Polyps in the large intestine are benign neoplasms formed from glandular epithelial cells. Normally, tissues from this type of cells line the inside of the intestine, but under the influence of certain factors they begin to grow uncontrollably, forming single or multiple mushroom-shaped, spherical or branched outgrowths directed into the intestinal lumen. In the international classification of diseases ICD-10, colon polyps are designated by code K63.5. (colon polyps).
Most often, the pathology is diagnosed in men and women of the older age category. The greatest surge in incidence is observed after overcoming the 60-year mark. In childhood, polyps are found more often in boys aged 3 to 6 years (in 80% of cases), and most often neoplasms are localized in the distal intestine.
The main danger of polyps in the large intestine is the high risk of malignancy (degeneration of a benign neoplasm into a malignant one). That is why, regardless of what polyps (type, shape and size) are detected, they are considered precancerous neoplasms with varying degrees of malignancy.
Types and sizes of colon polyps
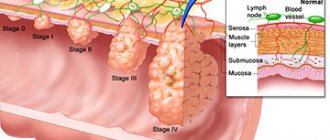
In medicine, a branched classification of polyps of the large intestine has been formulated depending on the cellular structure, appearance, nature and number of tumors. The size of the polyps also plays a role in diagnosis, since this parameter is directly related to the risk of intestinal cancer.
Polyps are divided into 4 types (forms) depending on their structure:
- Adenomatous is the most common and dangerous form of polyps, which can differ in appearance. There are tubular (tubular), tubular-villous and villous. The neoplasms are penetrated by many tiny vessels and often bleed. Regardless of appearance, they have a high level of malignancy (malignancy). It is diagnosed mainly in older people.
- Hyperplastic - a small glandular polyp, slightly rising above the surface of the intestinal mucosa, has a color natural to the surrounding epithelium. It is quite rare to transform into a malignant tumor. Often diagnosed in patients over 40 years of age.
- Hamartomatous - white-pink neoplasms that consist of several types of cells that develop disproportionately. Rarely reaches large sizes, as they grow evenly and very slowly. Such a neoplasm often bleeds and has a low risk of malignancy.
- Inflammatory - a glandular polyp that forms against the background of an acute inflammatory process in the intestine.
Based on the number of neoplasms in the intestine, single, multiple and diffuse (hundreds of rapidly growing and spreading neoplasms) polyps of the large intestine are distinguished. Diffuse and multiple polyps have the greatest tendency to transform into cancerous tumors.
Good to know! Affects the rate of malignancy and the size of polyps. Thus, small formations with a diameter of up to 1 cm have a degree of malignancy from 3 to 9%, while large polyps with a diameter of more than 3 cm transform into a cancerous tumor in 30% of cases.
Treatment of pathology
Ignoring signs of a problematic neoplasm in the colon is dangerous. To prevent the development of oncology, therapeutic measures and removal of the growth are necessary. When determining health measures, one must proceed from the signs of the disease.
Operation
Surgery today is considered the most effective and gentle way to get rid of multiple polyposis of the ascending colon. The operation is performed using colonoscopy, which involves influencing polyps with a high-frequency current to remove them.
The surgical procedure is as follows:
- To avoid damage to the intestinal wall, the leg or base of the polyp is compressed with special medical clamps. In this case, the doctor must make sure that the intestinal mucosa, despite the neoplasms, remains mobile.
- Performing perforation. Small polyps are cut off in one step. Removal of large growths is carried out by cutting off parts of the growth.
- The removed polyp is sent for histological examination.
If the polyposis is total, then coagulation is chosen as a method of getting rid of it. Surgery for single growths is performed through colotomy and resection. In case of extensive damage, surgical procedures are carried out in 2 or 3 stages with an interval of 2-3 days.
If after surgery the polyps appear again, the patient undergoes curettage of the problematic part of the intestine with complete removal of the mucous layer.
Drug therapy
Drug treatment is an additional measure to surgical removal of polyps. It allows you to prevent possible complications: the occurrence of an inflammatory process, tissue infection. In addition, taking special medications improves the functioning of the immune system.
Some patients have contraindications to surgery. So, for example, endoscopy is not recommended if polyps are bleeding or if the growths are located not on thin stalks, but on thick bases. In this case, doctors prescribe potent drugs aimed at destroying the polyp cells.
The last stage of treatment is following a gentle diet and systematically visiting a doctor as part of a medical check-up to monitor the condition of the intestines. Women experiencing colonic polyposis are prescribed a course of hormonal pills for 6-12 months.
Polyposis of the transverse colon is an extremely unpleasant pathology. Since the risk of its development increases with age, people over 50 years of age are recommended to periodically undergo examinations of the digestive tract in order to detect deviations from the norm and stop the pathogenic process in the early stages.
Causes of colon polyps
Doctors cannot name the exact reasons for the formation of benign tumors in the large intestine. Previously, it was believed that their formation occurs under the influence of bad habits - alcoholism, smoking. However, a considerable number of patients diagnosed with colon polyposis follow the principles of a healthy lifestyle, which raised some doubts about the validity of such judgments.
Recent studies have found that bad habits as such are not the main risk factor. They play the role of a trigger, but in most cases the disease occurs in those whose close relatives suffered or suffer from polyps in various parts of the gastrointestinal tract. In addition, colon polyps threaten people with acute and chronic diseases of the digestive system, excess weight, and chronic stool disorders due to non-compliance with norms and diet.
According to statistics, approximately 50% of men and women over 60 years old have polyps in the large intestine. This indicates that age-related changes are the most common cause of the disease.
Important! Certain types of polyps are formed due to inflammation of the intestinal mucosa.
Causes of pathology
The etiology of the disease is still not fully understood. This explains the poor development of therapeutic measures and methods for preventing the development of the disease. Provoking factors are considered:
- chronic problems in the gastrointestinal tract;
- frequent constipation;
- rapid aging of the mucous membrane;
- history of gastritis;
- sedentary lifestyle, sedentary work;
- tendency to drink alcohol;
- smoking;
- unhealthy diet, in which a person eats a lot of meat and little fiber;
- excess body weight, tendency to overeat;
- endocrine pathologies and disrupted hormonal levels;
- genetic predisposition to the occurrence of lymphangiomas.
Symptoms and signs of colon polyps
At the initial stages of development, polyps do not appear in any way, and therefore they are discovered by chance when examining the intestines for other diseases. Clinical manifestations of polyposis appear if there are several benign formations or they are more than 1 cm in diameter. In this case, the symptoms can be very diverse and nonspecific. Most often, patients complain of the following phenomena:
- unstable stool with frequent alternation of diarrhea and constipation, sometimes within one day;
- irritation of the mucous membrane of the anus and the skin of the perianal area, which occurs against the background of abundant mucus secretion from the rectum (a symptom characteristic of polyps located in the lower part of the colon);
- scant rectal bleeding that is not accompanied by acute pain in the anus (a symptom characteristic of villous polyps located in the lower part of the large intestine);
If you have these problems, you should urgently contact a gastroenterologist or coloproctologist, since they are the ones who diagnose and treat the disease.
Clinical manifestations and diagnosis
To make a correct diagnosis, a doctor does not have enough examination and laboratory and instrumental methods. According to modern concepts, any neoplasms should be examined by histologists. This makes it possible not only to find out the tissue identity of the polyp, but also the prognosis for the person.
Adenomatous polyps are more prone to malignancy than others, so when they appear along with other histological types, the need for surgical intervention arises.
Polyposis is almost always completely asymptomatic. A person may not even be aware of such a problem, so polyps are often discovered by chance during an examination for another gastrointestinal pathology. However, the simultaneous presence of several diseases should not be ruled out.
When diagnosing a disease, the doctor takes into account the following aspects:
- Anamnesis data. It is possible to establish causally significant factors in the development of pathology, including chronic gastrointestinal diseases, alcohol abuse, dietary errors, and family history;
- Physical examination. Polyps of the rectum and anus are usually detected. The general condition of the patient is also taken into account, which may be aggravated by symptoms of complications, for example, pallor of the skin and mucous membranes with posthemorrhagic anemia;
- Digital examination of the anus and rectum. The tone of the anal sphincters, pain, and possible defects of the mucous membrane are taken into account. This is how various volumetric neoplasms of this localization are found;
- Sigmoidoscopy or colonoscopy. With an endoscopic examination, it is possible not only to visualize polyps, but to perform a biopsy (sampling of material for further study by histologists) or even remove them on the spot, if the situation allows.
If there are obstacles to endoscopic examination methods, irrigography is performed as an alternative or the patient is referred for ultrasound/CT/MRI.
Of course, patients are prescribed various diagnostic measures, which will depend on the characteristics of their body, age and financial capabilities.
As the pathological process progresses, the patient develops the following symptoms:
- Abnormal bowel movements such as constipation or diarrhea;
- After a bowel movement, a feeling of dissatisfaction/incompleteness remains;
- In the stool you can visually notice the presence of impurities such as streaks of blood or mucus. It happens that only with a digital examination the doctor detects signs of intestinal bleeding;
- Abdominal pain, most often localized in the lower parts.
Patients with familial forms of polyposis also tend to have various extraintestinal pathologies, for which they usually first visit a medical institution.
Diagnostics
Very often, the symptomatic manifestations of colon polyps are similar to other diseases of the gastrointestinal tract. When making a diagnosis, differential diagnosis is used, during which the doctor excludes other pathologies.
First of all, the doctor collects anamnesis and conducts a survey of the patient, during which he establishes the characteristics of the patient’s symptoms, diet and gastronomic habits.
Important! To make a correct diagnosis, a specialist will need information about previous diseases and diseases of the colon that immediate relatives have suffered.
Next, the coloproctologist conducts a digital examination of the rectum, during which it is possible to determine the presence of polyps in the area of the rectum remote from the anus, their size, method of attachment to the mucous membrane (pedunculated or wide base), shape, consistency and degree of displacement.
In addition to the listed studies, patients with suspected colon polyposis will have to undergo a number of laboratory tests:
- general blood test (in some situations, low hemoglobin levels indicate polyposis);
- stool occult blood test (often replaced by the Colon-View occult blood screening test).
To establish the exact location, size, number and shape of polyps in the colon, instrumental diagnostic methods are used:
- sigmoidoscopy - a visual examination using endoscopic equipment equipped with a fiber optic system, a light source and forceps for taking a biopsy;
- colonoscopy is a method of visual examination of the intestines using a flexible probe (colonoscope) equipped with a camera, a lighting device, an air injection tube and forceps for taking a biopsy;
- irrigoscopy - x-ray examination of the colon using a contrast agent;
- magnetic resonance or computed tomography.
After colonoscopy and sigmoidoscopy, a study of biological materials (parts of the mucous membrane of the colon or the polyp itself) is carried out to determine their cellular structure and the risk of malignancy.
How does an intestinal polyp appear?
Cancer in the intestine begins, as a rule, not out of nowhere, but against the background of a benign tumor, popularly called a “polyp.” All benign tumors are divided according to their structure into:
- adenomatous polyps
- and adenomas: tubular, villous and tubular-villous.
Adenomatous polyps are the most common, accounting for almost a third of all tumors.
The risk of cancer due to a polyp is about 15%, maybe more, so all polyps are removed. A quarter of all existing villous adenomas can become cancer, so they are considered the most “harmful”. Of course, not all adenomas become malignant, but the chance of cancer cells appearing in one or another part of the polyp increases with the polyp, its size and age.
A polyp is a tumor that is benign for the time being. They should be distinguished from hyperplastic polyps, which are not polyps at all, but the result of inflammation of the mucous membrane. This name has been preserved since the time when in medicine everything was determined by eye without histological examination, so they were mistaken for true tumors.
Real polyps consist of connective tissue and irregular and deformed glands of the mucous membrane; they are not just a growth, like a hypertrophic polyp, but a complex tumor. And not just a benign tumor, but a precancer that can become a real cancer.
It is not known why polyps occur in the colon; it is assumed that diet, life and genetic factors are to blame. The intestinal mucosa consists of villi and depressions - crypts; for each villi there are several crypts. At the bottom of each crypt, intensive division of stem cells occurs, replenishing the lost cells of the villi and the crypts themselves. A polyp on the villus appears when the balance between proliferation—replenishment of cells—and their differentiation—specialization of newborn cells by function—is disturbed.
The size and shape of polyps vary even in one intestine; they can look like warty protrusions, or they can be a ball on a thin stalk or a fungus sitting on a fold. They can cluster in one place, forming a cluster, or they can be located a meter from each other. It is believed that adenomatous polyps accumulate additional mutations in genes that should normally suppress emerging cancer cells, or in genes responsible for regulating proliferation, and the polyp becomes malignant - becomes malignant, and this is early colon cancer.
Treatment methods for colon polyps
Conservative methods of therapy for colon polyps are not used, as they are not effective. Doctors call surgical removal of tumors the only way to eliminate them. Depending on which polyps are detected during diagnosis, the following methods are used:
Surgical colonoscopy is used to remove single and multiple polyps. It is performed using a colonoscope equipped with a loop electrode. During the procedure, a loop is placed on the stalk of the polyp and tightened until it fits as tightly as possible. Then high-frequency currents are passed through the loop, as a result of which the head is cut off and the leg is charred. The resulting wound is cauterized.
If the polyp is located on the mucous membrane of the colon on a broad basis, an endoscopic operation is performed, the so-called endoscopic resection of the mucosa, with coagulation of the base of the wound. The operation is performed using a special electric knife, which is used to resect a section of the mucous membrane along with the polyp. Surgeries for resection of colon polyps can be quite lengthy, the duration depends on the size of the polyp, but they are minimally traumatic and do not require long-term hospitalization. Typically, the hospitalization period is from 1 to 3 days.
Radio wave and laser coagulation. Used to remove one or more polyps. The tumor is exposed to a narrow beam, causing its tissue to die. To prevent bleeding, coagulation of blood vessels is performed. The procedure, like the previous one, is low-traumatic, does not cause side effects and does not require long-term rehabilitation and recovery.
Abdominal surgery. For diffuse familial polyposis, a subtotal or total colectomy is performed, i.e. resection of the colon with the affected area, subsequently an anastomosis is formed.
Immediately after surgery, a gentle diet with limited salt, sour, and spicy foods is recommended. Do not eat too hot or cold foods, mushrooms, fatty meat and fish, fried and smoked foods, alcohol and strong coffee. You will have to stick to the diet for at least 4 weeks.
After removal of types of polyps prone to malignancy (villous, multiple and large), a year after treatment, the patient is shown an endoscopic examination of the intestine to monitor the condition of the mucous membrane. Medical supervision is recommended for two years.
If there are no symptoms of polyposis, colonoscopy is subsequently performed every three years.
Features and nature of the pathology
A hyperplastic polyp is an initially benign neoplasm characterized by the growth of mucous membrane into the organ cavity. The size of the tumor can reach 3 cm. In appearance, the polyp has a clear structure: body, base and stalk. Sometimes the stem may be absent; such growths are called flat. The base or stroma of the polyp has an altered mucosa with impaired regeneration of cellular structures.
Polyps never appear on healthy tissue. The formation is based on a violation of the integrity of the mucous membranes under the influence of various factors.
Hyperplastic polyps are diagnosed in the vast majority of all clinical cases. The main risks as the polyp grows are associated with malignancy of tumor cells and transformation of the growth into an oncological neoplasm.
Classification and types
The modern classification of pathological foci is determined by two main criteria: quantity and forms of changes in the mucous membranes of the colon.
By number
There are three main directions in the growth of polypous foci:
- Limited or localized (1-2 polyps in the rectal lumen);
- Multiple (2 or more pathological growths);
- Diffuse familial polyposis (there are up to hundreds of pathological units).
With multiple focal growths, the development of rectal polyposis occurs. With diffuse polyposis, growths cover almost the entire rectal cavity with neoplasms of different sizes from 0.4 mm to 1-2 cm. Find out what a rectal polyp looks like here.
Diffuse polyposis is almost always inherited; it can be diagnosed in infants with autoimmune diseases if parents or close relatives have a history of multiple familial polyps.
According to the form of the neoplasm
There are 4 main forms of hyperplastic polypous foci:
- Adenomatoses or adenomatous polyps (most often degenerate into malignant ones; clinicians characterize adenomatosis as a precancerous condition). Adenomatous tumors are classified into the following subtypes: Tubular type (foci of a pinkish tint with a dense structure and a smoothed surface);
- Villous (the growth appears as branch-like growths resembling small villi, the body and base are filled with multiple vascular weaves);
- Tubular-villous (mixed type, based on changes in the hypertrophied mucosa of the tubular and villous type).
Hyperplastic forms of polyps are characterized by elongation of the tubes of epithelial structures with an increased tendency to cystic transformation.
Note ! According to the results of long-term observations, all hyperplastic neoplasms grow and change. When transformed into adenomatosis, such growths are most prone to cell malignancy.
Hyperplastic polyps of the sigmoid colon
The sigmoid colon is a large distal section of the intestine, up to 70 cm long. The normal lumen diameter reaches 4 cm. The main function is the absorption and distribution of nutrients.
It is in this segment that most of the liquid and vitamins are absorbed. This is where the formation of primary feces begins. With the formation of hyperplastic polyps, the diameter of the sigmoid colon can expand, and the functionality of the organ is often impaired.
Polypous formations of the sigmoid colon are predominantly benign, and the localization is atypical. In terms of numbers, a localized single polyp (1-2 units) is formed in this section.
The spread of hyperplastic polyps accounts for 3-5% of all cases of polyposis disease of various parts of the intestine. However, clinicians are confident that the figures are significantly underestimated due to the lack of primary symptoms in many patients with small tumors.
Complications of the disease
In patients who ignore the signs of the disease, colon polyps can provoke various complications:
- intestinal bleeding;
- intestinal obstruction;
- severe forms of anemia.
The most dangerous complication of colon polyposis is colorectal cancer. This disease poses a serious threat to the patient’s life and requires complex combined treatment - surgery, chemotherapy, and radiation therapy.
About the risks of colorectal cancer and the importance of timely diagnosis of colon polyps, watch the video:
The only complication that threatens patients who have undergone the procedure for removing polyps in the large intestine is intestinal perforation, when a hole forms in the intestinal wall at the site of polyp removal. As a result of the effusion of intestinal contents into the abdominal cavity, peritonitis may develop. Fortunately, such complications occur extremely rarely.
Effective treatment of polyps at ON CLINIC
Modern diagnostic equipment and gentle methods of surgical treatment allow coloproctologists of the Multidisciplinary Medical Center ON CLINIC to diagnose and effectively treat polyps of any size, multiple types (including villous adenomas).
Thanks to the introduction of a modern endosurgical treatment method (transanal endoscopic microsurgery), operations are performed on an outpatient basis, and the patient’s performance is restored in the shortest possible time.
After the operation, the patient is observed in a comfortable day hospital at ON CLINIC under the supervision of the attending physician. Control endoscopy is carried out every year, for preventive purposes - every three years.
Coloproctologists at ON CLINIC will help each patient prevent the development of a dangerous disease. And with the help of preventive studies, the disease can be recognized in time (including asymptomatic polyps), and highly effective treatment will be carried out in accordance with international standards.
ON CLINIC – modern standards of diagnosis and treatment!
Symptoms of intestinal polyps
Most often, polyps exist asymptomatically, until malignancy (malignancy). In those rare cases when the patient has complaints, they are usually vague: abdominal pain, irregular diarrhea or constipation. When a polyp located relatively close to the rectum bleeds, blood may appear in the stool. The further the source of bleeding is from the “exit”, the less noticeable the blood is, since it has time to mix evenly with the intestinal contents. Polyps in the rectal area can manifest as itching in the area of the anus, and if they are large, they can protrude into the anus.
Symptomatic manifestations
Unfortunately, hyperplastic polyps in the rectum rarely have a clear clinical picture. Acute symptoms often occur due to twisting of the long leg, when the sphincteral parts of the intestine are pinched. Sluggish symptoms usually accompany the picture of the underlying disease or factors that led to the formation of polypous foci.
The following main symptoms are identified::
- Intestinal bleeding . Blood may be obvious or diagnosed through a stool test. The darker the blood clots, the higher the pathological focus. Scarlet or red blood indicates that the polyps are located close to the anus.
- Pain in the rectum . The pain may be accompanied by burning and itching. Pharmacy medications and warming procedures can soothe pain.
- Abnormal stool . Destabilization of defecation is determined by frequency, periodicity, and formality. Constipation usually alternates with diarrhea.
- Painful bowel movements . Pathological manifestations are observed with increasing polyp growth.
- Development of iron deficiency anemia.
Symptoms may resemble the course of almost any intestinal disease, including hemorrhoids, purulent lesions of the rectum and colon. In addition, pus, serous exudate, and an abundant mucous component can be released from the rectal canal.