Sheep feces can cause fissures in the anal canal, can provoke rectal prolapse, and cause the formation of hemorrhoids. Regular constipation requires mandatory consultation with a specialist.
2. Pasty stool.
There can be many reasons for mushy stool. If you have similar stools and also notice an increase in the number of bowel movements (more than 3 times a day), contact a specialist to establish a diagnosis.
Pasty yellow stools can be caused by infections, inflammatory processes of the intestinal mucosa, disturbances in the functioning of the stomach (indigestibility of food), or rotavirus infection. Pasty stools with mucus - may appear against the background of a common cold, after eating mucus-like foods, fermented milk mixtures, fruits, berry porridges. Often, with a severe runny nose, mucous secretions enter the esophagus, then into the intestines and can be visualized in the stool. For an infection that is bacterial in nature.
Diet food
Diet for mushy stools plays a decisive role. Sometimes, by changing your diet, you can quickly and permanently eliminate the problem. First of all, it is necessary to reduce the amount of plant food consumed, which accelerates peristalsis and forms liquid stool. It is necessary to include in the diet:
- bread;
- pasta;
- boiled rice;
- buckwheat;
- bananas;
- cookie;
- potato;
- persimmon.
Diet food - photo gallery
Bread anchors the chair
Pasta contains essential carbohydrates
Rice has a beneficial effect on the digestive tract
Buckwheat regulates intestinal function
Bananas contain a large amount of starch
It is better to cook cookies yourself or buy them without additives
Potatoes have a beneficial effect on the gastrointestinal tract
Persimmon has an astringent effect
Stool smell
Normally, stool has an unpleasant and not pungent odor.
- A pungent odor is characteristic of meat foods that predominate in the diet.
- Rotten smell - due to poor digestion of food (undigested food can be food for bacteria, it can simply rot in the intestines).
- Sour – may indicate the predominance of dairy products in the diet. Also noted with fermentative dyspepsia, after drinking fermented drinks (for example, kvass).
- Foul - with pancreatitis, cholecystitis, hypersecretion of the large intestine, with the proliferation of bacteria.
- Putrefactive – putrefactive dyspepsia, digestive disorders in the stomach, colitis, constipation.
- The smell of rancid oil is a consequence of bacterial decomposition of fats in the intestines.
- Weak odor - observed with constipation and accelerated evacuation from the small intestine.
Feces should sink gently to the bottom of the toilet. If stool splashes into the toilet water, this indicates insufficient dietary fiber. If feces float on the surface of the water, this may be a consequence of eating a large amount of fiber, high levels of gases in the feces, or a large amount of undigested fat. Poor flushing from the toilet walls may indicate pancreatitis.
Folk remedies
Traditional methods of treatment can be used as an auxiliary way to eliminate this symptom. To do this, use herbs that affect the functioning of the intestines. The most effective recipes:
- A decoction based on chamomile and oak bark. This remedy not only regulates the intestines, but also strengthens the stool. It will take 1 tsp. listed ingredients that need to be placed in a saucepan and pour 500 ml of boiling water and cook for 15 minutes. Then let stand for another 2 hours and strain. Take a quarter glass 2 times a day 30 minutes before meals for a week.
- Mint tea. Additionally you will need St. John's wort. It is necessary to mix both herbs and 1 tbsp. l. pour 400 ml of boiling water over the resulting mixture. Let stand for 25 minutes and then filter, taking 2-3 times a day a quarter of an hour before meals for 10 days.
- Chicory decoction. You will need 2-3 sprigs, which must be poured with 350 ml of boiling water and cooked over low heat for 10 minutes. After this, drain the liquid and divide it into 3 doses. The product should be taken 15–20 minutes before meals for 5 days.
Folk remedies - photo gallery
Chamomile relieves inflammation in the gastrointestinal tract
Oak bark has a strengthening effect
Mint regulates the functioning of the gastrointestinal tract
St. John's wort has a beneficial effect on the intestines
Chicory helps with digestive disorders
Treatment prognosis and consequences
As a rule, in the presence of pasty stools that are not burdened by additional symptoms, the prognosis is good. With timely diagnosis and treatment, recovery occurs fairly quickly. One of the most dangerous consequences is severe pathologies of the pancreas, in which self-digestion of the organ can occur and the production of enzymes will completely stop. In addition, advanced gastroduodenitis and liver diseases are fraught with the appearance of ulcerative lesions.
With constant mushy stool, a large amount of fluid is lost, which can ultimately lead to dehydration. This symptom cannot be ignored.