Principles of surgical tactics
In a broad sense, GERD occurs as a result of disturbances in the acid balance of the upper gastrointestinal tract (primarily the esophagus), which are caused by its motor dysfunction in combination with excessive secretion of hydrochloric acid by the stomach and a hiatal hernia, which seriously complicates the course of the disease.
Any surgical intervention carries certain risks: blood loss, postoperative complications in the form of infections, thrombosis, myocardial infarction, diabetes, unexpected allergic reactions to drugs and materials.
An adequate assessment of these risks depends on the results of the examination (the degree and nature of inflammatory changes), laboratory data, knowledge, experience, intuition and the depth of clinical thinking, which form the basis of medical art.
The tactics of surgical intervention depend on the nature and scale of complications of GERD, which sometimes have atypical clinical manifestations (for example, cough, pneumonia).
Note! The most dangerous and sudden complication of GERD due to perforation (rupture) of the esophagus is pneumothorax - penetration of air into the pleural cavity, it instantly causes compression of the lung, can lead to disability and even death if the person is not operated on in time.
Each type of operation has its own specifics, indications, and advantages. The success of the operation depends to a large extent on the treatment that precedes it, concomitant diseases, the patient’s preoperative preparation, including psychological, and his motivation.
Gastroesophageal reflux disease (GERD, or reflux esophagitis) is the most widespread gastroenterological disease, occurring in young and middle-aged people, who make up the most able-bodied part of the population [1, 2]. The prevalence of reflux esophagitis in developed countries reaches 50-60% and is steadily growing every year [3], which determines the relevance of this work.
This disease is multi-etiological, but the main cause of development in 90% of patients is a sliding hiatal hernia (HH) [3, 4]. The prognosis for a patient suffering from reflux esophagitis is determined by complications of the disease, such as peptic stricture, Barrett's esophagus, and ulcerative lesions of the esophagus [3, 5]. Developed drug therapy regimens using modern and most effective drugs have significantly reduced the risk of complications and increased the level of quality of life. However, it is necessary to understand that the cause of the development of the disease is an organic pathology, which is not possible to influence with medication [5]. Conservative therapy, including recommendations for following a certain lifestyle and diet and drug therapy, is aimed only at relieving the symptoms of reflux esophagitis, and not eliminating the causes of the disease [5, 6]. Thus, conservative therapy only delays the development of life-threatening complications and surgical treatment. Patients are forced to take medications for a long time [7].
According to many authors [7, 8], relapse of symptoms of the disease such as heartburn, chest pain and epigastric pain, bitterness in the mouth occurs in 50% of patients 3 months after cessation of therapy, and in 100% after 6 months.
Even the newest drug with a modified release of the active substance, dexilant, developed in the USA and available for sale in Russia since 2014, which belongs to the group of proton pump inhibitors for the treatment of reflux esophagitis, is only a modification of some drugs of the same group with a similar pharmacological effect [9, 10].
It is also important to note that, according to world literature [8] on the treatment of GERD, there is a group of patients with reflux esophagitis due to hiatal hernia (40%) for whom conservative therapy does not bring the desired effect. These patients are most at risk of developing life-threatening complications and are therefore candidates for surgical treatment of a sliding hiatal hernia.
Particular attention should be paid to extraesophageal clinical manifestations of reflux esophagitis, which are divided into abdominal, bronchopulmonary, cardiac, otolaryngeal and dental [11-13]. The reasons for the development of these manifestations are gastroesophageal reflux itself, regardless of the amount of the aggressive component contained in the refluxate [11, 13-15]. Thus, the main etiological factor in the development of extraesophageal symptoms of reflux esophagitis is not an increase in the acidity of gastric juice and a decrease in bicarbonates and mucin of the esophageal mucosa, but a violation of the valve mechanism of the cardia [16, 17].
The above does not mean that every patient with reflux esophagitis must be subjected to surgical treatment, but it should be understood that sooner or later the question of surgical intervention has to be raised [8, 18]. It is this issue that has recently caused the most heated discussions in the treatment of reflux esophagitis.
This is largely due to the number of unsatisfactory results of surgical treatment, which, according to many surgeons [19], reaches 30%, as well as the ineffectiveness of drug therapy. In our opinion, the ineffectiveness of antireflux techniques is associated with the wrong choice of surgical treatment technique. Currently, a number of issues relating to the surgical treatment of reflux esophagitis have not yet found their final solution. The inability to avoid serious complications characteristic of different fundoplication methods explains the need for a constant search for the most effective, safe and technically easy to perform anti-reflux surgery.
With the advent of minimally invasive technologies, almost all methods of surgical treatment of hiatal hernia and reflux esophagitis are performed laparoscopically [20, 21]. The low invasiveness of interventions, short rehabilitation periods, and good cosmetic effect have made minimally invasive endovideosurgical antireflux interventions the “gold standard” for surgical treatment of reflux esophagitis and the method of choice for almost any hiatal hernia [22].
However, data from a comparative analysis of the results and effectiveness of laparoscopic techniques carried out by many authors have shown that the results of operations in the immediate and late postoperative periods are practically no different from the results of open interventions. Thus, the number of complications of laparoscopic fundoplications also reaches high figures [23–25].
It should also be noted that an important reason for the ineffectiveness of fundoplications is often the overestimation by some clinicians of the indications for laparoscopic antireflux operations. It is known that the introduction of minimally invasive technologies has made it possible to make a significant step forward in reducing the trauma of surgical interventions [24, 26, 27]. In antireflux surgery, the indications for surgical treatment of patients with reflux esophagitis remained the same, with the exception of general contraindications for laparoscopic surgery. However, the desire of some surgeons to follow technical progress and use new minimally invasive technologies to reduce recovery time and disability of patients leads to an increase in the number of indications for performing laparoscopic surgery instead of open surgery. To achieve the best results from these operations performed laparoscopically, surgeons must adhere to clear indications.
Patients with shortened esophagus deserve special attention. As is known, shortening of the esophagus develops due to the action of the aggressive component of the refluxate on the wall of the esophagus, causing first inflammatory changes in it, and then destructive ones [18]. By contracting and dragging the cardia and fundus of the stomach into the posterior mediastinum, the esophagus aggravates the development of hiatal hernia and gastroesophageal reflux [28]. When the esophagus is shortened and it is impossible to bring the cardiac part of the stomach into the abdominal cavity, a fundoplication cuff sometimes has to be formed in the posterior mediastinum 5-10 cm above the diaphragm, which is technically much more difficult [21, 29]. Therefore, such patients require a special individual approach when choosing a surgical treatment option. It should be understood that surgical treatment is not aimed at eliminating the sliding hiatal hernia, but at recreating the acute angle of His and containing reflux [29].
At the beginning of the 21st century, the US Food and Drug Administration (FDA) introduced two techniques for the treatment of reflux esophagitis - the transoral rotational esophagogastric fundoplication technique (TIF procedure), performed with using the EsophyX device, as well as the LINX system (developed by the American private company Torax Medical for the production of medical devices). These techniques were supposed to become an alternative to antireflux interventions performed laparoscopically [30–32]. However, after some time, publications by different authors began to appear in the literature [31, 33-35], who were faced with an even greater number of complications. There are often reports of complications of procedures such as bleeding, subdiaphragmatic abscesses, and perforations. Moreover, the presence of a large number of contraindications to these procedures make them inapplicable for patients with large hiatal hernias and complicated forms of severe reflux esophagitis [30].
Specialists of the Russian Scientific Center of Surgery (RSSC) named after. acad. B.V. Petrovsky have extensive experience in treating patients with reflux esophagitis, dating back to 1979 [36, 37]. In our opinion, fundoplication as modified by RNSC is the most optimal surgical intervention for the treatment of patients with reflux esophagitis. The vast experience of performing this technique convincingly proves and allows us to confidently assert its advantages as an operation that is devoid of many disadvantages and allows one to avoid complications characteristic of other techniques [15, 23, 34]. A good result is achieved in 95% of observations [19, 28, 38].
The analysis of the entire experience of treating these patients allowed us to formulate clear indications for surgical treatment of reflux esophagitis. Thus, the indications for antireflux surgery are:
— severe reflux esophagitis against the background of hiatal hernia;
— reflux esophagitis due to hiatal hernia, not amenable to conservative treatment;
- reflux esophagitis complicated by Barrett's esophagus (without dysplasia) or peptic stricture of the distal esophagus;
— extraesophageal manifestations of reflux esophagitis against the background of hiatal hernia.
In case of shortening of the esophagus of the first degree, antireflux surgery should be started laparoscopically, but it should be taken into account that the likelihood of switching to laparotomy at the stage of formation of the fundoplication cuff is high due to the impossibility of adequate visualization and the lack of room for manipulation. In case of II degree shortening of the esophagus, it is advisable to perform fundoplication from a laparotomic approach [18, 37, 39].
Thanks to the performance of fundoplication using the RNSC method for the above indications, high clinical effectiveness of this anti-reflux operation in the treatment of patients with reflux esophagitis was achieved. Efficiency is 95%.
The authors declare no conflict of interest.
* e-mail; https:/orcid.org/0000-0002-0484-5022
When surgery is unavoidable
Indications for surgery are the complete ineffectiveness of drug treatment for GERD in combination with the following manifestations:
- obstruction of the esophagus (or its real imminent prospect);
- bleeding of ulcers of any location;
- the presence of persistent lesions of the mucous membranes of the upper gastrointestinal tract and respiratory tract against the background of ongoing episodes of reflux;
- hernia of the esophagus and stomach;
- extensive or multiple erosive and ulcerative lesions of the walls of the esophagus.
Gastroesophageal reflux disease - symptoms, treatment
Clinical symptoms are associated with the impact of gastric contents on the walls of the esophagus and the development of esophagitis.
- Heartburn is the most common complaint of patients with GERD with esophagitis. It manifests itself as a burning sensation behind the sternum, which occurs after eating or at night. The appearance of heartburn is provoked by drinking carbonated drinks and performing physical exercises, in particular, bending forward. This is due to the fact that in an inclined position of the body, as well as in a lying position, conditions are created for gastric contents to enter the esophagus.
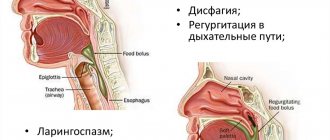
- Dysphagia is a swallowing disorder. This symptom occurs as a result of spasm of the esophagus, making it difficult to accept even liquid and soft food. Dysphagia may be a manifestation of complications of GERD or an esophageal tumor.
- Belching with sour contents, a feeling of bitterness in the mouth after a night's sleep.
- A quick feeling of fullness while eating, which may be accompanied by nausea and even vomiting.
- Extraesophageal manifestations of gastroesophageal reflux disease - chest pain, cough, sore throat, hoarseness. Substernal pain is of a compressive nature and can radiate to the collarbone and to the left side of the chest. In this case, the pain goes away within a few minutes after taking antacid medications. This feature is an important point in the differential diagnosis of GERD and cardiac pathology that has similar symptoms.
If symptoms bother you more than 2-3 times a week for several weeks or months, you should consult a gastroenterologist.
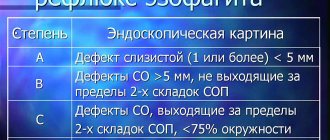
Depending on the degree of damage to the esophagus, detected during endoscopic examination (esophagogastroduodenoscopy), 2 forms of the disease are distinguished:
- endoscopically positive - GERD with esophagitis, in which visible erosive or ulcerative lesions of the mucous membrane are observed in the lower part of the esophagus (erosive form);
- endoscopically negative - GERD without esophagitis, in which there are no visible damage to the esophagus (non-erosive form).
The long course of the disease can have adverse consequences in the form of Barrett's esophagus, a condition characterized by metaplasia of epithelial cells. This pathology is a precancerous disease and can cause the development of adenocarcinoma (cancer) of the esophagus.
Esophagus problems
Inflammatory changes in GERD, which affect the esophageal walls, can cause varying degrees of obstruction of the esophagus and eating disorders. Such violations are both reversible and irreversible.
Strictures (narrowing of the lumen) are formed as a result of scar tissue thickening during the healing process. They significantly reduce the motor properties of the esophagus and a person’s quality of life: rough scars irreversibly reduce the elasticity of the esophageal tube and make swallowing difficult.
In general, surgery is performed in the following cases:
- complete or partial stricture, which significantly impedes the passage of food;
- complete insufficiency of the lower esophageal sphincter (LES);
- complicated ulcer (edematous, infected, profusely bleeding, causing extensive necrotic changes in surrounding tissues);
- tumors of the esophagus, significantly narrowing its lumen, especially malignant ones;
- signs of Barrett's esophagus (BE) of a certain modification.
Of course, cases of irreversible, life-threatening complications require surgery, but still such a division is very arbitrary. Even with adequate therapy, disorders that seemed reversible can take on the opposite character (the ulcer suddenly begins to increase in size or bleed). Conversely, intensive therapy (for example, in preparation for surgery) sometimes causes stable remission, allowing it to be avoided.
In special cases (deep, extensive lesions, large tumors), doctors have to remove entire fragments of the esophagus during abdominal surgery. Modern clinics perform prosthetics of the esophagus and LES.
Types of surgeries for the treatment of GERD
Conventionally, surgical operations performed to treat gastroesophageal reflux disease can be divided into two types.
- Surgery to treat the immediate causes of GERD.
- Elimination of consequences or complications that developed as a result of incorrect or untimely treatment.
The first type of surgical treatment is carried out as planned. The second type is often performed urgently, for example, as a result of massive bleeding.
Gentle surgical methods
Modern high-tech (so-called minimally invasive) treatment methods involve the insertion of a special probe into the esophagus. With its help they carry out:
- visual examination of mucous membranes, assessment of the size and condition of the affected areas;
- taking a biopsy sample (a piece of tissue) to assess cancer risks;
- for narrowing of the esophagus - bougienage (gradual stretching of the lumen of the esophagus using a special hollow balloon into which air is pumped), carried out in several stages, surgical dissection of strictures;
- for BE, erosions, superficial ulcers - argon coagulation (cauterization) of the surface of the affected tissue in several sessions (to prevent the formation of scars);
- argon resection (removal) of the upper layer of the esophageal wall.
Important! The volume and tactics of surgical intervention for BE depends on the location and degree of damage to the mucosal area.
The described methods of surgical treatment are performed using a plasma generator and are used for small volumes of intervention. They are expensive, but short-lived, significantly reduce (and even completely eliminate) blood loss, and make it possible to provide assistance to patients with contraindications to abdominal surgery.
Rehabilitation period
After the operation, the patient is prescribed antibacterial medications to prevent infection. They resort to painkillers because in the first days after surgery, patients complain of pain. The next day the patient is allowed to get up and drink fluids. After 2 days, an X-ray examination is performed using a contrast agent, which makes it possible to determine the patency of the esophagus. On day 3, it is permissible to consume vegetable broths. Meals are gradually expanded, patients are allowed to include pureed foods on the menu. The patient is allowed to return to the usual diet, which is prescribed for reflux esophagitis, 1 month after surgery.
After surgical treatment, it is recommended to exclude carbonated drinks from the diet.
It is important for people to take into account that after surgical treatment they will be unable to vomit and will not be able to burp effectively, since the air that accumulates in the gastrointestinal tract is not able to escape through the esophagus. Therefore, patients are advised to exclude carbonated mineral water and drinks from their diet.
It's a matter of time
The question of surgical intervention arises when there is simply no alternative to it. The surgeon does not have the task of “cutting” every first patient.
But in emergency situations, when it comes to the life and death of a person, and time counts by minutes, the surgeon does not have the opportunity to make optimal medical decisions. You need to understand that by postponing a visit to the doctor for years, each person increases the likelihood of such a situation.
When the operation is planned in advance, the doctor has time to examine and adequately prepare the patient, assess possible risks and, if possible, reduce their level, develop the optimal strategy and tactics of surgical intervention.
How to prepare?
Before surgery, the patient will need to be examined by a nutritionist, surgeon and gastroenterologist. Then you need to go for an x-ray and attend an endoscopy, during which a sample is sometimes taken for a biopsy. The person then undergoes a manometric test, which shows the contraction of the muscles of the esophagus. 14 days before surgery you will need to stop using Aspirin and other medications that can thin the blood. The day before surgery for reflux esophagitis, it is permissible to eat only foods that are easily digestible. Drinking is prohibited 8 hours before your scheduled surgery.
What is a hiatal hernia
Under physiological conditions, the stomach is located under a kind of “roof” in the form of a diaphragm, a flat muscle-septum separating the chest and abdominal cavities. The diaphragm has a small opening through which the esophagus passes, which is logically called the esophagus. The junction of the esophagus with the stomach is located below the diaphragm, but quite close to the esophageal opening.
Under certain conditions, the upper (fundic) part of the stomach and part of the esophagus are squeezed up through the esophageal opening into the chest cavity. This protrusion is called a hernia. The diaphragm, being a large muscle that holds the heart and lungs, relaxes only momentarily during exhalation and securely holds the stomach in an unnatural “bifurcated” state.
Change of status
In such a situation, the LES is pressed from below by the protruded part of the stomach, causing its partial or complete opening and provoking reflux. The presence of a hernia makes no sense in any antireflux therapy, including coagulation of the affected mucosa.
The muscle tone of the LES is directly related to the position of the stomach in the abdominal cavity. Sometimes, due to various reasons (exorbitant physical effort, injuries that weaken muscles), prolapse of the stomach occurs. It reflexively reduces the muscle tone of the LES, which also contributes to the appearance of reflux. Only fundoplication surgery can return the stomach to its original position and guarantee the elimination of episodes of reflux.
Concerns about surgical treatment
Surgery, on the other hand, is associated with a very low, but immediate, risk of general anesthesia and direct complications. Laparoscopic techniques have reduced the degree of surgical trauma and shortened hospital stay, but the risk has not been completely eliminated and there is still the possibility of a prolonged period of surgery-related ill health in some patients. Patients are also concerned that the effects of surgery will not last long and they will eventually have to take medications again to control GERD symptoms. This concern is supported by the recently published results of a longitudinal collaborative study comparing patients randomized to medical or surgical treatment. After an average of 10 years of follow-up, more than half of the patients in the surgical group resumed taking antacids [1].
What contributes to the formation of a hernia
The walls of the stomach, consisting of muscle fibers, are much thicker than the intestinal walls, but they are very elastic, mobile and easily stretched. The appearance of a hernia is caused by excess pressure in the abdominal cavity, expansion of the stomach (as a result of injury, infection, damage to the splanchnic nerve) and systematic overeating.
Overfilling of the stomach gradually stretches and thins its walls, causing, in addition to a hernia, dangerous circulatory disorders and degenerative changes in the mucous membranes, which can lead to tissue death (necrosis).
Gastric fundoplication
Antireflux fundoplication surgery involves fixing the stomach in a position that prevents its re-protrusion. To put it simply, the “problem” part of the stomach is placed in place, but since it turns out to be stretched, it is slightly pulled up and sutured in the form of a cuff, wrapped around the lower part of the esophagus.
Laparoscopic fundoplication is a gentle method of surgical intervention that avoids abdominal incisions. Only four punctures are made in it, into two of which miniature cameras are inserted for an internal view of the abdominal cavity, and into the other two - manipulators are inserted, through which the necessary actions are carried out.
Contraindications for surgery are:
- conditions after removal of the stomach or spleen;
- dysfunction of a certain type of esophageal motility;
- relapses of reflux after similar operations performed in the past;
- ulcers, esophageal strictures, BE.
Minimal trauma during fundoplication allows one to shorten the patient's hospital stay and avoid the formation of adhesions. Laparoscopic fundoplication surgery has a good cosmetic effect and can be performed without the use of narcotic analgesics, respiratory depression and consciousness.
Treatment of gastroesophageal reflux with esophagitis
I. Conservative treatment
According to the literature, up to 90% of patients with uncomplicated forms of reflux esophagitis can be treated with conservative methods. First of all, these are dietary restrictions. It is necessary to refrain from bad habits, since smoking and drinking alcohol not only irritates the mucous membrane, but also leads to dysfunction of the esophageal sphincter. You can receive recommendations for drug therapy by scheduling a consultation.
II. Surgical treatment of reflux disease
Indications for surgical treatment are:
- Ineffectiveness of intensive conservative therapy, manifested by the persistence of painful heartburn or pain, progression of the disease or the addition of complications.
- Ulcerative reflux esophagitis in the absence of positive dynamics after a course of intensive treatment.
- Complicated reflux esophagitis (bleeding, pneumonia, bronchitis).
The goal of surgical treatment for reflux esophagitis is to eliminate pathological gastroesophageal reflux. Today, a number of operations of varying degrees of complexity are used in world practice. In our opinion, the risk of surgical intervention should not exceed the risk of the disease itself. When choosing the scope of the operation, we take into account the severity of reflux esophagitis, the degree of violation of the size of the esophageal opening of the diaphragm and the angle of His. We prefer Nissen fundoplication. During this operation, a circular cuff is formed by suturing the anterior and posterior walls of the stomach around the abdominal segment of the esophagus. If necessary, in addition, posterior crurorrhaphy is performed (reducing the size of the esophageal opening of the diaphragm by suturing the posterior legs of the diaphragm).
In our Clinic, most of these operations are performed endovideosurgically (laparoscopically). In this case, the hospital stay after surgery is reduced to 1-2 days. You can clarify the feasibility of surgical treatment and choose the optimal method by undergoing an examination and consulting with a specialist.
Open your mouth wider
Sometimes the pathologies accompanying GERD are such that it is not possible to perform laparoscopic gastric fundoplication. The level of development of medical technologies makes it possible to perform transoral fundoplication.
It is performed without any external incisions at all, which significantly reduces the risks of postoperative complications and is practically painless. A special manipulator is inserted through the mouth into the LES area and further into the stomach cavity. Operating from the inside, remotely controlled grippers tighten and suture the stomach.