A gastric biopsy is a diagnostic procedure of taking a sample of tissue from the stomach lining and then examining it under a microscope. The tissue sample is called a biopsy. From a medical point of view, a biopsy sample is taken intravitally.
A biopsy is considered mandatory if cancer is suspected. Only under a microscope can you see the structure of a tissue sample and determine the presence and type of cancer cells. For this purpose, a special database of visual images of all studied cancer cells has been developed. They are simply compared with the sample taken.
However, in recent years, gastric biopsy has become increasingly used for the diagnosis of other gastrological diseases.
There is one subtle point in this procedure - the introduction of an endoscopic probe. Yes, the procedure is not dangerous and without pain. However, there are people who are not psychologically ready for it. The urge to vomit prevents the insertion of a probe. You just need a psychological attitude.
What is a gastric biopsy
Gastric biopsy is a diagnostic technique that allows intravital examination of stomach tissue.
When performing a gastric biopsy, organ tissue or individual cells are collected for subsequent histological, cytological or immunohistochemical examination.
To obtain the most reliable information, tissue is collected from several areas of the mucosa (the most suspicious from the point of view of the proposed diagnosis). That is, for one gastric biopsy, three or more samples (biopsy) are usually taken.
Currently, gastric biopsy is widely used in gastroenterological practice. This study is highly accurate, well tolerated by patients and rarely leads to complications.
Gastric biopsy is considered the “gold standard” for diagnosing malignant neoplasms of the stomach and precancerous pathologies of the gastric mucosa. Gastric biopsy is also used in the diagnosis of gastritis, polyps, ulcers, etc.
If Barrett's esophagus or esophagitis is suspected, a gastric biopsy is combined with a biopsy of the esophageal mucosa, and for Crohn's disease and celiac enteropathy - with an intestinal biopsy.
What does a gastric biopsy show?
Gastric biopsy analysis allows:
- assess the cellular composition of tissues;
- assess the secretory function of cells;
- assess the pH level;
- identify Helicobacter pylori;
- identify the presence of atypia (tumor atypical cells);
- carry out differential diagnosis between malignant and benign tumors;
- assess the activity of the inflammatory process;
- establish the type of gastritis (hyperacid, hypoacid, with normal secretion);
- identify rare forms of gastritis (lymphocytic, eosinophilic, granulomatous, autoimmune);
- identify and determine the type of dysplasia of the gastric mucosa;
- identify intestinal metaplasia of the gastric mucosa;
- assess the risk of malignancy of a stomach ulcer or polyp;
- assess the depth of the ulcer, etc.
The importance of a biopsy is confirmed by the fact that surgical treatment of gastric tumors is not performed without histological confirmation of cellular atypia.
The material collected during the biopsy is sent to the laboratory, where it is stained and examined by histological, cytological or immunohistochemical methods.
Stomach biopsy - what is it taken for?
A gastric biopsy is performed when a patient has:
- stomach tumors of any etiology (as well as if there is a suspicion of a tumor or if it is necessary to perform a differential diagnosis between benign and malignant neoplasms);
- chronic gastritis (to clarify the types, stages and activity of inflammatory processes, as well as to assess the risk of transformation of gastritis into gastric ulcer);
- acute gastritis and stomach ulcers, difficult to treat (the study is carried out to clarify the cause of the development of the disease and assess the degree of activity of the inflammatory process);
- long-term non-regenerating ulcers of the stomach and duodenum;
- gastric polyps;
- Barrett's esophagus (stomach biopsy is performed in combination with esophageal biopsy);
- dysplasia of the mucous membranes of the stomach;
- pernicious anemia;
- dyspepsia, combined with anemia, fever, weight loss, jaundice, abdominal pain, etc.;
- dysphagia;
- chemical damage to the esophageal and gastric mucous membranes;
- intestinal metaplasia of the gastric mucosa;
- erosions of mucous membranes;
- space-occupying formations in the epigastrium.
A gastric biopsy is also indicated:
- when other diagnostic methods are not informative;
- after surgical interventions to remove tumors and polyps (to control the quality of treatment and timely detection of relapses);
- when conducting screening methods for diagnosing malignant neoplasms in patients at risk.
Stomach polyp - symptoms and treatment
Based on the number of growths there are:
- single polyps;
- multiple polyps;
- gastric polyposis (more than 20 polyps).
According to the clinical course, some Soviet scientists identified the following forms of gastric polyps:
- asymptomatic form;
- gastritis form;
- anemic form;
- complicated form (bleeding of the polyp and its prolapse into the duodenum);
- combined form (the appearance of a polyp and stomach cancer).
Based on endoscopic features, four types of gastric polyps can be distinguished:
- Type I - flat, raised, with indistinct edges;
- Type II - protruding, semicircular, with fairly clear boundaries;
- Type III - clearly protruding, rounded, with a retracted base;
- Type IV - pedunculated.
All of the above classifications deserve attention. However, in practice, the most important classification is based on the signs of degeneration of polyps into a malignant tumor [1][3].
According to the WHO classification, benign stomach tumors are defined as adenomas (adenomatous polyps). They are divided into papillary and tubular forms. Hyperplastic polyps are separately identified and included in the group of tumor-like processes [2][10].
In 2010, the British Society of Gastroenterology proposed its classification of gastric polyps, and also developed recommendations for patient management for each type of gastric polyp. According to this classification, gastric polyps are divided into five groups:
- Fundic gland polyps.
- Hyperplastic polyp.
- Adenomatous polyp.
- Hamartomatic polyps (associated with developmental defects):
- juvenile polyp;
- Peutz-Jeghers syndrome;
- Cowden's syndrome.
- Polyposis syndromes (nehamartoma):
- juvenile polyposis;
- familial adenomatous polyposis.
Fundic gland polyps are cystic expansions of the stomach's own glands and account for 16-51% of benign polyps. They usually reach 1-5 mm in diameter and are located mainly in the body or fundus of the stomach. They have a smooth, even surface, can be lobulated, and are covered with an unchanged mucous membrane. They can appear as an independent disease or as part of familial adenomatous polyposis of the colon.
Not associated with gastritis and Helicobacter pylori infection. They can form due to long-term use of proton pump inhibitors (drugs that reduce the production of hydrochloric acid). These medications increase the activity of gastrin (a stomach hormone), which stimulates the growth of epithelial cells.
The average development interval for fundic gland polyps is 32.5 months. Regression occurs three months after stopping taking proton pump inhibitors [4][7].
Hyperplastic polyps account for 30-93% of benign gastric polyps. It can be sessile and pedunculated, less than 2 cm in diameter. It is characterized by enlarged gastric pits, dilated and tortuous glands, and chronic inflammation of the gastric mucosa. A single polyp is most often located in the antrum (lower) part of the stomach. Multiple polyps can occur in all parts of the stomach.
Associated with chronic (Helicobacter-associated), chemical and atrophic gastritis. It occurs due to increased cell renewal (their layering on top of each other) in response to damage to the gastric epithelium (usually with erosions or gastric ulcers).
The hyperplastic polyp itself rarely becomes malignant (malignant), but it increases the risk of malignancy of the surrounding inflamed stomach tissue. Therefore, when a hyperplastic polyp is detected, it is recommended to perform a biopsy of the surrounding tissue (from 4-5 different places) [4][5].
Adenomatous polyp is a precancerous disease with a high potential for degeneration into cancer, especially when the polyp is more than 2 cm. It accounts for 3-26% of gastric polyps. Usually single, can be localized in any part of the stomach, but is more often found in the antrum (lower part of the stomach). The structure is tubular, villous and mixed. It occurs against the background of atrophic gastritis and intestinal metaplasia (when the gastric epithelium is replaced by intestinal epithelium) [4].
It is worth noting that in one study at the Vitebsk Regional Clinical Hospital, a hyperplastic polyp with areas of adenomatosis was found. The authors suggested that hyperplastic polyps can transform into adenomatous ones. They also allowed themselves to identify another histological form of polyps - a hyperplastic polyp with focal adenomatosis. It is a true benign tumor of the stomach, capable of developing into cancer [10].
Hamartomatic polyps are rare, but it’s worth saying a few words about them.
A single juvenile (youthful) polyp has no malignant potential, but, like all polyps, it can be complicated by bleeding or strangulation, since such polyps are mainly located in the lower part of the stomach and are susceptible to trauma.
Peutz-Jeghers syndrome is a rare hereditary disease that is accompanied by the appearance of hamartomatous polyps in the gastrointestinal tract, as well as pigmentation in the lips, fingers and buccal mucosa. With this disease, there is a high risk of malignancy of both the digestive organs and the lungs, mammary glands, pancreas, and uterus. Therefore, such patients should be closely monitored.
Cowden's syndrome is a rare hereditary disease that is accompanied by the presence of polyps of the gastrointestinal tract, benign tumors of the mouth, as well as malformations of various organs (breast, thyroid and genitals). Polyps with this syndrome very rarely degenerate into cancer, but still require observation.
Polyposis syndromes include juvenile polyposis and familial polyposis syndrome.
In juvenile polyposis, many juvenile polyps are found that have malignant potential. This disease can also be complicated by gastrointestinal bleeding and enteropathy, a disease of the small intestine that is accompanied by loss of protein and other nutrients.
Familial polyposis syndrome is a hereditary disease with a very high risk of cancer of the stomach and other parts of the gastrointestinal tract. Affected family members have a large number of colonic and rectal adenomas, which have a 100% chance of developing into cancer unless a prophylactic colectomy—complete removal of the colon—is performed. Gastric polyps are detected in 30-100% of cases. This syndrome does not have a clear connection with gastritis caused by Helicobacter [4].
Specific stages of disease development are not distinguished, since different types of polyps have different origins and development. But if we talk about frequently occurring adenomatous and hyperplastic polyps, then we can conditionally distinguish three stages of development [1]:
- polypous gastritis (inflammation or atrophy of the gastric mucosa);
- stomach polyp;
- stomach cancer.
Contraindications
Despite the fact that gastric biopsy is a minimally invasive and minimally traumatic procedure, it has a certain list of contraindications.
Absolute contraindications to performing a gastric biopsy include the presence of the following in the patient:
- ischemic or hemorrhagic strokes;
- myocardial infarction;
- stenotic lesions of the esophagus (with this disease it is not possible to pass a probe from the esophagus into the stomach);
- attacks of asthma (bronchial asthma).
Relative contraindications to performing a biopsy include the presence of the patient:
- fever;
- severe runny nose of any etiology (this is due to the fact that during endoscopy the patient must breathe exclusively through the nose);
- inflammatory processes in the pharynx;
- infections;
- epilepsy;
- bleeding disorders, hemorrhagic diathesis;
- hypertensive crisis;
- HF (heart failure);
- mental pathologies.
Stomach biopsy - preparation
The gastric biopsy procedure does not require complex and lengthy preparation. Before the biopsy, the patient undergoes general tests (blood and urine tests, blood clotting tests, etc.).
The patient must warn the doctor about the presence of concomitant diseases (diabetes mellitus, cardiovascular pathologies, etc.) and about allergies to medications.
Eight to ten hours before the biopsy, you should not eat or drink anything. If the patient has a stenotic lesion of the pylorus, it is recommended to lavage the stomach before the biopsy. This is due to the fact that with pyloric stenosis there is often stagnation of undigested food.
Patients with an easily excitable psyche are premedicated with antispasmodics, tranquilizers and atropine.
To increase the accuracy of the study, the patient is simultaneously subjected to an FGDS and a gastric biopsy.
It should be noted that a gastric biopsy is not painful, but the procedure can cause significant discomfort in the patient (especially due to the gag reflex and difficulty breathing when the endoscope is inserted).
The entire procedure is carried out under local anesthesia (irrigation of the throat with a ten percent lidocaine solution). Irrigation with lidocaine is required to reduce the intensity of the gag reflex when inserting a fibrogastroscope. After passing the endoscope through the pharynx, there is practically no pain.
Minor trauma to the gastric mucosa when collecting tissue with a biopsy needle (or forceps) does not cause pain. Minimal damage to the mucosa heals quickly, so there are no scars left after the biopsy.
Discomfort in the throat and sore throat after the procedure usually disappear within 2-3 days.
Preparing for the study
Proper preparation for gastrointestinal endoscopy is important to obtain accurate data and eliminate even minimal risks of side effects from the procedure. If preparation recommendations are not followed, the physician may have difficulty visualizing tissue, patency of the endoscope, or obtaining detailed images during the procedure. The patient may experience pain, discomfort and disruption of the gastrointestinal tract after endoscopy.
Before performing the procedure, additional examination may be required to exclude the patient’s contraindications to the study:
- general clinical tests and blood biochemistry;
- electrocardiography.
After receiving the results, if there are no restrictions, the doctor sets a date for the examination and gives recommendations for preparation.
Experts advise before gastric endoscopy:
- stop drinking alcohol for 3–5 days;
- stop taking medications that affect the rate of blood clotting within 2–5 days;
- on the day of the study, avoid smoking;
- do not take solid food for 8–10 hours;
- do not take liquids for 2 hours;
- on the day of the examination, take vital medications that the patient takes daily, and drink them with a small amount of water.
For patient comfort, the examination is recommended to be done under sedation. Before sedation, a consultation with an anesthesiologist is carried out.
Gastric biopsy using endoscopy - what is it?
A gastric biopsy is performed during gastroscopy (esophagogastroduodenoscopy, EGDS), an endoscopic procedure that allows you to visualize the walls of the esophagus, stomach and duodenum using a gastroscope.
A gastroscope is an endoscopic instrument (a flexible tube with fiber-optic systems inside) inserted through the mouth into the lumen of the esophagus, stomach, etc.
Video esophagogastroduodenoscopy (VEGDS), performed using a video gastroscope, can also be performed.
Modern gastroscopes are equipped with biopsy forceps. This is due to the fact that sometimes the decision to perform a biopsy arises directly during endoscopy, if the doctor detects suspicious areas of the mucosa.
Types of biopsy
A gastric biopsy can be performed using a surgical endoscopic method. Surgical endoscopy is performed against the background of open surgery.
Endoscopic biopsy is performed during:
- FEGDS – fibrogastroduodenoscopy;
- VEGDS – video esophagogastroduodenoscopy.
According to indications, chromogastroscopy can be performed. This is an additional diagnostic method prescribed to identify mucosal pathologies that are difficult to detect with conventional endoscopy.
Most often, chromogastroscopy is prescribed to detect benign and malignant tumors at an early stage of their development. Also, this technique is highly informative when it is necessary to determine clear boundaries of various neoplasms and degenerative lesions of the mucosa.
When performing chromogastroscopy, special dyes (methylene blue, Congo red, etc.) are sprayed onto the mucous membrane.
The affected areas of the mucosa are more intensely stained than normal mucosa, which allows for a more accurate (targeted biopsy).
Carrying out a brush biopsy
This type of biopsy is carried out in several successive stages - its essence is that the collection of biomaterial for examination is carried out from the source of pathology. Quite often, biomaterial is also taken during surgery. This is how you can achieve a double positive effect - on the one hand, there is treatment with the help of surgical intervention, on the other hand, a full diagnosis.
After the biomaterial is taken from the site of the pathological process, it is studied under microscopes. The collection of biomaterial itself as a process is controlled using special devices - a tomograph and an endoscope, as well as ultrasound and x-rays, which allows you to accurately insert the catheter, capture the biopath and remove the catheter.
When the biomaterial is extracted, it is sent for study, when in the laboratory it is pre-treated with special substances, which makes the sample solid. In this form, it is easier to examine it under a microscope, cutting it into thin plates.
21.01.2018
How to recover after a gastric biopsy
After the study, the patient should be under the supervision of a specialist for several hours. If there are no signs of bleeding, the patient is sent home.
Eating after a gastric biopsy is prohibited for 3-4 hours. Also, for three to four weeks you should stick to a light diet and avoid eating fatty, fried, spicy, etc. food.
Avoid drinking alcohol for at least two weeks.
After a gastric biopsy, it is not recommended to smoke (if possible for a day). You should also limit your intake of foods that increase gastric secretion (coffee, strong tea, marinade, pickles, sauerkraut, etc.) for several weeks.
Physical activity is excluded for a month.
It is necessary to limit emotional stress and avoid, if possible, stressful situations. If necessary, the doctor may prescribe mild sedatives.
Possible complications
Most often, after collecting the material, no traces remain. Rarely, slight bleeding occurs, but it resolves on its own and does not require additional medical attention.
Complications after gastric biopsy occur in less than 1% of patients
If after the biopsy the patient feels unwell, has nausea or vomits blood, then he needs to go to the hospital. Although the probability is extremely low, the following complications are still possible:
- damage to the stomach or esophagus (due to the motor activity of the subject during the procedure);
- development of septic shock;
- bleeding resulting from a rupture of a vessel when taking a biopsy;
- development of aspiration pneumonia. It develops when vomit enters the airways, causing infection. That is why the patient must breathe deeply through his nose and follow the specialist’s instructions.
When an infection occurs, the patient experiences fever and pain. Inflammation is accompanied by exudation. As a result of poor-quality manipulations, abrasions and swelling occur on the mucous membrane.
Implications of the study
This type of biopsy is a low-traumatic examination, so most often, a gastric biopsy does not have serious consequences.
The main consequence of the procedure is pain and sore throat after insertion of the endoscope. This effect goes away on its own within a few days.
In rare cases, discomfort in the epigastric region, nausea, and slight bloating are noted. It is also possible to experience minor bleeding that stops on its own.
In isolated cases, severe bleeding, inflammation of the gastric mucosa, aspiration pneumonia, gastric perforation, etc. may develop.
If these symptoms appear, indicating the development of serious complications, you should immediately call an ambulance:
- development of brown vomit, reminiscent of coffee grounds;
- the appearance of severe nausea and abdominal pain;
- addition of febrile symptoms, chills;
- difficulty breathing;
- chest pain, persistent cough;
- the appearance of blood in the stool (tarry black stools - melena).
Complications during gastrobiopsy
Careful preparation of the patient for the examination reduces the risk of complications. Sometimes unexpected situations happen.
Possible complications of gastric biopsy (rare in practice):
- acute bleeding from the sites where material was taken for gastric biopsy;
- perforation of a hollow organ;
- allergic reactions to the administration of anesthetic;
- damage to teeth.
Long-term complications after biopsy
Compliance with the rules for performing a biopsy minimizes the development of long-term complications. Most often, their occurrence is facilitated by concomitant pathology, anatomical and physiological characteristics of organs, and the degree of immune protection.
Adverse consequences include:
- systemic inflammatory response syndrome;
- inflammatory lesions of the proximal parts of the digestive tract, oral cavity;
- aspiration pneumonia;
- bleeding from an injured vessel.
Possible consequences of a biopsy
For several days after gastroscopy with histological examination, the patient may experience discomfort.
Does the stomach suffer when taking material?
Most often, the consequences of a gastric biopsy are heaviness in the abdomen, pain when swallowing and while eating, and the presence of black stool. Over the course of 3 days, moderately expressed unpleasant symptoms are not pathological and go away on their own after a few days. The mucous membranes of the organ are restored quickly due to their high reparative properties.
Carefully! If pain or bleeding worsens, you should consult a doctor immediately.
Stomach biopsy - interpretation of results
The interpretation of the tests should be carried out by the attending physician. Independent interpretation of the research results and subsequent self-medication are absolutely unacceptable.
In conclusion, the biopsy results indicate the following parameters:
- thickness of the gastric mucosa;
- cellular composition of the epithelium;
- level of secretory function of cells;
- the presence of atrophic changes, hypertrophy, etc.;
- presence of atypical cells;
- the presence of epithelial dysplasia and metaplasia;
- signs of the inflammatory process;
- Hh (the presence of HP on a gastric biopsy means the detection of Helicobacter pylori);
- degree of stomach contamination Hp (detection of Helicobacter during a gastric biopsy for an ulcer or gastritis indicates the Helicobacter nature of the mucosal lesion);
- the presence of lymphocytic cells, eosinophilic infiltrates, etc.
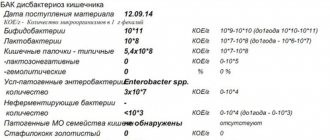
Results table
Also, with a gastric biopsy, a diagnosis is indicated based on morphological changes in the gastric mucosa.
In addition to the most common diagnoses such as Helicobacter pylori gastritis and ulcers, precancerous diseases and malignant neoplasms can be detected.
The table provides examples of histological precancerous diagnoses and their brief descriptions:
The price of the procedure depends on the region (in Moscow the study costs more than in the regions) and the number of biopsy samples. On average, the price for one biopsy ranges from 500 to 2000 rubles.
Similar articles:
- How is a pancreatic biopsy done, features of the procedure? A pancreatic biopsy is an important diagnostic test, since the pancreas...
- What is a biopsy? Its importance in diagnosis Biopsy is one of the instrumental diagnostic methods. Contemporary instrumental…
- How is a lung biopsy done, interpretation of the results? A lung biopsy is a diagnostic procedure that allows you to identify respiratory disease…
- Why and how a breast biopsy is performed Breast biopsy is the most reliable method of differential…