The number of people who suffer from diseases of the digestive tract is growing every year around the world. Focal atrophy of the gastric mucosa is a pathology that leads to the death of the glands that are responsible for the production of gastric juice. With this type of atrophy, disorders that occur in the mucous membrane are pathologically progressive. The insidiousness of this disease lies in the ability of cells in the affected areas to degenerate into malignant ones. Therefore, experts classify focal atrophy as a precancerous condition.
Below we consider the symptoms and treatment of atrophic gastritis.
Reasons for the development of the disease
Another name for this pathology is atrophic gastritis of a chronic nature. According to statistics, people of retirement age are most susceptible to this disease. Citizens aged 18 to 35 years old get sick much less often. The provoking factor in this situation is autoimmune diseases, when, due to a malfunction, the immune system begins to kill its own tissues and cells. Such a target may be the stomach and its internal membranes.
Most often, focal atrophy of the gastric mucosa develops after 50–60 years, as a result of gastritis caused by the bacteria Helicobacter pylori.
The main reasons contributing to the development of the disease are quite diverse. These include:
- Poor nutrition is the most common factor affecting the condition of the gastric walls. A person who has been eating fast food, spicy, and fatty foods for many years causes a blow to this main digestive organ. Fasting, constant dieting, failure to observe time intervals between meals negatively affect the state of the gastrointestinal tract. What are other causes of atrophy of the gastric mucosa?
- Bad habits (smoking and drinking alcohol) disrupt the normal rhythm of the digestive system, causing an inflammatory process in the mucous membrane, the formation of ulcers and erosions.
- Prolonged uncontrolled use of medications. Many modern pharmacological preparations may contain chemicals that have a detrimental effect on the inner lining of the stomach and organs of the entire digestive tract.
- Intoxication. When dangerous chemicals or natural substances penetrate into the body, irritation and, as a result, inflammation of the gastrointestinal tract occurs.
- Hereditary factor. Experts say that gastritis, which is inherited, is dangerous with a high probability of degeneration into an oncological tumor.
- Frequent stress and nervous shock can cause disruption of the normal functioning of the digestive system, provoking the occurrence of irreversible disorders.
- Some somatic pathologies (diabetes mellitus, diseases of the cardiovascular system) significantly increase the risk of atrophic disorders.
- Lack of iron and vitamin B12 affects the condition of the digestive organs, disrupting their activity.
Signs of atrophy of the mucous layer in gynecology
Atrophy of the mucous membrane (in gynecology, treatment, as with any disease, is carried out only after identifying the cause and the nature of the severity of symptoms) at the initial stage can occur without symptoms.
In advanced form, the following symptoms may be observed:
- dryness in the vaginal mucosa even during intimacy;
- pain during sexual intercourse;
- presence of curdled discharge with an unpleasant odor;
- frequent urination;
- discomfort in the vagina accompanied by itching and burning;
- presence of bloody discharge after sex. Blood occurs due to damage to the capillaries due to lack of lubrication;
- the process of intimate hygiene (washing), as well as urination, may be accompanied by burning and pain;
- nagging pain in the lower abdomen, which can extend to the lumbar region and limbs;
- frequent inflammatory processes in the genitourinary system;
- reduction of vegetation on the external genitalia;
- Upon visual examination, increased folding of the vaginal walls and their prolapse are noted.
In severely advanced forms, spontaneous urination is possible. Also a decrease in a woman’s sexual desire and activity.
Classification
This disease has a specific classification:
- Focal atrophy of the gastric mucosa is characterized by the appearance of pathological foci in the connective tissue in place of the dead glands of the inner lining. The lesions have different sizes and shapes; their morphological structure and appearance resemble an atrophic scar on the skin of the face - a pink, flabby area with noticeable borders. Focal atrophy is dangerous because there are often no symptoms during its development.
- Focal atrophy of the mucous membrane of the antrum of the stomach is a type of pathological process that is characterized by damage to the distal part of the stomach and the death of the glands responsible for the production of hydrochloric acid and pepsin. As a result, the walls of the stomach begin to become inflamed. With an old course, bacterial damage and the development of ulcers may occur.
- Moderate atrophy, which can be mild, severe and moderate. A weak one is characterized by a slight change in the main glands. For moderate, negative measurements are more significant, in addition, the formation of pathological areas is observed. Severe atrophy is characterized by extensive necrotic lesions.
Symptoms
Superficial atrophy of the antrum of the stomach often occurs without any signs. When the glands are still coping with their functions, a person is bothered by heartburn and moderate pain after eating. This is due to increased production of hydrochloric acid. Signs of gastritis that indicate atrophy of the glands:
- increased gas formation;
- constant rumbling in the stomach;
- chronic stool disorder;
- bad breath;
- thick white coating on the tongue;
- frequent poisoning.
The hyperplastic form of the disease is characterized by sudden weight loss and lack of appetite.
Since the absorption of vitamins and minerals is impaired, a person’s immunity weakens. The disease is recognized by external changes: pale skin, brittle nails, increased hair loss.
With atrophic antral gastritis, a person quickly becomes full. Even after a snack, heaviness appears in the stomach. Intoxication can be caused by foods that do not cause a negative reaction in other people. Exacerbations are also caused by medications, heavy foods, and alcohol.
Focal atrophic gastritis is often complicated by concomitant diseases - cholecystitis, pancreatitis. The patient develops intolerance to dairy products and eggs. Their smell can cause nausea and dizziness.
With esudative atrophic gastritis, fluid accumulates at the site of inflammation. The formed elements are filled with blood particles. Symptoms of the esudative (eosinophilic) form of gastritis:
- pain and burning in the stomach;
- belching with a putrid odor;
- general weakness;
- weight loss;
- the urge to stool after every meal.
Clinical signs of antral atrophy include pale mucous membrane with capillary lumens. The epithelium is dense in places with wide gastric pits. Total atrophy leads to a decrease in the size of the organ.
Symptoms
The symptoms of focal atrophic lesions are blurred and rather weakly expressed, so in the early stages of the disease patients are not aware of its existence.
Classic symptoms of focal atrophy of the gastric mucosa differ in the degree of intensity and severity:
- Nausea occurs. If this phenomenon occurs frequently and without objective reasons, it may indicate inflammatory processes.
- Changing the stool. Diarrhea or constipation are a sign of a violation of the full process of digestion of food, malfunctions of the intestines.
- Unpleasant sensations in the stomach. After eating, patients complain of a feeling of heaviness, fullness, and pressure in the epigastric region. For this reason, patients suffering from focal atrophy eat poorly and quickly lose weight.
- Flatulence. With mucosal atrophy, food is poorly digested, its remains decompose, which leads to increased gas formation.
- Belching, which is a sign of insufficient production of gastric juice to break down food. There is belching with an unpleasant odor and bitterness. Some patients complain of dry mouth and an unpleasant taste.
- Pain syndrome. Pain in focal atrophic lesions is dull, intermittent, and occurs after eating. In advanced cases, the pain is permanent.
- The appearance of a white coating on the tongue, which is most typical during exacerbations of the disease.
- Weight loss, which occurs due to a weakened general condition of the body and insufficient absorption of food.
The periodic occurrence of 2-3 of the above symptoms should be cause for concern and contact a gastroenterologist.
Treatment
Therapy for mucosal atrophy is aimed not only at eliminating the cause (that is, normalizing estrogen production), but also at eliminating accompanying symptoms (dryness, burning, pain). Depending on the degree of damage to the vagina, treatment may consist of taking hormonal drugs orally, using suppositories or complex therapy (especially if an infection is attached).
Hormone replacement therapy
Since atrophy of the vaginal mucosa develops due to a lack of estrogen, the basis of treatment (especially in advanced form) is the use of hormones. Therapy with this type of drug takes a long time (possibly up to 5 years). After discontinuation of medications, a relapse of the disease is possible.
List of hormonal medications used:
| Drug names | a brief description of |
| Aktivel | The tablets are prescribed to women one year after the cessation of menstruation. Treatment is carried out by taking 1 tablet of the drug daily, without breaks. |
| Angelique | The drug is used for therapy in women from menopause. Therapy consists of taking 1 tablet daily. A break in the use of the drug is unacceptable. |
| Davina | The tablets must be taken for 21 days followed by a 7-day break. The drug is often prescribed to women of climatic age. |
| Individual | The drug is prescribed from the onset of menopause. Treatment consists of taking 1 tablet daily, without breaks. |
| Climodien | Taking the pills is recommended for women during menopause. Therapy is carried out by taking 1 tablet at one time daily. After the end of the medicine in the package, continued administration from a new plate is required. A break between taking pills is unacceptable. |
| Cliogest | |
| Pauzogest | Tablets are prescribed one year after the cessation of menstruation. The tablets are taken without interruption at one time. |
The choice of medication is made by the attending physician.
Before prescribing them, the gynecologist must exclude contraindications:
- the presence of oncological formations in the reproductive organs and mammary glands;
- increased blood clotting or blood viscosity;
- liver or kidney diseases in the acute stage;
- high blood pressure;
- presence of bleeding from the vagina of unknown origin;
- diseases of the cardiovascular system.
If there are contraindications, the gynecologist prescribes non-hormonal drugs.
Drug therapy
Drug, non-hormonal therapy for mucosal atrophy can achieve the following results:
- restoration of hormone production;
- normalization of metabolic processes;
- protection against infection.
Drugs used in drug therapy:
| Type of medicine | Purpose of application | Names of drugs |
| Immunomodulatory | Help strengthen the immune system and reduce the likelihood of further development of mucosal atrophy. Additionally, tissue restoration occurs. |
|
| Vitamin complexes |
| |
| Phytoestrogens | The drugs help compensate for the lack of estrogen. They have a natural base. |
|
Non-hormonal therapy has low effectiveness, so it is more often used in complex treatment or at the onset of pathology development.
Vaginal suppositories, ointments
Products for vaginal use are prescribed in complex therapy. They help restore microflora in the vagina, eliminate dryness and accelerate the healing of microcracks and wounds in the mucous membrane.
List of vaginal products used:
| Names of funds | Production form | Application nuances |
| Miramistin | The drugs are used to prepare solutions for douching. The products prevent the development of infections and accelerate the restoration of the vaginal mucosa. | Procedures should be carried out in the morning and evening hours, after performing hygiene procedures. |
| Furacilin | ||
| Rivanol | ||
| Ovestin | Vaginal suppositories, creams or ointments help restore hormonal balance, normalize microflora and prevent the development of infections. | It is recommended to use the drugs in the evening for better absorption and absorption by the vaginal mucosa. |
| Estriol | ||
| Estrocade | ||
| Bifidumbacterin | Suppositories can eliminate dryness and normalize the microflora in the vagina. | |
| lactobacterin | ||
| Vagilak |
This therapy may be accompanied by irritation of the vaginal mucosa and local manifestation of an allergic reaction. The type of drug is determined by the gynecologist.
Are antibiotics needed?
For mucosal atrophy, antibiotics are used only when a bacterial infection occurs in the vagina or urinary system. In other cases, antibiotic therapy is not used.
To eliminate complications caused by bacterial activity, the following are used:
- Amoxicillin;
- Ceftriaxone;
- Azithromycin;
- Ampicillin;
- Ofloxacin.
Complications can also be caused by the addition of a fungal infection. In this case, antifungal medications are used (Clotrimazole, Miconazole, Terzhinan).
Erythematous gastropathy with focal atrophy of the gastric mucosa
Erythematous gastropathy refers to redness of the gastric mucosa, which may be accompanied by swelling, bleeding and excessive mucus production. A similar sign is determined when examining the stomach using an endoscope - fibroesophagogastroduodenoscopy.
Hyperemia of the mucous layers of the stomach is provoked by some unfavorable factors, for example, spicy, rough and too hot foods. Under the influence of the causative factor, microcirculation is activated in the affected areas of the stomach, which gives it a bright red color.
Not everyone knows what atrophy of the gastric mucosa is.
Varieties
Otorhinolaryngologists identify several types of diseases in which mucosal atrophy is noted:
- Atrophic rhinitis is a condition characterized by a sensation of a foreign body in the nose, scanty viscous mucous discharge and rare nosebleeds.
- Subatrophic rhinitis is a disease without obvious signs. It can only be recognized by the fact that crusts constantly form in the nose, and the mucous membrane feels rough to the touch.
- Ozena is a serious condition in which necrosis of the mucous membranes is noted. At the same time, a large amount of foul-smelling mucus is released from the nose. The patient constantly feels nasal congestion, his sense of smell is reduced, and yellow-green crusts constantly form in the nose.
- Infectious rhinitis is a disease in which an infection is associated with mucosal atrophy.
Treatment of atrophic rhinitis and its other varieties depends on the symptoms. These types have varying degrees of severity, so the appropriate therapy is selected.
Main difference
A distinctive feature of this symptom of the disease is that it directly affects the mucous layer of the organ, while the deeper layers remain intact.
Most often, a similar syndrome can be observed when performing FEGDS in patients with erythematous gastritis. In this clinical case, it is necessary to take therapeutic measures in a timely manner, since the course and outcome of the disease depend on the adequacy and timeliness of therapeutic measures. Incorrect or late treatment threatens the transition of the pathological process to a gastric ulcer.
If erythema is detected in the stomach, the doctor may recommend some additional studies, the purpose of which is to identify Helicobacter pylori, as well as determine the pH of gastric juice or conduct a biopsy of the affected areas of the mucous membrane, followed by histological examination.
In almost every case, erythematous gastropathy is detected accidentally during FEGDS, which is carried out during the diagnosis of other diseases or for preventive purposes.
It is important to recognize signs of focal atrophy of the gastric mucosa in a timely manner.
Diet and recommendations for antral gastritis
For successful treatment, diet is very important for patients with antral gastritis.
In case of exacerbations of the disease and increased levels of gastric acidity, diet No. 1 is prescribed with a strict prohibition of fried, fatty, spicy, raw vegetables, sour fruits and berries. Before improvement, beans and mushrooms, fresh bread and pastries, confectionery, chocolate and coffee are also excluded.
What can prevent the development of antral gastritis? Doctors advise:
- reduce consumption of red meat, hot peppers, fatty and sweet foods;
- eat food at regular intervals, the last meal should be two hours before bedtime;
- eat in small portions, chew food slowly and well;
- Do not drink water during meals, as this may slow down the digestion process;
- Drink green tea and plenty of water regularly throughout the day.
An accurate prognosis for the development of gastroenterological diseases is hardly possible, and - taking into account the causes, type, degree of atrophy of the gastric mucosa, and the body's response to treatment - the doctor can assume how antral gastritis behaves in each specific case.
Predisposing factors
To treat pathology, you need to know what causes it. Predisposing factors include:
- Unhealthy eating. Abuse of fried, spicy, salty foods contributes to the occurrence of erythema in the stomach. Fast food, smoked foods, soda and hot drinks also negatively affect the gastric mucosa.
- The use of medications from such categories as non-steroidal anti-inflammatory, antibacterial, hormonal, anticoagulant and others.
- Infectious invasion. It is necessary to note the negative impact on the organ of the bacterium Helicobacter pylori, as well as fungi and staphylococci.
- Reflux of intestinal contents into the stomach cavity.
- Irritation of the mucous layer with hydrochloric acid during dieting or fasting.
- Chronic stress.
- Increased physical activity.
- Insufficient sleep.
- Alcohol abuse and smoking.
- Changes in metabolism.
- Hormonal imbalance.
- Hereditary predisposition.
- Pathologies of internal organs, for example, inflammation of the pancreas, intestines, gall bladder and others.
- Vascular atherosclerosis.
- Exposure to food allergens and chemicals.
Are blood, urine and stool tests necessary?
Characteristics of the atrophy process
The most common location for atrophy of the gastric mucosa is the lower third of the body or the antrum. One of the main damaging factors is considered to be Helicobacter, which lives closer to the pyloric zone.
At the initial stage, glandular (goblet) cells produce hydrochloric acid even in excess. Perhaps this process is associated with the stimulating effect of the bacterial enzyme system.
Then the synthesis of gastric juice is replaced by mucus, and the acidity gradually decreases.
By this time, the protective role of the mucous membrane is lost. Any food chemicals can harm the cells lining the inside of the stomach. Toxic products and remnants of destroyed cells become foreign to the body.
The autoimmune mechanism is involved in the destruction process. Antibodies are produced against damaged cells, which continue to fight their own epithelium. Blocking recovery processes plays an important role.
In a healthy stomach, the epithelial layer is completely renewed every 6 days. Here, old dysfunctional cells remain in place or they are replaced with connective tissue.
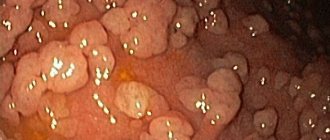
On histology, instead of clear outlines of the epithelium (look along the upper edge), destroyed cells are visible, there are no pyriform glands
In any case, the atrophied mucosa cannot replace gastric juice with mucus. There is a gradual thinning of the stomach wall. In practice, the organ is excluded from digestion, and gastrin production increases. The bolus of food enters the small intestine unprepared, which leads to failure of other successive stages.
The process doesn't end there. The most dangerous period of atrophic changes begins: the epithelium begins to produce similar, but not true, cells. Most often they can be classified as intestinal. They are not able to produce gastric secretions. This process is called metaplasia and dysplasia (transformation), and precedes cancerous degeneration.
Atrophied areas on the mucous membrane cannot be completely restored, but with the help of treatment there is still a chance to support the remaining functioning cells, compensate for the lack of gastric juice and prevent disruption of the overall digestive process.
Diagnostic measures
If you suspect focal atrophic gastritis, you should contact a gastroenterologist. The specialist collects anamnesis, finds out the patient’s complaints, and the intensity of symptoms.
Diagnosis of atrophy of the gastric mucosa should be comprehensive:
- Detailed and general blood tests, urine tests with determination of protein volume, leukocytes.
- A coprogram, which is a stool test showing how much food is digested and how nutrients are absorbed.
How much stool is needed for analysis? This is indicated by the attending physician when writing a referral. In addition, the following studies are being conducted:
- For the presence of Helicobacter pylori infection - breathing tests, morphological techniques.
- Using an endoscope is a reliable technique that allows you to visually assess the severity and type of atrophic lesions.
- Biopsy of stomach tissue, histological studies, which allow us to determine the stage of morphological changes in the mucous membrane.
- Ultrasound of the liver and pancreas, since with atrophic lesions of a focal nature, their activity may be impaired.
How much stool is needed for analysis in a child, infants and adults? The measure will be almost the same. To do this, use a special sterile container, which can be purchased at the pharmacy. It is sealed and the set includes a spoon. There are marks on the container.
The volume of feces for adults will be no more than the size of a walnut. 15 grams of formed stool is enough to collect for a child.
How to treat atrophy of the gastric mucosa?
Therapeutic measures
Properly prescribed treatment for focal atrophic gastritis can significantly improve the patient’s condition. To cure and restore the mucous layers of the stomach is the main goal of such therapy, the effectiveness of which directly depends on the reasons that provoked the development of this disease.
If the pathology has developed against the background of Helicobacter pylori infection, inhibitors and antibacterial drugs are prescribed. A one-week therapeutic course is usually sufficient to destroy this bacterium.
The main groups of medications used in the treatment of focal atrophic lesions:
- Replacement medications (natural gastric juice) and digestive enzymes (Pangrol, Creon, Mikrazim), which help to fully digest food.
- Medications that help produce hydrochloric acid. For example, thanks to the use of Plantaglucid, the process of gastric secretion is enhanced, inflammatory manifestations and spasms are relieved.
- Vitamins in tablet or injection form are prescribed when the level of hemoglobin and serum iron (vitamin B12) decreases.
- Painkillers, such as No-Spa or Buscopan, are good for eliminating pain and spasms.
- Medicines that improve the motility of the digestive tract - Cerucal, Motilium. They help move the food lump through the stomach to the intestines, preventing the development of stagnation.
In advanced cases of the disease and precancerous conditions, therapy through surgical intervention is indicated.
Treatment of atrophic gastritis of the antrum of the stomach
Expert opinion
Irina Vasilievna
Practicing gastroenterologist
Treatment of antral atrophic gastritis is a multi-stage and lengthy process . The final treatment of the disease depends on the stage of atrophy, as well as on the form of disturbance of gastric secretion.
Often, with atrophic gastritis, the production of hydrochloric acid is completely absent. In these situations, replacement therapy is prescribed, which can last a long time, sometimes throughout life.
Treatment is prescribed on an individual basis and usually includes the following points:
- Drug therapy is the main and most effective method of treating atrophic antrum gastritis.
- Diet therapy , based on the principles of sparing the stomach, is a prerequisite for successful treatment, complementing the main therapy.
- Replacement and stimulating therapy is prescribed outside the period of exacerbations.
- Herbal medicine has proven effectiveness in the diagnosis of “atrophic gastritis” and can successfully complement the main treatment.
- Physiotherapy - magnetic therapy and electrotherapy, electrophoresis with medications, thermal procedures for the epigastric region.
- Sanatorium-resort treatment is prescribed outside the period of exacerbations.
Treatment is prescribed only by a doctor - a therapist or gastroenterologist! It is better to try to get an appointment with a gastroenterologist.
What do doctors usually prescribe?
Treatment of atrophic antrum gastritis is carried out with the following drugs (the combination and dosage of which is prescribed by the doctor):
- Antibiotics (if Helicobacter pylori infection is detected) - a treatment regimen using two different antibiotics is usually used, for example, Metronidazole + Amoxicillin.
- Proton pump inhibitors (at gastric pH <6) - Omeprazole, Rabeprazole.
- Glucocorticosteroids are prescribed only for autoimmune gastritis and severe vitamin B12 deficiency.
- Enveloping and astringent agents – “Phosphalugel”, “Almagel”, “De-nol”, “Vikalin”.
- Replacement therapy drugs - natural gastric juice, Acidin-Pepsin, Abomin.
- Stimulating therapy means - "Limontar", mineral waters (Essentuki No. 4, 17), rosehip decoction, medicinal mixtures (plantain, St. John's wort, thyme, wormwood).
- Enzymatic preparations – “Festal”, “Creon”, “Mezim”.
- Gastroprotectors – “Sucralfate”, “Solcoseryl”.
- Antispasmodics - “No-shpa”, “Drotaverine”.
- Anticholinergics - “Gastrocepin”, “Platifillin”.
- Drugs that stimulate gastric motility - Trimedat.
- Vitamins.
- Iron supplements.
Folk remedies
Folk remedies for the treatment of atrophic gastritis of the antrum of the stomach will be a good addition to drug treatment, but their use must be agreed with a doctor. Popular recipes:
- Rose hip decoction. 2 tbsp. spoons of crushed rose hips should be poured into 250 ml. boiling water and 10 min. simmer over low heat. Let the broth brew for 2-3 hours. Drink 75 ml of the product. half an hour before meals for a month, then take a week's break and repeat the course.
- Aloe juice and natural honey. The ingredients should be mixed in equal proportions and taken 1 teaspoon before each meal. The course of treatment is 2-3 weeks.
- Oatmeal infusion . 2 tbsp. I pour 400 ml of oat flakes crushed into powder. boiling water and let it brew in a thermos for 4-5 hours. The resulting infusion is filtered and taken ½ glass half an hour before meals twice a day. The course of treatment is 1 month.
- Fruit and vegetable juices (cabbage, tomato, lemon juice). Freshly squeezed juices are diluted with warm boiled water in a 1:1 ratio and taken before or during meals in small portions.
On our website: Autoimmune gastritis - symptoms, treatment and diet
Diet and menu
During the period of exacerbation, patients with atrophic gastritis are prescribed diet No. 1a. This diet puts minimal stress on digestion.
- Products that irritate damaged mucous membranes are excluded from the patient’s menu.
- The food is served as a warm liquid or puree.
- Dishes should be steamed or boiled and thoroughly chopped.
- The diet menu consists of slimy soups and porridges, steamed cutlets, soufflés, omelettes, purees, and jelly.
Expert opinion
Irina Vasilievna
Practicing gastroenterologist
Diet No. 1 is prescribed after acute symptoms subside : it helps to normalize the secretory and motor functions of the stomach. The diet is considered balanced in terms of protein, fat, carbohydrates, and calorie content.
Dishes are steamed, boiled, stewed or baked without forming a crust. Served pureed or not pureed (at the last stage of treatment).
Allowed to use:
- dried white bread, dry cookies;
- vegetable or cereal puree soups;
- milk porridge;
- boiled/steamed meat and fish;
- low-fat dairy and fermented milk products;
- vegetables (potatoes, carrots, beets, zucchini, cauliflower);
- baked fruits;
- jellies, mousses, jellies, compotes;
- honey, sour jam, marshmallows, marshmallows.
On our website: Methods and complex of exercise therapy for gastritis
For atrophic gastritis, the main one is diet No. 2 - rational therapeutic nutrition, providing the body with all the substances necessary for its normal functioning.
Recommended dishes are steamed, boiled, stewed, baked without forming a crust. Only those dishes that have a rough structure are subject to complete rubbing. Recommended:
- dried white bread, dry cookies, biscuits;
- soups with the addition of cereals and vegetables in weak meat, fish or vegetable broths;
- porridge (except pearl barley and millet) in water with the addition of milk;
- boiled/stewed meat and fish;
- dairy and fermented milk products, including cheese and cottage cheese;
- soft-boiled eggs, omelettes;
- vegetables (white and cauliflower cabbage, pumpkin, carrots, beets, potatoes, zucchini);
- pureed ripe sweet fruits, mousses, jellies;
- rosehip decoction, diluted juices, tea with lemon;
- honey, jam, jam, marmalade, marshmallow, marshmallow, soft toffee.
At all stages of treatment, the following are prohibited: fatty foods, smoked foods, canned food, salted and pickled foods, legumes, baked goods, sour berries and fruits, chocolate, coffee, ice cream, soda.
Nutritional Features
Diet plays a very important role in the treatment of focal atrophic gastritis. The basic principle is gentle, fractional nutrition. It is preferable to steam food. You should not eat food that is too hot or cold, which will injure the walls of the organ. The basis of the diet should be:
- Soups with low-fat broths.
- Thoroughly pureed vegetable puree.
- Boiled meat (rabbit, beef, turkey), white fish.
- White dried bread (yesterday's).
- Oatmeal, rice porridge.
- Compotes from dried fruits, non-carbonated mineral.
Fatty foods, canned food, foods with vinegar and spices, carbonated drinks, and artificial juices are prohibited.
Prevention
Taking good care of the digestive organs allows you to maintain health for many years. For people who have relatives with diseases of the digestive tract, compliance with preventive measures is necessary.
Proper nutrition is the key to health and well-being. Eliminating junk food significantly reduces the load on the stomach, allowing you to preserve secretory functions. Giving up bad habits also allows you to minimize the negative effects of harmful substances on the mucous membranes of the stomach.
The presence of past diseases (colitis, duodenitis) is a reason for regular monitoring of the condition of the gastrointestinal tract. People suffering from gastritis should undergo a diagnostic examination annually.
We looked at the symptoms and treatment of atrophic gastritis.
Precancerous changes in the gastric mucosa
Oncological disease of the stomach is a common pathology of the digestive system of the body, which causes a significant percentage of death. This malignant process occurs in the pathologically altered mucous membrane of the organ, which is preceded by precancerous diseases of the stomach. These diseases of the gastric organ, which are acquired or, in rare cases, congenital in nature, precede the oncological process, but do not always develop into cancer.
According to statistics, gastric cancer most often develops at the age of 40-70 years and is much more common in men than in women. The pathology against which a malignant process develops does not always have severe symptoms and a long course. Therefore, the degeneration of a benign tumor into a cancerous tumor, for the most part, goes unnoticed. This explains why patients seek help late, resulting in a significantly reduced positive prognosis for life and its quality.
Precancerous conditions of the stomach are pathologies, which include the following diseases.
Precancerous conditions of the stomach are pathologies, which include the following diseases:
- Gastritis with decreased secretory function is most often atrophic gastritis, which is characterized by heaviness in the stomach, flatulence, belching with an unpleasant odor, and intestinal dysfunction in the form of frequent constipation, alternating with diarrhea. Pain syndrome is present, but it is mildly expressed.
- Gastritis with increased secretory function - manifested by frequent heartburn, severe pain in the stomach, especially on an empty stomach or at night, when hydrochloric acid acts aggressively on the empty organ. Vomiting with mucus and bile is possible after eating.
- Stomach ulcer - a pathological process accompanied by “hungry” pain, nausea, vomiting with the presence of mucus and sometimes streaks of blood in the vomit, decreased appetite, and flatulence.
- Polyps are benign formations of a hyperplastic or adenomatous type, capable of malignancy, which are localized on the wall of the stomach. With their small size, clinical symptoms do not appear or manifestations of gastritis occur. With an increase in the volume of pathology, bleeding, cramping abdominal pain, severity and difficulty in evacuating the bolus of food into the duodenum may occur.
As a rule, the reasons for the development of gastric precancer can be very different. In this case, external factors that contribute to the occurrence of this pathology play a major role. These are an unbalanced diet, alcohol abuse, work in hazardous industries, chronic stress, the presence of Helicobacter pylori, long-term use of anti-inflammatory non-steroidal medications ( Aspirin, Diclofenac ).
But the reason for the degeneration of a benign process into a malignant formation has not yet been clarified.
Sources
https://tsito logiya.su/zheludok/ochagovaja-atrofija-slizistoj-zheludka-chto-jeto
https://gastritlechim .ru/bolezni-pishhevoda/kakie-simptomy-u-vospaleniya-slizistoj-obolochki-zheludka-kak-ix-lechit.html
https://zhivot -info.ru/vospalenie-slizistoy-zheludka
https://tsitologiya .su/zheludok/ochagovaja-atrofija-slizistoj-zheludka-chto-jeto