Metastases are secondary foci in various organs, the result of the spread of a malignant tumor in the body. According to statistics, about 53% of patients with pancreatic cancer already have distant metastases at the time of diagnosis.
- Features of metastasis in pancreatic cancer
- Where do pancreatic malignant tumors most often metastasize?
- What are the dangers of metastases in pancreatic cancer? Possible complications
- Modern diagnostic methods
- Treatment of pancreatic cancer with metastases
- Forecast
It is difficult to fight such an advanced disease. Remission (complete “cleansing” of the body from tumor foci - in a sense, this term can be considered synonymous with recovery) is impossible. But there are treatments that help to slow down the progression of the disease to some extent, cope with painful symptoms and improve the patient's condition.
The goal of treating metastatic pancreatic cancer is to prolong the patient's life and control pain and other symptoms.
Features of metastasis in pancreatic cancer
Considerable progress has been made in the treatment of pancreatic cancer in recent years. However, it is still on the list of cancers with the worst prognosis. The chances of such a patient staying alive for five years are only 9%. At stage IV, when there are distant metastases, the five-year survival rate is 3%.
In general terms, metastasis of any malignant tumor occurs as follows. Some cancer cells break away from the main site and enter the blood or lymphatic vessels. They migrate with the blood or lymph flow, settle in various organs and, under certain circumstances, give rise to secondary foci - metastases.
The mechanisms of metastasis of malignant pancreatic tumors are not yet fully understood. But advances in molecular biology have been able to shed light on some nuances. Disturbances in the functions of certain proteins and genes play a role in the spread of cancer cells throughout the body:
- Cell adhesion molecules : E-cadherin, immunoglobulins, integrin. These proteins are located on the surface of the cell and normally ensure its connection with the extracellular matrix and other molecules.
- Matrix metalloproteinases : these enzymes are located outside cells, their function is to destroy proteins of the extracellular substance. They play an important role in the growth and development of cells, their migration, the formation of new blood vessels, and the inhibition of tumor growth.
- Plasminogen/plasmin systems . Plasmin is an active enzyme that is formed from the proenzyme plasminogen; its main function is the destruction of fibrin clots that make up blood clots.
- KAI1 gene . It prevents metastasis, and in pancreatic cancer its activity may decrease.
Tumor cells in the pancreas produce substances that stimulate angiogenesis , the growth of new blood vessels. This may also contribute to the spread of metastases.
How long do you have to live?
It all depends on the characteristics of the metastases. If you seek treatment in time and take appropriate measures, patients can live for about 3 more years. But if this is the last stage and the metastases have spread widely, then the period is reduced to a year or six months. And this despite the fact that the patient will be provided with maintenance therapy.
To prevent metastases in the pancreas , it is necessary to follow at least the basic rules of prevention. In addition, you can’t wait to go to the hospital, because a timely examination will help prescribe treatment in the early stages of their development.
Where do pancreatic malignant tumors most often metastasize?
Pancreatic cancer has a high tendency to metastasize. Even with small, less than 2 cm, malignant tumors, secondary lesions can often be detected. This partly explains why many patients already have metastases at the time of diagnosis.
Most often, secondary lesions are found in the following organs:
- Liver - in almost 80% of cases.
- In 40–50% of cases, carcinomatosis (damage by cancer cells) of the peritoneum develops.
- Lungs - in about 40% of cases.
- Lymph nodes in the abdominal cavity - 20%.
- Bones - 10%.
- Adrenal glands - 5–7%.
- Lymph nodes in the chest - 3%.
In less than 10% of cases, metastases from pancreatic cancer are found elsewhere. They can be found in almost any organ, including the diaphragm, brain, heart, gallbladder, kidneys, small and large intestine, pericardium, ovaries, testicles, stomach, skin, thyroid gland, spleen, uterus, bladder.
Even in cases where pancreatic cancer is operable and seemingly at an early stage, there are often already micrometastases in the abdominal organs and bone marrow. is most prone to hematogenous (through the bloodstream) spread, and to a lesser extent - malignant tumors of the head.
Pancreatic cancer can recur as distant metastases after treatment. For example, according to statistics, in 2/3 of operated patients with stages I and II of a malignant tumor, secondary lesions are subsequently discovered.
Diagnosis of the disease
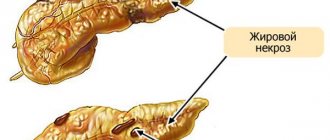
Complicated by the small size of the tumor and localization features. The organ, located on the back wall of the abdominal cavity, is additionally “covered” by the stomach. Active formation of distant metastases is not accompanied by compression of the ducts and does not manifest itself clinically. First, the pancreas itself and regional lymph nodes are affected. Gradually, the tissue of the liver, spine, vascular complex of the porta hepatis (biliary tract, portal vein), and duodenum are involved in the process.
What are the dangers of metastases in pancreatic cancer? Possible complications
Metastases are themselves a serious complication of any malignant tumor. They lead to the death of cancer patients in most cases.
Secondary lesions in the liver can lead to disruption of the outflow of bile and the development of jaundice . bilirubin, increases . The skin, mucous membranes and whites of the eyes turn yellow, causing itchy skin. The patient's condition and prognosis worsen, and the possibilities for active antitumor treatment are reduced.
With peritoneal carcinomatosis, the life expectancy of patients is reduced to 4–6 months, and this condition is very difficult to combat.
Ascites , can result from liver damage and peritoneal carcinomatosis . The abdomen increases in size, there is a feeling of heaviness, dull aching pain. When there is a lot of fluid, it restricts the movements of the diaphragm, shortness of breath occurs. Due to compression of the stomach and intestines, nausea, belching, and upset stool are bothersome. Urination is impaired.
Pancreatic cancer with metastases to the lungs can be complicated by exudative pleurisy . In this condition, fluid accumulates between the layers of the pleura , a thin film of connective tissue that lines the inside of the chest cavity and covers the lungs. This condition manifests itself in the form of weakness, shortness of breath, cough, and chest pain. In severe cases, the fluid causes compression of the lung, its ventilation significantly worsens, and blood flow to the heart is disrupted. Pulmonary heart failure develops , which can lead to death.
Bone metastases lead to weakening of bone tissue and pathological fractures from light loads. In more than half of the cases, the femur is affected. Pathological fractures of the vertebrae are especially dangerous, since they cause compression of the spinal cord, and if not treated in time, neurological damage becomes irreversible.
Up to 85% of patients with bone metastases from pancreatic cancer experience excruciating pain in the bones, which intensifies during exercise and at night.
Due to the intense destruction of bone tissue, the level of calcium in the blood increases - hypercalcemia . Its most common symptoms are: nausea, vomiting, abdominal pain, lack of appetite, weakness, lethargy, depression of consciousness, and heart rhythm disturbances. As this complication progresses, the functions of various organs are disrupted, and the patient dies due to cardiac arrhythmia or severe renal dysfunction. Half of patients with hypercalcemia die within a month. Average survival is 10 to 12 weeks.
Penetration of the tumor with metastases to other organs
For pancreatic cancer, there are target organs that are primarily affected during the growth of a malignant neoplasm. These include neighboring organs that are at risk of destruction:
- lymph nodes;
- all digestive organs;
- peritoneum;
- spleen.
In the absence of treatment, distant metastases develop:
- into the lungs;
- into the brain;
- in the bones.
The more metastases are formed, the more severe the patient’s general condition and the more unfavorable the prognosis. The rate of spread and the new location of malignant cells depends on the tissue from which the tumor grows and the degree of differentiation.
It has been established that metastases immediately affect the liver. This is due to its filter function: due to the dense network of vessels, atypical cells enter the liver tissue with the blood and lymph flow.
Pancreatic cancer is characterized by early metastasis, so the secondary lesion is often mistakenly mistaken for the primary tumor. This occurs in cases where, unlike the main process, it manifests itself earlier clinically and is immediately detected during diagnosis. The liver is the organ in which secondary foci, due to the frequent entry of carcinogenic cells into it, are detected earlier than pancreatic cancer itself.
Modern diagnostic methods
If pancreatic cancer is suspected, the doctor will most likely order a CT scan first. The images clearly show the pancreas; you can detect not only the primary tumor, but also its spread to neighboring organs and distant metastases. In addition, CT allows one to evaluate the possibility of surgical treatment.
The most informative is multi-slice computed tomography (MSCT) with multiphase intravenous bolus contrast . During this study, images are taken at certain intervals after intravenous administration of contrast solutions.
The diagnosis is usually confirmed with a biopsy. The doctor obtains a certain amount of pathologically altered tissue from the pancreas and sends it to the laboratory for cytological and histological examination. This can be done using a needle inserted through the skin under CT scan guidance.
Magnetic resonance imaging
Sometimes MRI is used to diagnose pancreatic cancer and its metastases. In some cases, special techniques are used:
- MR cholangiopancreatography - study of the condition of the bile ducts and pancreatic duct.
- MR angiography is the study of blood vessels.
Ultrasonography
When a patient is bothered by incomprehensible abdominal symptoms, most often an examination is prescribed with an ultrasound. But computed tomography is much more informative in diagnosing pancreatic cancer and its metastases.
Valuable data can be obtained using endoscopic ultrasound - endosonography , or endosonography . A miniature ultrasound sensor is used at the end of an endoscope, which the doctor inserts into the stomach and duodenum. A needle can also be inserted through an endoscope to perform a biopsy. Such a study is available in the European clinic.
Cholangiopancreatography
This study is used to check whether a pancreatic tumor or its metastases has blocked the bile ducts. The procedure can be performed in two ways:
- Retrograde cholangiopancreatography (RCPG) . This is an endoscopic procedure. The doctor inserts an endoscope into the duodenum, inserts a thin catheter into the bile ducts and fills them with a radiopaque solution. After this, the areas of narrowing are clearly visible on radiographs. During ERCP, you can install a drainage tube, perform a biopsy, and install a stent - a tube with a mesh metal wall that will expand the lumen of the blocked section of the duct and ensure normal outflow of bile.
- Percutaneous transhepatic cholangiography is performed with a needle through the skin. Typically, this method is used when, for various reasons, it is not possible to perform RCCP.
PET scan
Positron emission tomography is the gold standard for detecting distant metastases in modern oncology. The essence of the procedure is that a weak radioactive drug is injected into the patient’s body, which actively accumulates in tumor cells. Then the images are taken using a special device. All secondary tumor foci are clearly visible on them.
PET is even more informative if combined with computed tomography. With the help of CT, a high-quality image of different areas of the body is created, and with the help of PET, areas in which the radioactive drug accumulates are superimposed on it.
Laboratory research
For jaundice, a biochemical blood test is prescribed: the levels of different fractions of bilirubin and other substances that are markers of liver function are determined. A blood test helps assess the degree of deterioration of the organ and distinguish obstructive jaundice associated with impaired bile outflow from parenchymal jaundice caused by the destruction of liver cells - hepatocytes.
Symptoms
The patient may not immediately determine what is happening to him, since single metastases often occur. Their uniqueness lies in the fact that for a long time they do not appear in any way and do not show signs of their existence. Therefore, it is necessary to undergo diagnostic examinations as often as possible.
However, with the rapid progression of the disease, metastases immediately make themselves felt. A number of signs indicate that a tumor is growing in the body. The main symptoms include the following:
- Stomach ache. Over time, they become unbearable, so that the patient cannot do without painkillers.
- Loss of appetite. The consequence of this is a significant weight loss, the patient becomes weaker.
- Nausea and vomiting. At the same time, dizziness and a general deterioration in well-being appear.
- Problems with stool. This may be diarrhea, the urine becomes noticeably darker. Such signs are a direct consequence of problems with the pancreas.
- Itching and sweating. Sometimes accompanied by fever. A more individual symptom depends on the organism itself.
Usually the patient immediately observes a combination of symptoms. Therefore, you should not consider individual and single symptoms as clear prerequisites for tumor growth. Self-treatment is not allowed; for any question, consultation with your doctor is necessary!
Treatment of pancreatic cancer with metastases
For pancreatic cancer with metastases, surgical treatment is not used. The main way to fight a malignant tumor is chemotherapy. The choice of treatment tactics largely depends on the general condition of the patient and the morphological affiliation of the tumor. If it is bad, only one chemotherapy drug is prescribed, usually gemcitabine or capecitabine.
If the patient is in good condition, it is preferable to use the FOLFIRINOX combination of chemotherapy drugs. This regimen includes four drugs: 5-fluorouracil, irinotecan (Camptosar), leucovorin, oxaliplatin (Eloxatin).
If BRCA1, BRCA2, or PALB2 mutations are found in tumor cells, a combination of gemcitabine and cisplatin or olaparib (Lynparza) may be considered as treatment options. The latter is a targeted drug; it blocks the enzymes poly(ADP-ribose) polymerase (PARP).
The choice of chemotherapy agents for stage IV pancreatic cancer is limited, so patients whose condition allows them to tolerate active treatment should consider participating in clinical trials.
If first-line medications no longer help, your doctor may prescribe second-line treatment. Some possible schemes:
- FOLFIRI: 5-fluorouracil + leucovorin + irinotecan.
- OFF, FOLFOX: oxaliplatin + 5-fluorouracil + leucovorin.
- Capecitabine + oxaliplatin.
In some cases, radiation therapy is used to control symptoms.
Sometimes patients with stage IV pancreatic cancer benefit from pembrolizumab (Keytruda), an immunodrug from the group of checkpoint inhibitors. It blocks PD-1, a molecule that is found on the surface of immune cells and, by binding to PD-L1, a protein that can be found on the surface of cancer or other cells, suppresses the antitumor immune response.
Pembrolizumab activates the immune system, causing it to recognize and attack a malignant tumor. In 2021, the US Food and Drug Administration (FDA) granted accelerated approval to the targeted drug larotrectinib (Vitraqui). It is effective against various types of malignant tumors, including the pancreas, if the cancer cells have certain mutations.
It is possible to use chemoradiotherapy - a combination of chemotherapy drugs with irradiation of tumor foci. This treatment may be more effective, but it carries a higher risk of serious side effects.
Treatment of complications of pancreatic cancer metastases:
With obstructive jaundice, the outflow of bile can be restored using external, internal or external-internal drainage. During ERCP or percutaneous transhepatic cholangiography, a drainage tube is installed in the bile ducts, which drains bile out into the lumen of the duodenum or in both directions. A more modern solution is stenting, when a stent is placed in the blocked area during ERCP. It is a tube with a mesh wall made of metal or polymer.
For peritoneal carcinomatosis, in some cases, the modern technique of hyperthermic intraperitoneal chemotherapy (HIPEC) . If the cancer is confined to the abdomen, the surgeon may remove any large tumor lesions and then flush the abdomen with a warmed chemotherapy solution to destroy any remaining cancer cells. Unfortunately, HIPEC is not suitable for all patients. In order for such treatment to be carried out, there must be no metastases outside the abdominal cavity, all large lesions must be resectable, and the patient must be in a state of health that allows major surgery.
For chronic pain, medications are prescribed in accordance with the “pain ladder” recommended by the World Health Association. Nerve blocks are indicated for some patients with metastatic pancreatic cancer.
For ascites, laparocentesis is indicated - a procedure during which a puncture is made in the abdominal wall to remove fluid. Peritoneal catheters are installed to ensure constant fluid drainage . Some patients require surgery to prevent fluid accumulation.
For exudative pleurisy, thoracentesis is indicated - a procedure in which fluid is removed from the pleural cavity through a puncture. Systemic chemotherapy helps prevent its further accumulation. If it is ineffective, pleurodesis is performed - a procedure during which a drug is injected between the layers of the pleura, as a result of which they stick together and fluid stops accumulating between them.
For bone metastases, drugs from the bisphosphonate group are used to prevent bone loss. If there is a high risk of pathological fracture, the bone can be strengthened with metal plates or screws. With their help, you can restore the integrity of the bone if a fracture has already occurred. In some cases, special bone cement is used.
What are metastases
When the main tumor is located in the tissues of the stomach or, for example, the kidneys, it is called primary. A malignant neoplasm appears at the moment when the first cell with a defective gene reproduces in the body. Its mutation occurs against the background of a hereditary predisposition or due to the effect of carcinogens on a specific organ.
Subsequently, the growth of the tumor and the spread of its cells to other organs is carried out through their uncontrolled division. In medicine, this process is called abnormal mitosis.
The life cycle of pathological cells is much shorter than that of normal ones, but the rate of their division is so high that it is faster than the rate of death.
Cancer patients may experience local spread of cancer cells. It happens when a primary tumor grows into the tissue of a neighboring organ. But the circulatory and lymphatic systems also contribute to the metastasis of cancer cells. Cancer cells enter there as a result of destruction of the walls of blood vessels by an overgrown neoplasm. Secondary lesions begin to form as soon as a cancer agent circulating in the hematogenous or lymphatic system manages to attach to the tissues of the organ through which the vessel passes.
Forecast
To assess prognosis in oncology, the five-year survival rate is used - the percentage of patients who remain alive within five years from the date of diagnosis. For pancreatic cancer with metastases, this figure is about 3%. This is the worst prognosis among all tumors of the digestive system.
But even such a terrible diagnosis is not a reason to give up. There are effective treatments that help prolong the patient's life. Literally every year the possibilities of oncology are growing. Even if the patient managed to give an extra week of life without pain and other painful symptoms, it was worth fighting for. For us there are no hopeless patients. Contact us to find out more about treatment options at the European Clinic.
Book a consultation 24 hours a day
+7+7+78
Forecast by stage
This disease occurs due to factors such as obesity, alcoholism, and poor quality of drinking water consumed. The causes of the disease can be diabetes, cholelithiasis, and hereditary predisposition. In 70 percent of cases, cancer affects the head of the pancreas, 20 percent - the body, and 10 percent - the tail.
First stage
In this case, the tumor has no more than two centimeters in diameter and is located only in the pancreatic tissue. In this case, the right treatment can return a person to normal life within six months. Surgical removal of part of the pancreas (the place where the tumor is located) is recommended. After surgery, a person's health may improve.
What to do if you have diabetes?!
Read more >> |
Second stage
The tumor has a diameter of about three centimeters; in this case, natural blood flow may be disrupted. The lymphatic system is affected and metastases form. The survival rate of patients after surgery in this case is 30 percent, and the patient is operated on.
During the operation, the affected areas of the pancreas are eliminated. The patient is prescribed a course of chemotherapy. Doctors say that you can live with this for no more than 3-4 years.
Third stage
During this period, the tumor actively develops. Its cells disrupt the functioning of the gastrointestinal tract. Metastases penetrate the bone marrow, and at this stage of development, recovery is possible for 2-3 patients out of 1000. Treatment of the disease at this stage is complicated by the fact that it is accompanied by renal failure and diabetes mellitus. A patient with this diagnosis lives no more than 2 years.
Fourth stage
The malignant tumor spreads throughout the body, penetrates the bone marrow, and the person has virtually no chance of life. Operations in this state are no longer performed, and the person is left with the last months of his existence.
Doctors improve the inoperable life expectancy with the help of chemical therapy and pills. Often the patient is sedated with morphine to relieve pain.
Treatment methods and the prognosis of how long the patient will live can only be determined after a complete clinical examination. In the early stages of the disease, a person does not feel discomfort. Then pain appears in the upper abdomen. As the disease progresses, the patient begins to lose weight and has abdominal pain.
Latest research
In 2014, the American journal AACR, dedicated to cancer research, published information that by 2030 in the United States, pancreatic cancer will take the second position in mortality. This information was obtained as a result of a certain series of studies. Along with them, it was noted that this trend will be observed in many countries, since the eating habits and eating habits of all modern people, regardless of nationality, are approximately the same - these are dry snacks on the go, coffee, alcoholic drinks, addiction to fast food and products containing preservatives, which primarily affects the health of the pancreas.
Vice President of the Scientific and Medical Center in the USA Lynn Matrisian then stated that the overall mortality rate from malignant tumors is gradually decreasing, however, this does not apply at all to liver and pancreas cancer. According to her opinion, this fact should serve as motivation for further research on this issue and the development of new methods in the fight against such pathology.
The conference discussed news regarding the latest research in the field of pancreatic cancer.
- A set of biomarkers may make it possible to detect cancer at an early stage of development, said Aumu Taguchi, an associate professor at the University of Texas. He argues that the complex of biomarkers provided more informative information than the CA19-9 tumor marker alone. This indicates that the identified group of biomarkers can significantly reduce the number of patients who require one or another invasive diagnosis. Development is underway to determine such a complex of biomarkers, which will find wide application in medicine.
- Radioimmunotherapy and Gemcitabine are a combination for the successful treatment of cancer tumors. Radioimmunotherapy involves exposing cancer cells to radioactive substances. Vincent J. Piccosi Jr., director of the Pancreatic Disease Research Center in Virginia, says that radiotherapy, unlike radiation, is effective in destroying malignant cells located anywhere in the body, including treating tumors located in the pancreas .
A clinical trial was conducted in which 58 patients with this diagnosis took part. They were divided into 2 groups. The first received a course of radiotherapy along with chemotherapy drugs: Gemcitabine was used in a small dose. The second group received only radioimmunotherapy. As a result of this experiment, it was found that the survival period of patients in group A was 45% longer than that of those patients who did not receive chemotherapy drugs. In real time terms, the difference in life expectancy was as follows: 7.9 months for participants in group A and 3.4 months for patients in group B.
- Blocking the CD47 protein. Such measures led to the destruction of a neuroendocrine neoplasm of the pancreas and ductal adenocarcinoma of this organ in mice. It was in these types of cancer that high levels of CD47 were detected. The results obtained formed the basis for further developments, which are currently being worked on by specialists at Stanford University in California.
Cancer prognosis and life expectancy
It is impossible to say unambiguously how long people diagnosed with pancreatic cancer live, since life expectancy depends on the specific individual case. Many factors can be decisive here: the patient’s age, the presence of chronic or any infectious diseases, the size of the tumor, its morphological structure, the presence or absence of metastases in other organs, etc.
According to statistics, 50% of cancer patients who learned about their disease at the 2nd stage of its development live about 5 years; for pancreatic cancer of the 3rd and 4th degrees, survival is approximately 6-12 months. Surgery plays an important role in the treatment of pancreatic malignancy, but since an advanced tumor is no longer operable, the patient’s life expectancy is reduced significantly. Most often, in such a situation, palliative therapy is used, thanks to which only the manifestations of the pathology are eliminated, and not the pathology itself.
Treatment therapy can achieve successful results when the tumor is detected at a very early stage. However, due to the fact that pancreatic cancer is completely asymptomatic at first, the patient does not even realize the presence of pathology in his body, and therefore turns to doctors only when it is too late.
Prognosis for the treatment of testicular cancer at different stages
- The 5-year survival rate of patients practically reaches 100% if the tumor can be detected at stage 1, that is, when the lesion has not yet spread beyond the testis. It is necessary to immediately clarify that the meaning of the medical term “survival” is often misinterpreted. In fact, this statistical indicator refers to the percentage of patients who have not had a relapse of the disease for a given number of years. But this does not mean that the life of the treated patient is limited to just one, two or five years.
- In stage 2 testicular cancer, tumor cells are found in nearby lymph nodes, which requires expanding the scope of treatment, but only slightly worsens the prognosis: the five-year survival rate reaches 90-95%.
- Therapy for patients with metastases (stage 3-4 testicular cancer) can also be very successful: in 80 out of 100 such patients, the disease does not return in the next five years. There is another positive point: if a relapse does occur, then, most often, it can also be stopped.
ul
Diagnosis of metastases in the pancreas
Experts point out the significant difficulty in diagnosing pancreatic metastases, which is due to the peculiarities of its structure. In order to timely identify the pathological process, the following laboratory and instrumental studies will be recommended:
- various blood tests;
- tumor markers;
- Ultrasound;
- MRI or CT;
- fine-needle biopsy - collection of biomaterial directly from the tumor focus followed by examination under a microscope;
- ERCP;
- endoscopic methods;
- UZT.