Common causes of the development of pathologies of the large intestine
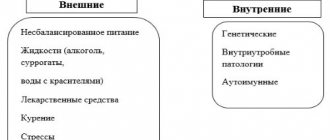
In most cases, diseases of the colon occur as a result of injury to the intestinal mucosa and subsequent inflammation, disruption of its microflora and motility. They lead to:
- Bacteria and infections;
- Stress, nervous tension;
- Taking medications for a long time;
- Allergic reactions;
- Incorrect and unbalanced diet;
- Impaired metabolism;
- Sedentary lifestyle;
- Bad habits (smoking and alcohol abuse).
And only a small part of the pathologies is due to the genetic predisposition of the patient.
What contributes to the development of pathology
Any disease does not appear on its own; a number of root causes and prerequisites contribute to its occurrence. What becomes the detonator of an inflammatory abnormality of the colon? Unfortunately , there are many factors that lead to the formation of this pathology:
- Infections.
- Poor nutrition.
- Intoxication of the body with low-quality products.
- Poor blood circulation in the large intestine.
- Heredity.
- Imbalance of healthy microflora.
Inflammation of the large intestine can manifest itself in the following pathologies:
- Enteritis.
- Duodenitis.
- Mesadenitis.
- Colitis.
In this case, the inflammatory phenomenon can occur in:
- Chronic form (from 6 months).
- Acute form (up to 12 months).
In addition, pathology can develop in any part of the intestine:
- Blind.
- Direct.
- Duodenum.
- Sigmoid.
- Large intestine.
Constipation is a common cause of colon inflammation
Colitis (inflammation of the mucous membrane of the large intestine) can be of several types:
- Spicy.
- Chronic.
- Ulcerative.
- Spastic.
- Crohn's disease.
Diagnosis of pathologies is carried out only by a doctor, who, after examination, prescribes appropriate treatment.
Signs and Symptoms of Colon Diseases
Diseases of the colon are among the most common diseases of the gastrointestinal tract. They all have similar primary symptoms:
- Abnormal stool – some patients complain of constipation, others – of diarrhea;
- Bloating – especially bothersome in the afternoon;
- Abdominal pain that subsides in the evening.
The first sign of the disease, as a rule, is mild pain in the abdomen and anus. As the disease progresses, the following are added:
- The presence of mucus or blood in the stool;
- Increased gas formation;
- Severe signs of neurasthenia (irritability, insomnia), possible depression and tearfulness;
- Weakness, fatigue, apathy.
If you experience such signs, it is advisable to immediately consult a doctor. This way you can prevent the development of intestinal pathology and possible complications.
Symptoms
An inflamed colon will not remain silent about itself, especially if the inflammation of the mucous membrane has become a reaction to the development of the disease. Therefore, a person is unlikely to feel well, but rather will notice the following symptoms:
- abdominal pain without clear localization;
- pain in the anus or rectum;
- pain may increase with bowel movements;
- false urge to defecate, increased frequency of urges;
- change in stool color and odor, feces become foul-smelling;
- diarrhea or constipation, they can also be alternate;
- there are impurities of mucus, pus or even blood in the stool;
- Instead of feces, only mucus may come out;
- rumbling and bloating;
- flatulence;
- loss of appetite and weight;
- Sometimes intoxication phenomena are observed - nausea, vomiting, dehydration;
- increased body temperature;
- general malaise and weakness;
- decreased performance.
If a person notices several or even all of these symptoms, then these are symptoms of inflammation of the large intestine, and in order to successfully restore the mucous membrane from damage, you need to contact a gastroenterologist or proctologist for treatment, as well as a comprehensive diagnosis.
Irritable bowel syndrome
This disease is associated with problems with bowel movements and pain in the large intestine. Irritable bowel syndrome is caused by abnormal movement of the intestinal walls. This movement causes pain and various disorders in the functioning of the organ.
Treatment of the disease comes down to lifestyle changes. It is necessary to minimize stressful situations (the most common cause of illness). Regular exercise is very important to improve bowel function. It is important for recovery to give up bad habits that negatively affect the functioning of the organ.
If the symptoms of the disease intensify, you can relieve cramps with a warm compress on the stomach. In addition, drinking warm water is recommended. It is also worth remembering that this disease is characterized by alternating constipation and diarrhea.
It is also necessary to pay attention to nutrition. You should exclude sweets, high-fat dairy products, coffee, red meat, alcohol and foods with a large number of different flavor enhancers and additives from your diet. Conversely, it is recommended to eat low-fat yogurt, fruits and vegetables, lean fish, and poultry.
Typhlitis
Topical diagnosis is often difficult, which is explained by the polymorphism and nonspecificity of the clinical picture of the disease. A diagnostic search for suspected typhlitis involves a comprehensive examination of the patient using modern laboratory and instrumental studies. The most informative are:
- Microscopic examination of stool
. The coprogram contains a large number of striated muscle fibers, starch grains and plant fiber. The development of the inflammatory process is indicated by the acidic reaction of feces and the abundance of iodophilic microflora. Additionally, a fecal occult blood test is performed to exclude bleeding from the intestines. - Ultrasound of the abdominal organs
. In the case of typhlitis, sonography can detect thickening and swelling of the cecum, smoothness of the folds of the mucosa. Also, during an ultrasound of the abdominal organs, attention is paid to the condition of the appendix and adjacent parts of the intestine. In the initial stage of the disease, the method may not be informative enough. - X-ray examination
. Survey radiography of the abdominal cavity is performed for the purpose of express diagnosis and assessment of the general condition of the gastrointestinal tract. To visualize the structure of the cecum, irrigoscopy with double contrast is performed. With typhlitis, narrowing of the intestinal lumen, flattening of the haustra, deformation and shortening of the cecum are detected.
In a general blood test, typical signs of an inflammatory process are observed: leukocytosis, an increase in ESR, and the possible appearance of granularity in neutrophils. In a biochemical blood test, all indicators are usually within normal limits. To establish the etiology of the disease, bacteriological culture of stool is carried out, followed by determination of the sensitivity of the isolated microorganisms to antibiotics. In difficult cases, diagnostic laparoscopy is recommended.
First of all, typhlitis must be differentiated from acute appendicitis. Ultrasound data (thickening of the walls of the cecum, absence of changes in the appendix) are of decisive importance in making the correct diagnosis. The rate of development of the disease is also taken into account (acute onset is characteristic of appendicitis) and the presence of symptoms of peritoneal irritation. In elderly patients, differential diagnosis with tumor formations must be carried out. Patients with typhlitis are examined by a proctologist and surgeon.
Ischemic colitis
When the arteries of the large intestine narrow and become blocked, blood flow decreases and as a result, ischemic colitis occurs. Reduced blood flow causes pain in the peritoneum on the left side and leads to injury to the colon. Blockage leads to the death of intestinal tissue and therefore requires immediate surgery to remove the dead tissue. This problem is mainly faced by people over sixty years of age.
The situation is aggravated if symptoms appear on the right side. Blood passing through the arteries on the right side supplies both the large and small intestines. Painful manifestations in this case are more intense.
Risk factors include age over sixty, high cholesterol, bleeding disorders, heart failure, and previous abdominal surgery. Seeing a doctor is necessary if the pain is severe enough to prevent you from sitting, and if there is bleeding in the stool.
Treatment for ischemic colitis involves the use of antibiotics (prescribed only by the attending physician) or surgery to remove or repair the damaged part.
Collagen colitis
Refers to microscopic colitis. The disease develops due to an increase in the number of white blood cells in the intestinal epithelium. Women over the age of forty-five most often face this problem.
Treatment is carried out according to traditional therapy prescribed by the attending physician. In this case, medications based on the topical steroid budesonide are prescribed. A diet is also suggested. All foods that can stimulate peristalsis are excluded from the diet - coffee, fatty meat and fish, smoked meats. It is also useful to use decoctions of herbs such as cinquefoil, fireweed, and oak bark.
Ulcerative colitis
Inflammation, during which ulcers and erosions form on the inside of the colon. Characteristic signs of the disease are aching pain on the left side of the abdomen, diarrhea, and in advanced cases, bleeding after defecation. The causes of ulcerative colitis have not been established.
Symptoms of the disease include bleeding from the rectum, diarrhea, and pain on the left side of the peritoneum. Weakness and fatigue are observed.
Treatment is based on the use of hormonal and basic therapy. Patients are prescribed anti-inflammatory drugs, including aminosalicylates, corticosteroids and immunosuppressants. The main goal of drug therapy is to eliminate erosions and prevent relapses.
In nutrition, it is necessary to use the following diet:
- The diet should consist of foods rich in proteins and vitamins;
- Low-fat varieties of meat and fish, vegetables are recommended;
- It is advisable to steam all products.
Types of inflammation of the large intestine and their signs
The formation of colitis is based on an inflammatory process, which gastroenterologists divide into two types of course: acute and chronic.
Acute colitis
This type of inflammation is most often diagnosed in people aged 17 to 40 and from 55 to 70 years. The high incidence rate in these groups is due to frequent contact with various infections and a weakened digestive system due to non-compliance with the rules of healthy nutrition and systematic use of medications that aggressively affect the mucous membrane of the stomach and intestines.
Acute colitis can occur with pronounced symptoms, such as:
- pain;
- nausea, vomiting;
- bloating;
- frequent painful urge to defecate;
- mucus discharge from the anus;
- diarrhea;
- purulent-blood impurities in the stool.
These symptoms may include: general malaise, weakness, fever, weight loss (cachexia), arthralgia and myalgia.
Severe inflammation, especially in patients with weak immunity, causes the appearance of abscesses of the intestinal wall, dehydration shock, sepsis, and peritonitis.
Sometimes the acute form has a different picture of the disease: for several weeks the patient suffers from diarrhea, he has gurgling and discomfort in the abdomen, and other local minor symptoms are possible. Due to their apparent insignificance, the patient does not associate them with serious inflammation. And during the latent course, colitis can develop into a chronic form.
Chronic colitis
It manifests itself in cyclical relapses and leads to difficult-to-treat dysfunctions of the digestive system. In the chronic form, there is a high risk of developing various complications from the gastrointestinal tract. Most often, ulcerative or destructive-degenerative lesions of the submucosal and mucosal colon, bleeding (internal), and various types of neoplasms (benign and malignant) occur.
The changes that occur in the organ during chronic inflammation of the large intestine are as follows:
- the intestinal walls become thinner and the lumen in the affected area narrows;
- the blood supply to the affected area is disrupted;
- ulcers that arise on the surface penetrate into the muscular layer of the intestine, suppuration appears;
- the appearance of neoplasms – pseudopolyps – is possible.
When examining the blood, a clear picture of inflammation is observed - pronounced leukocytosis.
The following symptoms are possible:
- alternate attacks of diarrhea and constipation are observed;
- there are pain sensations in the abdominal area without a specific localization, they are aggravated by nausea and belching;
- there may be a frequent urge to defecate with the release of mucus along with streaks of blood;
- flatulence and bloating;
- loss of appetite, bitter taste in the mouth;
- discharge of feces with a foul odor.
The patient's general health ranges from satisfactory to extremely uncomfortable. Against the background of weakness and malaise, performance decreases significantly, irritability and nervousness increase.
Symptoms of different types of colitis
In the early stages of colon inflammation, the following symptoms may occur:
- rumbling in the stomach;
- the urge to defecate or frequent bowel movements;
- a feeling of slight discomfort in the intestines before or after bowel movements.
These symptoms are mild and may not interfere with the patient’s normal rhythm of life, but as inflammation develops, others may join the listed symptoms:
- nausea, sometimes vomiting;
- abdominal cramps;
- general malaise.
After this stage, which often becomes chronic, ulcerative colitis may develop. Erosion appears on the intestinal walls, which can cause bleeding. Even purulent or mucous formations may occur.
Pseudomembranous colitis
This type of colitis occurs with long-term use of drugs against bacteria - antibiotics. The result of such treatment may be fibrinous plaques. Symptoms can be different, it all depends on the stage of the inflammatory process:
- In mild cases, diarrhea may occur, which will subside quickly. The symptoms resemble those of a digestive tract disorder.
- With moderate severity, the disease has a clearer picture - the patient experiences a false urge to defecate, abdominal pain, mucus and blood may be observed in the stool, and possibly bloating.
- In severe forms, disturbances in the heart area are observed: tachycardia and hypotension may develop, and sometimes rectal perforation occurs.
Nonspecific ulcerative colitis
This type of inflammation is more common in women than in men. The average age of patients with this diagnosis is 20-40 years.
The disease is characterized by hemorrhagic inflammation of the colon with the following symptoms:
- severe pain (mainly in the left abdominal area);
- low-grade fever;
- bleeding from the rectum;
- chronic constipation;
- discomfort in the joints;
- bloody and purulent discharge from the anus.
Over time, such symptoms become less pronounced, creating a period of remission, but as the disease worsens, the patient’s condition becomes serious. The following may occur: diarrhea, pain, anemia develops (due to blood loss), physical exhaustion.
This type of colitis is very dangerous due to complications:
- development of intestinal expansion;
- frequent internal bleeding;
- risk of perforation of the intestinal walls, peritonitis;
- creating favorable conditions for the occurrence of oncology.
Spastic inflammation of the large intestine
This colitis is a functional disorder, which means it is not a severe pathology. It occurs against the background of chronic fatigue, stress, etc.
This inflammation is based on spasms, contractions of the intestinal walls of varying strength and frequency, which leads to the patient experiencing symptoms such as:
- flatulence;
- pain.
- constipation;
- difficult bowel movements or diarrhea;
Spastic colitis is less dangerous than the others. Its main symptom is considered to be transformed feces, resembling round sacs in appearance. When defecating, the patient may feel pain.
Enterocolitis
Enterocolitis combines an inflammatory process in the large intestine with damage to the gastric mucosa. Acute enterocolitis occurs due to infection or non-infectious exposure (allergens, poisons, food poisoning, chemicals).
Primary inflammation may appear suddenly:
- spasmodic pain in the abdominal area;
- bloating, rumbling in the stomach;
- nausea, sometimes vomiting;
- diarrhea.
If enterocolitis is of infectious origin, then blood and mucus may appear in the stool, the temperature may increase, there will be an abundant white coating on the tongue, and when palpating the abdomen, pockets of pain will be detected.
Crohn's disease
A rare disease that affects not only the large intestine, but the entire digestive tract. Doctors identify two possible variants of its origin:
- infectious cause of inflammation (then the disease responds well to treatment with antibiotics);
- autoimmune (it is assumed that immune cells begin to damage the tissues of their own intestines).
Other organs may be affected. Stomatitis, conjunctivitis, arthritis in the joints, cirrhosis of the liver, inflammation of the bile ducts, and pyelonephritis develop.
Prednisolone and Sulfasalazine are used in treatment. In case of exacerbation, a course of antibiotics is prescribed.
In addition, be sure to follow a strict diet. Smoked meats, sweets, fatty meats and fish, coffee, and chocolate should be excluded from the diet.
Remember that self-medication in the case of such a serious illness is unacceptable. Drug treatment is prescribed only by the attending physician.