Causes
The mechanism by which this symptom occurs is based on the fact that hydrochloric acid irritates cough receptors located along the entire length of the respiratory tract, including those located in the upper sections.
A characteristic feature of such a cough, which occurs with gastric pathology, is that it is unproductive and also annoying. This is due to the fact that sputum is not produced. The occurrence of cough is purely due to chemical irritation of the receptors.
The most common is a combination of reflux esophagitis and cough. It is this pathology that causes coughing in most patients.
The main diseases of the digestive tract that are accompanied by this symptom are:
- Gastroesophageal reflux disease. This pathology is associated with impaired motility of the digestive tract. The development of gastroesophageal reflux disease occurs when the smooth muscles of the stomach contract improperly, and food moves not to the duodenum, but back to the esophagus.
- Hyperacid gastritis. This disease is associated with the proliferation of various areas of the mucous membrane on which special G cells are located. It is these cells that are responsible for the production of hydrochloric acid, which is the main component of gastric juice. This disease is characterized by heartburn and cough.
- Peptic ulcer disease. Almost always, peptic ulcer of the stomach and duodenum is accompanied by an increase in acidity.
- Esophagitis. A cough with esophagitis can appear regardless of food intake, which is the result of an inflammatory process.
- Duodenitis.
- Pathologies of the biliary tract or pancreas.
All these diseases are accompanied by increased acidity of the gastric environment. It is acids that are the etiological factor that leads to the appearance of the symptom.
It is worth noting that stomach cough does not appear in all patients. An important point is the presence of increased sensitivity of receptors to acids.
Cough as a symptom of gastroesophageal reflux disease
Reflux esophagitis is a disease caused by dysfunction of the stomach and esophagus. More often, the disease affects people with high acidity of digestive juice. With poor nutrition and abuse of acidic, salty, and spicy foods, constant irritation of the mucous membrane occurs. As a result, its surface becomes damaged, inflamed and swollen, and the lower esophageal sphincter loses its tone, beginning to leak gastric contents back into the esophagus.
More often, cough with reflux esophagitis appears as the first symptom and has its own characteristics. Cough is different:
- unproductivity (lack of sputum and relief);
- soreness in the larynx, similar to a sore throat;
- simultaneous belching during an attack with a sour taste, which is often confused with phlegm.
The nature of the cough differs depending on the form of gastroesophageal reflux, for example:
- in case of acute manifestation, the main symptom is paroxysmal, hammering, long-lasting, occurring immediately after eating;
- in case of a chronic illness, the symptom is quickly passing, but constant, accompanied by belching, especially after spicy and sour foods.
Additional signs are:
- chest pain;
- dyspnea;
- severe heartburn.
Symptoms
Each disease has its own time of cough onset. A cough with GERD appears immediately after eating, and with diseases of the stomach or duodenum - 1-2 hours after eating.
In addition, the cough may appear at night, regardless of food intake. This is due to the fact that in some diseases, gastric juice is produced even at night. This condition is extremely dangerous, as it can lead to the formation of ulcers. If ulcers have already been diagnosed, the risk of developing gastrointestinal bleeding or perforation of the ulcer increases significantly.
Interesting! Bitterness in the mouth and nausea: causes and prevention
A cough from the stomach has the following characteristics:
- Dry. With gastrointestinal pathology, the cough will always be unproductive.
- Nasty, not bringing relief. The duration of coughing attacks can reach an hour. The longest attacks occur at night.
- The appearance of bloody sputum. During prolonged attacks, a violation of the integrity of the bronchial mucosa may occur, which will lead to the release of a small amount of blood.
Additional symptoms and the treatment needed to get rid of them depend on the underlying pathology. This may be pain in various parts of the abdomen, dyspepsia (vomiting, bowel movements, nausea), belching, deterioration in general condition, increased body temperature.
In some cases, patients develop cough and heartburn after eating, which is considered an important diagnostic criterion.
The appearance of such a symptom requires contacting a medical institution, where a comprehensive examination and selection of etiotropic treatment will be carried out.
What will help reduce reflux?
After identifying the causes of stomach cough, dietary recommendations from specialists are prescribed to alleviate unpleasant symptoms:
- exclude alcohol and carbonated drinks;
- normalize body weight, which will reduce pressure inside the cavity and reduce the occurrence of reflux;
- avoid overeating, a single meal should not exceed 300-500 ml;
- It is better to boil or steam food;
- eat small meals 4-5 times a day;
- reduce consumption of fatty foods;
- limit salty and spicy foods, as such foods increase the production of acid and enzymes in the stomach;
- after eating, it is forbidden to take a horizontal position, reflux may follow into the esophagus, and you should also not bend over;
- Night sleep should take place at a slightly raised head of the bed, approximately at a level of 15-20 cm.
Can cough due to GERD be cured? If you follow these recommendations, your chances increase, but not always. When the pathology takes a serious form, even more stringent restrictions must be applied to nutrition. Many foods are excluded, food is consumed only in pureed form, the last meal should be 4 hours before bedtime.
Diagnostics
Diagnostic measures for a cough reflex against the background of gastric pathology are quite long, since when a cough occurs, attention is first paid to the respiratory system. Only in the absence of pathology of the lungs or bronchi, doctors pay attention to the digestive tract.
A set of diagnostic measures consists of those examination methods, the purpose of which is to identify the cause of its occurrence, as well as to exclude diseases of the respiratory system:
- General laboratory tests. Carrying out blood and urine tests almost always makes it possible to exclude respiratory pathology. The most important criterion in a general blood test is the level of leukocytes. In case of stomach diseases, the level of leukocytes will be normal, and pulmonary pathology is always accompanied by high leukocytosis.
- Biochemistry of blood. This test is performed to confirm diseases of the gallbladder and pancreas. The results of this analysis pay attention to the levels of bilirubin, amylase and alkaline phosphatase. These substances are always elevated during inflammatory processes of the gallbladder and pancreas.
- Plain radiography of the chest organs. This examination is carried out to exclude diseases of the respiratory system.
- Ultrasound of the abdominal organs. Thanks to ultrasound diagnostics, it is possible to identify pathologies of an inflammatory or non-inflammatory nature. Most often, ultrasound is performed if cholecystitis or pancreatitis is suspected.
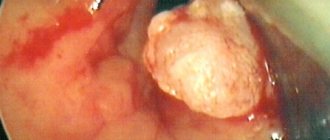
- Gastroscopy. Endoscopic methods are the basis for diagnosing diseases of the digestive tract. Using gastroscopy, you can visually assess the condition of the mucous membrane of the esophagus, stomach and duodenum. This examination requires special medication and psychological preparation.
Interesting! Quit smoking - heartburn appears: why does this happen?
- Duodenal sounding. Probing is carried out to assess the secretory function of the stomach, pancreas and gall bladder. The most common phenomenon that is diagnosed during such an examination is hyperfunction of the glandular cells of the stomach or insufficient amount of bile.
The duration of the examination for such symptoms can take a fairly long period of time due to the fact that cough is not a characteristic manifestation of pathology of the digestive tract.
During diagnosis, it is necessary to differentiate cough due to reflux with the following diseases:
- Asthmatic cough and bronchial asthma.
- Obstructive bronchitis.
- Damage to lung tissue.
The most important differential criterion is the absence of sputum. In addition, examination of the respiratory system does not reveal foci of inflammation in the bronchi and lungs.
Causes and consequences of prolonged cough
The protective role of coughing is that coughing movements remove phlegm and foreign particles from the respiratory tract. The most likely causes of cough are:
- infections affecting the respiratory tract;
- allergic diseases;
- respiratory tract tumors;
- aortic aneurysm compressing the bronchi;
- external factors of chemical irritation of the bronchi.
A severe, prolonged cough of any etiology leads to increased pressure in the chest, impaired circulation in the chest cavity and a decrease in the strength of heart contractions. Chronic cough weakens the elasticity of lung tissue and can lead to the development of emphysema.
Treatment
In order to get rid of such an unpleasant manifestation, treatment of stomach cough should be aimed directly at eliminating the disease that led to its occurrence. Thus, different groups of drugs can be used, depending on the pathology.
Antacids
Antacids are drugs that reduce acidity in the stomach. Today, there are two main types of antacids: absorbable and non-absorbable.
The mechanism of action of absorbed antacids is based on the fact that the active substance, entering the stomach, reacts with hydrochloric acid and neutralizes it. During this reaction, various chemical compounds are formed that can be absorbed into the blood.
This feature is the main disadvantage of such drugs, since long-term use can lead to intoxication of the body. But the main advantage of absorbable antacids is that they extremely quickly eliminate unpleasant symptoms, such as stomach cough or heartburn.
The most primitive remedy that belongs to this group is baking soda. The newest drugs in this class include Rennie, Bourget's mixture and magnesium carbonate. When they are used, the effect occurs after a few minutes, but its duration is insignificant.
The use of non-absorbable antacids is more relevant. Their effect occurs after a longer period of time, but the lasting effect lasts for several hours. The main representatives of this group are Maalox and Almagel.
The use of such drugs is practically safe, since their action is limited to the stomach cavity. The products of the chemical reaction, during which the acid is neutralized, are not absorbed into the blood. In addition, they have an enveloping effect, which protects the mucous membrane from the harmful effects of acid.
Interesting! Why does heartburn appear from sweets: the main reasons
The use of such drugs is permissible even during pregnancy and breastfeeding. They help get rid of not only cough due to GERD, but also heartburn.
Antibiotics
In some cases, stomach cough is a symptom of infectious diseases of the digestive system. In this case, broad-spectrum antibiotics or selective drugs should be used. The prescription of antibiotics requires the use of additional agents, the purpose of which is to protect the normal intestinal microflora, as well as the vagina.
For this purpose, live yoghurts and antifungal agents are prescribed.
In some cases, stomach cough needs to be treated promptly. Indications for surgery are for peptic ulcer disease, as well as for the development of complications.
Diet
The appearance of symptoms of stomach cough requires adherence to a diet, which helps reduce the likelihood of repeated attacks.
To do this, the patient should follow the following recommendations:
- Frequent meals in small portions. Thanks to this nutritional scheme, food will be located exclusively in the pyloric part of the stomach, which almost completely eliminates the risk of it refluxing into the esophagus. As a result, you can get rid of cough with reflux esophagitis without the use of medications.
- Refusal of sour, hot and spicy foods. These products significantly increase the acidity of gastric juice, which makes coughing attacks more pronounced.
- Eating food with an alkaline environment. This mainly includes drinks such as milk and soda mineral waters.
Healing with folk remedies
Is it possible to cure cough due to GERD using traditional methods? Witch doctors and healers shared some recipes to relieve unpleasant symptoms:
You will need flax seeds. A teaspoon of seeds is poured into a bowl (not metal), pour a glass of boiling water and simmer over low heat for 5 minutes. The dishes are set aside and wrapped for half an hour. After time, filter through cheesecloth. Drink warm, 1/3 cup 3 times a day.
- Treatment of cough due to GERD can be carried out using sea buckthorn or rosehip oil. You need to take it three times a day, a teaspoon.
- Collection of herbs. You will need 4 pinches of St. John's wort, 2 pinches each of calendula, licorice roots, plantain, calamus, one each of tansy and peppermint flowers. The herb is poured into an enamel bowl and everything is mixed. The collection is poured with a glass of boiling water, covered, wrapped and left for 30 minutes. After straining, take 1/3 cup warmed 3 times a day.
Prevention
In order to prevent the occurrence of cough in diseases of the digestive system, it is necessary to promptly diagnose and treat the underlying pathology.
Thanks to this, the risk of such a symptom occurring will be minimal. In addition, the patient will be provided with the most favorable outcome.
The appearance of cough in diseases of the stomach and lower esophagus is a rare occurrence. But it causes discomfort and inconvenience for patients. If you experience an unreasonable cough after eating, you should contact a gastroenterologist to undergo examination and begin treatment.
Reviews
Dear readers, your opinion is very important to us - therefore, we will be glad to hear your feedback about cough with reflux esophagitis in the comments, this will also be useful to other users of the site.
Karina : “My husband had a dry cough in the morning for a while, but during the day everything was fine. There were no other signs of a cold. The character is reminiscent of a smoker's cough, but my husband does not smoke. After a while he began to complain of heartburn and belching. These symptoms were treated and the cough disappeared.”
Elena : “With reflux esophagitis, the laryngeal mucosa is constantly irritated, and a cough may appear periodically. There is nothing dangerous or serious about this if you pay attention to the problem in a timely manner. I had to go on a diet for 2 weeks to normalize acidity, get rid of dry cough and other unpleasant symptoms.”
Dry barking-croaking cough for almost 3 months now. Throat, reflux, neurology???
Polina, Moscow
863 views
January 15, 2018
Hello! My 11-year-old son is tormented by a dry, prolonged cough, which gets worse in the evening and sharply worsens when lying down (only in the evening and at night; he can lie down normally during the day). Reminds me of the barking and cawing of a flock of crows. It’s impossible to fall asleep, it turns out somewhere in the morning. It hurts on the right and left under the ribs from this cough, sometimes coughing to the point of vomiting. Temperature 36.6. How we were treated and what diagnostics we carried out (we live in Italy, I apologize for the not very competent translation of terms): - in the emergency room they diagnosed laryngotracheitis and prescribed budesonide through an inhaler, which made the child cough even worse. - chest X-ray is good - examination by a pulmonologist: the bronchi are clean, throat cough - examination by an ENT specialist: nasal passages are free; the endoscope shows a foamy secretion deep in the throat; mucus flowing down the back wall; vocal cords are normal; mild hyperemia of the larynx; hypertrophy of nasal turbines. The diagnosis is chronic rhinopathy and posterior laryngitis, similar to reflux laryngitis. We have been seeing this (and not only) ENT specialist for a long time, the problem is constantly inflamed mucous membrane of the maxillary sinuses, frequent sinusitis, mucus running down the back wall. Adenoids of the 1st degree. The child has pyloric insufficiency, which is manifested by reflux, a burning sensation behind the sternum, a lump in the throat, sometimes followed by abdominal pain. This happens a couple of times a year. We try to follow the diet and recommendations for reflux. It should be noted that a couple of weeks before the onset of this cough, we stopped taking antacids after another exacerbation of reflux and abdominal pain. Painful sensations in the depths of the throat, a lump in the throat and a burning sensation under the throat - yes, such symptoms existed and still remain. The ENT prescribed: antacids, nasal rinsing, flixonase throat spray (instead of budesonide through an inhaler, because cold inhalation is not good for dry coughs), steam inhalations with a sedative additive based on calcium, soda and glycerin (and not with eucalyptus essential oil, as I did, and it was the only thing that gave a short-lived, but effective effect). 10 days of therapy did not produce any effect. Or rather, it seemed better for a couple of days, then they returned to their original state again. - blood test (lymphocytes, ESR, reactive protein, IgE, candida, aspergillus) - everything is excellent, only eosinophils 5.2%. Antibodies for whooping cough are also normal, however, the child was last vaccinated against it when he was 5 years old. - Erespal was reported from Russia (it is prohibited here) - my son began to vomit 15 times a day, both from syrup and tablets, and even on minimal doses. On the 4th day they stopped taking the drug. - the district pediatrician diagnosed laryngotracheitis, prescribed a mucolytic (at that time we had been drinking them for 2 months already: mucaltin, cough medicine, fluimucil, bromhexine), the sedative levodopropizine (we had already taken Stoptussin drops without effect and even tried codeine 2 times - no effect) , a budesonide inhaler and, as a last option, clarithromycin. The budesonide inhaler immediately made him choke and choke, but they didn’t stop. We started antibiotics. There was no improvement, but on the 4th day the cough stopped! True, there was such a nuance: I went with my youngest to the skating rink, but he also really wanted to. But he was offered a quiet walk with his dad, to which the child buried himself in the blanket, protested and freaked out. They waved their hand, it still doesn’t get better at home in the warmth, and took him to the skating rink. From that moment on he stopped coughing. There were sporadic coughs until the evening, and then suddenly it was cut off. We finished the antibiotic for a week, but we didn’t know that it had helped. A week later he started coughing a little again, we went into the snow and cold, and there his cough returned. - they took a swab from the throat - it was clear - the pediatrician was surprised and again prescribed an antibiotic, since for some reason it helped, this time azithromycin for 5 days. Today I took the last pill, no results. She also prescribed me to take cortisone tablets along with the antibiotic (I did not give them) and a budesonide inhaler. It was possible to make an inhaler not with a mask, but with an insert for the mouth, but my son began to vomit during or immediately after these inhalations. We stopped. We hoped for an antibiotic, but it didn’t help either. The child is emotional and complex, and we cannot rule out a nervous cough. With very strong positive arousal, the cough decreases significantly and subsides. But if you leave him alone in front of the computer to watch and do what he wants and not touch him, then he will still cough, no matter how keen he is on a pleasant activity. The child has been experiencing constant headaches in the forehead area (24 hours a day) of greater or lesser intensity for 4 years. They examined everything up and down, stopping at the chronically inflamed nasal sinuses (heavily thickened mucous membrane along the entire contour). The ENT specialist continues to believe that the nature of the cough is reflux. But 10 days of therapy with antacids, cortisone and steam inhalations did not improve the condition at all. The pediatrician said that he should suppress his cough by pinching his nose and exhaling weakly through his mouth, but he does not strain himself with this at all. On the contrary, he relaxes, opens his mouth and coughs with all his might. I explain that a lot depends on a person’s will and attitude, but my words apparently don’t get through. I’ll also add that the onset of this cough was preceded by a small cold and a couple of weeks of the usual dry cough, which I write about below. For 2 years now, sometimes for 10-14 days he develops a dry cough before going to bed, which is not thinned by mucolytics. But he was never a barker, he just coughed dryly, unproductively, without coughing, and that was all. This happened once every 2-3 months. In May, the cough became stronger (but just dry, not barking) and there was a tingling and burning sensation in the area of the lungs (not reflux, we know it well), it was painful to inhale deeply. X-ray and cardiogram were normal, 2 pulmonologists found nothing. Spirometry is normal. Allergy tests have been taken 2 times over the past 4 years. After a couple of weeks, everything went away, maybe the heat helped, or maybe albendazole (I stayed in the toilet for a long time, had suspicious stools, had pain in my lower abdomen here and there... we already had experience with such symptoms). We don’t know what to tie to what and what to do next. I’m not asking you for a diagnosis, I would like to know your versions and conclusions, as well as what tests and what diagnostics to undergo? If something was coughed up, you could collect it in a jar and send it to the laboratory, but here everything is dry... Thank you in advance!
The question is closed