In the modern world, it is difficult for a person to lead a healthy lifestyle. Due to poor nutrition and alcohol intake, internal organs are negatively affected. This leads to various diseases and pathologies of the digestive organs.
The pancreas is a multifunctional organ of the human digestive system. It participates in metabolic processes and carries a double load. But people remember about it only with diagnoses such as pancreatitis and diabetes.
Pancreas: role
The pancreas regulates the digestion process.
The role of the pancreas is very significant in human life. It is involved in the secretion of enzymes that synthesize nutrients and the hormone insulin, and also regulates the entire process of food digestion.
Pancreatic juice of the gland helps enhance the process of digestion of food. This organ is located behind the stomach at the level of the thoracic and lumbar vertebrae in the abdominal cavity. Improper functioning of the organ contributes to the development of diabetes, pancreatitis and pancreatic necrosis.
Useful article? Share the link on VKontakte
The digestive gland is divided into a head, body and tail. A change in the size of these sections leads to improper functioning of the gland and the development of various diseases. Any disorders of this organ can adversely affect the stomach, liver, heart and spleen.
Because the gland is very close to them and leads to other diseases of these organs. For this reason, it is important to know the size of this organ and what its deviation from the norm can lead to.
Symptoms of pancreatic atrophy
The clinical picture of the disease is determined by the cause of its development (diabetes mellitus, chronic pancreatitis and others). However, in any case, the characteristic symptoms are exocrine and endocrine insufficiency. Exocrine (exocrine) glandular insufficiency is characterized by decreased production of digestive enzymes, as well as bicarbonates and other electrolytes, which neutralize the contents of the stomach, providing an environment favorable for the action of pancreatic enzymes. Typical symptoms are loose stools, loss of appetite, and weight loss.
An early symptom of insufficiency of exocrine function is steatorrhea (increased excretion of fats in feces). This symptom develops when secretion decreases by 10% of normal. Weight loss occurs due to impaired digestion of food, absorption of substances in the intestines, and loss of appetite. With long-term pathology, signs of vitamin deficiency develop.
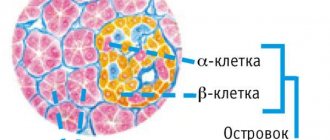
Endocrine (intrasecretory) insufficiency is manifested by disturbances in carbohydrate metabolism, occurring as a hyperglycemic syndrome. However, symptoms of diabetes develop in only half of patients. This is explained by the fact that insulin-producing cells have the ability to survive pathology better than acinar cells. Insulin and glucagon deficiency develops. The patient may experience severe weakness, dizziness, and thirst.
Pancreas size in a healthy person
The pancreas is the same size in both men and women.
Not everyone knows the size of the pancreas of a healthy person. And its parameters directly affect the condition of the organ itself and indicate the development of diseases.
A healthy digestive gland has an elongated shape and a tail curved upward. In men and women it is the same size: length on average from 16 to 23 cm, width - up to 9 cm, and thickness - up to 3 cm. The length of the head of the gland is up to 32 mm, the body is up to 21-25 mm, and the tail is up to 30 -35mm.
The Wirsung duct, which passes inside the gland and delivers pancreatic juice to other organs, is 20 cm long and 4 cm wide. The normal weight of the digestive gland reaches 150 g on average.
It is also important to know that the pancreas is formed in a person in the womb already at 4-5 weeks. By the time of birth, it has a length of no more than 5-5.5 cm. At the age of one year, the length reaches 7 cm, and the thickness - up to 1 cm. Then the gland develops gradually along with the entire body.
At the age of ten, the child’s pancreas is 15 cm long, and at the age of 14 the organ sharply enlarges. And only in adulthood does the digestive gland reach its constant size.
Normal parameters of the pancreas ensure the health and proper functioning of all organs of the digestive system. The slightest deviation from the norm indicates pathology.
Therefore, if its size increases, you must immediately look for the cause and begin treatment.
Ultrasound diagnostics of the pancreas
Pain in the left side under the ribs may be a sign of pancreatitis
Ultrasound diagnostics of the abdominal organs is prescribed for certain indications when there are suspicions of pathologies.
An ultrasound should be done if the following signs appear:
- pain in the left hypochondrium;
- pain when palpating or the presence of unknown formations;
- symptoms of digestive disorders: weight loss, change in stool;
- blood counts indicating pancreatitis or diabetes mellitus;
- heaviness in the stomach after eating;
- deformation of the duodenum;
- signs of jaundice (yellow discoloration of the skin).
Important. A diagnosis cannot be made on the basis of ultrasound alone, but the results obtained from this study are important in determining the disease. The advantages of this method are low price, safety, simplicity and high information content.
What will an ultrasound show?
Photo of ultrasound of the pancreas is normal
During ultrasound examination of organs, diagnostic signs of diseases are:
- morphological changes in the organ;
- echogenicity of tissues;
- sizes of organ parts;
- the presence of compactions or neoplasms.
Diagnosis involves examining not only the pancreas, but also nearby organs: the liver, gallbladder, spleen and their ducts. If at the time of examination the deviation from the norm is more than 5 mm, this is grounds to assume an acute or chronic disease.
The following are pathologies determined by ultrasound:
- Pancreatitis . Acute (disruption of tissue structure, swelling of the gland) or chronic (cyst-like formations, stones localized in the ducts, compactions in the parenchyma, increase in size).
- Neoplasms (benign or malignant) . In this case, compacted lesions, their location and lesions of the lymph nodes are visible. The doctor can measure the size of the tumors. These signs require mandatory confirmation using more high-precision methods (CT and MRI), and a study of histological material will also be required.
- Necrosis, abdominal dropsy (ascites), abscesses.
In order for ultrasound to correctly and as clearly as possible display all the nuances of the structure of the abdominal organs, you need to know how to properly prepare for the upcoming study. If this is not done, the accuracy of the results will decrease by 30-40%.
The essence of a diagnostic study is to reflect ultrasound from the walls of organs and display their outlines on the monitor of a diagnostic apparatus. For better access to ultrasound waves, the doctor will ask the patient to lie on his side several times and hold his breath.
During the examination, you should take a towel and wet wipes with you to wipe off the gel applied to the skin. Instructions for preparing for the study are indicated in the table.
Table. Preparing for an ultrasound of the pancreas:
| What should be done | A comment |
| An ultrasound is performed in the morning because the digestive organs should not contain food. There should be a light dinner the night before; you should not eat in the morning. The study is performed on an empty stomach. |
| During the day you should refrain from drinking carbonated drinks and foods that cause fermentation. For a good overview of the pancreas, there should be no accumulation of gases in the intestines and stomach, otherwise the data will be distorted. To reduce gas formation the day before the ultrasound, you should take espumizan (two tablets with each meal). |
| If a person does not have digestive problems and defecates regularly, then nothing needs to be done. But, as a rule, people with gastrointestinal pathologies have these problems. Therefore, on the eve of the examination, it is recommended to take activated carbon and laxatives. |
Nuances of ultrasound of the pancreas
Acute pancreatitis on an ultrasound image
During the examination, the patient's weight and age are taken into account. In obese people, the organ size is larger, and the older the person, the higher the echogenicity of the tissue.
The child’s organ will be smaller; weight also matters, which is necessarily taken into account by the doctor during the examination. At the end of the procedure, a description is carried out within a few minutes, a decision is made regarding the norm or deviations, and the conclusion is handed out.
It makes sense to take photographs of the abdominal organs in the presence of pathologies so that comparisons can be made in the future.
A person is healthy if:
- tissue of homogeneous echogenicity, no significant diffuse changes or neoplasms (cysts, stones or tumors);
- the organ has a clear, equal outline, the contours are not changed;
- all sizes are within acceptable values (normal size is 16-23 cm, gland body width 21-25 mm, head width up to 35 mm, tail 30-31 mm, diameter of the Wirsung duct in the head area 2.6-3.3 mm ).
The presence of the disease is indicated by the following deviations:
- Pancreatitis is the most commonly diagnosed diagnosis when the structure of the gland is disrupted in the form of its enlargement and diffuse tissue changes. In this case, contours may be poorly visible and echogenicity decreases. If there are difficult to distinguish zones of dense echogenicity, merging into a single cavity, this indicates the onset of pancreatic necrosis. As a rule, the cavity of these cysts is filled with purulent masses;
- If tissue death occurs in the gland, accompanied by the release of pus, then a cavity is formed, which is filled to a certain extent with liquid secretions. When changing body position, fluid vibrations can be recorded;
- The presence of pseudocysts on the monitor of an ultrasound machine is visible in the form of anechoic cavities filled with liquid;
- Suspicion of jaundice is diagnosed when narrowing or blockage of the bile ducts is detected;
- Oncological neoplasms are visible as clearly distinguishable heterogeneous foci. In this case, the doctor must very carefully examine the pathological foci, especially in the tail.
Note. All changes obtained using ultrasound are not a final diagnosis and require additional examination.
Causes of pancreatic diseases
Inflammation of the pancreas can cause pancreatitis.
The development of acute inflammation is rapid and can develop into a chronic form.
In diseases of the gland, the enzymes that it produces do not pass into the intestines, as during normal activity, but are activated inside the organ, thereby destroying it.
Toxins released into the bloodstream cause serious harm to other internal organs. The causes of inflammation can be excessive alcohol consumption, spicy and fatty foods, as well as cholelithiasis. Doctors include other risk factors:
- Duodenal disease;
- Surgical intervention for stomach diseases;
- Abdominal injury;
- Taking medications;
- Infectious diseases and hepatitis;
- Metabolic disease;
- Hormonal disorders;
- Heredity;
- Poor nutrition.
All these factors in their own way disrupt the normal functioning of the digestive gland. Violation of the outflow of pancreatic juice into the intestines leads to premature activation of enzymes in the organ itself. The gland tissue can be replaced by scar tissue and functions (endocrine and exocrine) are disrupted, which again leads to major inflammation.
Prevention and diagnosis of such diseases is mandatory for everyone. If you do not go to the doctor in time, the disease will lead to various complications. Very often, patients with pancreatitis also suffer from inflammation of the gallbladder.
In rare cases, internal bleeding develops. Another complication of this disease is no less dangerous - the development of peritonitis, which is accompanied by a serious condition and leads to an unfavorable outcome.
Diseases of the pancreas develop quickly and can lead to disastrous consequences. Therefore, if the following symptoms appear, a person must immediately undergo diagnosis:
- Pain in the subcostal area;
- Nausea and vomiting after eating;
- Loss of appetite;
- Increased body temperature;
- Bloating and stool retention;
- Unstable stool;
- Pale and yellow skin;
- Feeling of heaviness in the stomach.
Causes of pancreatic atrophy
This condition can be physiological, developing as a result of the natural aging processes of the body. It accompanies severe debilitating diseases (cachectic form). Also, atrophy is the outcome of all forms of chronic pancreatitis, with a significant part of the stroma being replaced by fibrous tissue, which is accompanied by the progression of endocrine and exocrine insufficiency.
A special place is occupied by pancreas atrophy in diabetes mellitus. This pathology is accompanied by a significant decrease in the size of the gland - up to 20-18 g, the consistency is significantly compacted, the surface of the organ is lumpy, the capsule is fused with the surrounding adipose tissue, as well as neighboring organs. At the microscopic level, the lesion is characterized by diffuse proliferation of fibrous tissue (intraacinous sclerosis), death of glandular parenchyma cells.
Pancreatic lipomatosis is also its atrophy. Despite the fact that this condition is characterized by the preservation or even increase in the size of the organ (pseudohypertrophy), most of it is replaced by adipose tissue, which contains individual glandular areas. In most cases, with lipomatosis, the islet apparatus and endocrine function of the organ are preserved. More rare cases of the disease in gastroenterology include atrophy of the gland due to cirrhosis of the liver, systemic scleroderma, compression by a tumor, blocking of the excretory ducts with stones.
Preparing for an ultrasound
An ultrasound of the pancreas will help make the correct diagnosis.
It is difficult to make a diagnosis of inflammation due to the location of this organ. It is located near the stomach and intestines, where gas is produced.
To obtain a normal picture, it is necessary to eliminate gases before performing an ultrasound, otherwise the ultrasound may not penetrate.
Two days before the examination, you should not eat foods that lead to the accumulation of gases (legumes, vegetables, carbonated water, flour and sweets). In the morning hours a person has few gases in his organs and therefore it is recommended to go at this time.
You should start the ultrasound on an empty stomach (last meal within 12 hours). On the day of the examination, do not take medications or alcohol. Sometimes medications are prescribed to cleanse the intestines. Failure to follow these simple recommendations increases the likelihood of misdiagnosis by up to 40%.
It is important to know that in this way the doctor can only give information about the appearance and size of the gland. And for an accurate diagnosis, you need to undergo additional research: computed tomography and blood tests. On an ultrasound scan of a person with a healthy pancreas, the doctor reveals the following:
- Absence of formations and anatomical anomalies;
- Standard gland sizes;
- The main duct is 1.5 to 2 mm wide;
- Clear outline of the organ;
- Homogeneous structure;
- Echogenicity, as in the liver and spleen.
All these factors together indicate the healthy state of the organ. If one of the indicators does not correspond, this indicates the development of inflammation.
Treatment of pancreatic diseases
A proper diet will help restore normal functioning of the organ.
In the treatment of diseases of the digestive gland, two methods can be used: conservative and radical.
In the first case, the patient is prescribed intravenous nutrition (starvation diet), during which toxins are cleansed with the introduction of electrolytes. The patient also takes medications that inhibit the formation of enzymes in the digestive gland.
For radical treatment, laparoscopy is performed. This operation involves a small incision and the use of an observation device (endoscope). In some cases, drainage may be performed. In this way, the doctor removes the resulting pus and toxic substances.
For any complications, doctors use all possible methods for treatment, but they may be ineffective. And then you have to do a resection of the organ - partial or complete removal of the pancreas.
It is important to remember that this organ is involved in the synthesis of hormones and enzymes, without which the absorption and digestion of food is impossible. It is in this gland that substances necessary for the body are produced. There is a possibility of complications during surgery and after removal.
Proper nutrition and eradication of bad habits can prevent diseases not only of the pancreas. Therefore, you need to change your lifestyle in accordance with this. Doctors also recommend checking the size of the pancreas to observe its deviation.
Learn how to keep your pancreas healthy from the video:
Pancreatic lipomatosis is a pathology in which normal cells are replaced by fat cells. Such changes negatively affect the performance of the organ. The situation is aggravated by the long asymptomatic period.
In fact, a person begins treatment when it is no longer possible to change something for the better using conservative methods. This article provides expert advice that will help you diagnose the disease in a timely manner and take adequate response measures.
Pancreas in Adults: Size, Norms, Deviations
Ultrasound diagnostics for suspected pancreatic dysfunction is the first and main method in detecting pancreatitis, diabetes mellitus and various diseases of the digestive system. Ultrasound is indicated for people who do not adhere to a healthy lifestyle or abuse bad habits.
The organ changes depending on the age of the person. At first it grows, then remains stable for a long time.
With age, certain changes may occur in the pancreas; it becomes smaller. Thus, for each age category there are certain norms, deviations from which indicate the development of a pathological process.
Dimensions and location
The pancreas is localized in the abdominal cavity on the left side below the stomach (hence the name) parallel to the costal arches in close proximity to the liver and spleen. There are three sections: the head (opens directly into the duodenum), body and tail.
Its role in the body is the formation of digestive enzymes and the synthesis of insulin, which is responsible for the concentration of glucose in the blood. Thus, iron participates in tissue nutrition. Disturbances in its work lead to serious pathologies of an endocrine nature.
During inflammation, the release of digestive enzymes becomes difficult; they begin to digest the parenchyma of the organ, causing the replacement of normal tissues with connective tissues; necrosis can cause the development of an oncological process.
In a healthy adult, the normal size of the pancreas is in the range of 16–23 cm. The size of the head is 32 mm. The longest part is the tail, it should not exceed 35 mm. The width of the organ is 5 cm.
If everything is normal, then the person does not feel pain or any discomfort; the organ cannot be felt during palpation. When the size of the pancreas exceeds 25 cm and the size of the tail exceeds 35 mm, this will indicate the presence of a pathological process (with pancreatitis and oncological processes it increases, a decrease indicates ischemia or atrophy).
The note. The size of the pancreas does not depend on a person’s gender, so they are the same in men and women.
The structure of the pancreas
In infants, the size of the organ is approximately five centimeters. By the first year of life it will increase by two centimeters, and by ten years the size will be 15 cm. Further growth will be slowed down until hormonal changes in the body.
During puberty, the organ grows to normal size, like that of an adult, and is fully formed by the age of 18-20. For many, final formation occurs by the age of 16.
The main excretory channel for digestive enzymes produced in the gland is the Wirsung duct (length 20 cm), into which smaller excretory ducts drain. It begins in the tail and runs along the entire gland, eventually flowing into the duodenum.
If its size exceeds the norm, then this indicates the presence of a painful process, which in most cases is pancreatitis. In this case, the digestion and absorption of food is disrupted, since enzymes do not enter the stomach in the required quantities. Their excess in iron leads to the fact that it begins to digest itself.
You can see changes using ultrasound, CT or MRI. The last two methods are the most informative, but the price of such diagnostics is quite high, and during computed tomography a person is exposed to a significant dose of radioactive radiation.
Ultrasound diagnostics of the pancreas
Pain in the left side under the ribs may be a sign of pancreatitis
Ultrasound diagnostics of the abdominal organs is prescribed for certain indications when there are suspicions of pathologies.
An ultrasound should be done if the following signs appear:
- pain in the left hypochondrium;
- pain when palpating or the presence of unknown formations;
- symptoms of digestive disorders: weight loss, change in stool;
- blood counts indicating pancreatitis or diabetes mellitus;
- heaviness in the stomach after eating;
- deformation of the duodenum;
- signs of jaundice (yellow discoloration of the skin).
Important. A diagnosis cannot be made on the basis of ultrasound alone, but the results obtained from this study are important in determining the disease. The advantages of this method are low price, safety, simplicity and high information content.
Risk factors
Pancreatic lipomatosis is fatty pancreas.
Why some people develop lipomatosis and others do not is not known for certain.
However, ongoing statistical studies allow us to identify some risk factors, the presence of which may lead to the formation of unwanted fat cells in the pancreas.
The most common situations that provoke the development of lipomatosis are given below:
- history of acute pancreatitis;
- current chronic pancreatitis;
- frequent consumption of alcoholic beverages;
- burdened heredity;
- current diabetes mellitus or chronic hepatitis;
- obesity;
- insufficient amount of thyroid hormones.
The fact that the factors mentioned above can provoke the development of lipomatosis does not mean that those who have these conditions will necessarily develop pancreatic obesity. However, in the absence of all these factors, the disease almost never develops.
The concept of atrophic changes in the glands
As a result of atrophic pancreatitis, active areas in the pancreas are completely or partially replaced by inert ones. Atrophy of the pancreas leads to a reduction in the volume of the mucosa with thickening of the membrane. A characteristic sign of the onset of the process is functional failure:
- with exocrine disorders, the synthesis of digestive enzymes and bicarbonates is disrupted;
- with intrasecretory pathology, the synthesis of insulin and glucagon slows down.
The process can be initiated due to the characteristics of physiological development, against the background of debilitating diseases, tumor compression, damage to the filling mass (parenchyma), disruption of the system of supplying the choroid plexuses of the organ with blood.
The total weight of the gland normally reaches 90 g. If the mucosa is atrophic, its weight decreases sharply down to 30 g.
Pancreatic atrophy.
Structural changes in the pancreas are characterized by the formation of excess connective tissue. This inert material proliferates around the lobules of the organ, indicating perilobular sclerosis. If the process occurs diffusely, then intralobular sclerosis is diagnosed. Subatrophy can be of different types, for example, with lipomatosis, part of the parenchyma is converted into fatty masses.
Symptoms of fatty degeneration of the pancreas
An ultrasound will help identify the disease.
The main pathology of this disease is the replacement of parenchyma with fat cells. This process is extremely slow and can generally take several years or decades.
It can be discovered accidentally during ultrasound diagnostics of this organ. The first negative sensations appear only when a third of the organ becomes modified.
Then they begin to intensify, causing multiple symptoms. But despite all the versatility of the manifestation of symptoms, they are all a consequence of 2 global disorders:
- dysfunction of the pancreas;
- compression of healthy tissues of this organ and others that surround it.
Signs of pancreatic malfunction
Due to a decrease in the percentage of healthy, normally functioning tissues in relation to the affected ones, digestion is disrupted. Protein foods and everything fatty are especially difficult to perceive. A person experiences the following symptoms:
- nausea;
- stomach ache;
- flatulence;
- heaviness, bursting feeling in the stomach;
- frequent stools containing fat and other impurities.
Due to the disease, disruptions in the production of hormones occur. As a result, complex endocrinological disorders develop. This applies to a greater extent to carbohydrate metabolism. At the same time, glucose levels increase sharply.
If this pathological course is not stopped, then over time a person will develop diabetes.
Symptoms
The pathology is accompanied by swelling of the gland, changes in blood circulation, the appearance of necrosis and cysts. Causes hyperinsulinemia (diabetes mellitus). Exocrine insufficiency (external) appears. Digestive disorders are observed: weight loss, poor appetite, nausea or vomiting, diarrhea, and fats are passed out along with the stool. The absorption of vitamins is impaired, paleness of the skin and mucous membranes, weakness, distortion of taste, and decreased muscle tone appear.
Endocrine insufficiency (internal) is explained by a violation of carbohydrate metabolism. This leads to the symptoms of diabetes - constant unquenchable thirst, dizziness, swelling, polyuria (excess urine), dry and itchy skin.
General and first signs are pain in the left hypochondrium, bloating after eating, the tongue changes color to crimson or red, plaque and teeth marks.
Diagnostics
Examinations begin with a visual examination (skin condition, appearance), determination of body weight deficiency, questioning of the patient, information about heredity. A blood test shows decreased pancreatic enzymes, anemia, and elevated glucose levels.
The following studies are also indicated:
- Coprogram - a study of stool to determine the amount of excreted fat.
- Ultrasound - reduction in the size of the gland, compaction.
- Pancreatic biopsy provides information about the extent of the lesion and facilitates prognosis.
- MRI.
If symptoms occur, you should immediately make an appointment with an endocrinologist, surgeon, or gastroenterologist.
Compression of surrounding tissues
Abdominal pain is a sign of gastrointestinal dysfunction.
Fat cells can develop to fill a large space. As a result, adipose tissue grows, which takes up much more space than the healthy cells that precede it.
If the fat cells are distributed evenly throughout the pancreas, then this will not cause problems. The situation is worse when cells are collected in groups.
Then they start talking about lipoma - a benign tumor. There is nothing too scary about it, because it will not give metastases, which means it will not cause harm to neighboring organs.
Trouble will occur when the tumor develops to such a size that it begins to put pressure on the vessels, pancreatic ducts, and nerve endings. Such exposure will lead to pain, nausea, flatulence and other unpleasant symptoms.
Watch the video about the risk of developing diabetes and obesity:
Nutrition for lipomatosis
There is an opinion in everyday life that reducing the amount of fat in the diet will help stop lipomatosis. This is a completely false statement.
Even completely stopping fat intake will not stop the degeneration of healthy cells into fat cells. The development of lipomatosis has nothing to do with nutrition. However, it is still better to exclude fats. This will have a beneficial effect on the body:
- relief of pancreas;
- getting rid of extra pounds.
Reducing the amount of incoming fat helps alleviate the condition; many signs of the disease recede and become less pronounced. In the absence of external manifestations of the disease, we can talk about preserved pancreatic functionality.
This means that all the ducts are functioning normally, they are not compressed by adipose tissue. With normal functioning of the pancreas, limiting fats in food will help you lose weight, but will not affect the further development of the disease.
Treatment of lipomatosis
Ibuprofen is a drug to relieve abdominal pain.
It is almost impossible to get rid of lipomatosis. The current treatment method goes in 3 directions:
- Lifestyle changes.
- Use of medications.
- Surgical intervention.
Changing your lifestyle in the right direction will help improve the situation as a whole. With persistence and perseverance, you can achieve a lot.
The condition of patients seeking recovery improves even without additional medications. The basics of getting rid of pathology are giving up alcohol and other bad habits, normalizing your diet, and getting rid of excess weight.
To achieve good results, you need to be more active. The second important factor is diet. Following the nutritional principles outlined below will help get rid of many problems. The principles are:
- Fractional meals. The desired number of meals is at least 5, optimal is 6.
- Limit fat. Avoiding sweet, fatty foods.
- A general reduction in the calorie content of dishes, the desire to reduce the daily volume of incoming calories.
It is almost impossible to resolve the situation with medications. Taking medications only helps to get rid of unpleasant symptoms. To eliminate the severe consequences of pancreatic obesity, the following drugs are taken:
- Ibuprofen for pain relief.
- Pancreatin for correcting digestion.
- Loperamide to block diarrhea.
- Metoclopramide to relieve nausea.
- Mebeverine to relieve intestinal spasms.
You should not get carried away with taking these medications. After all, they all have negative side effects on the body. Self-medication is highly undesirable. After all, the situation can be critical, and eliminating the symptoms will not help stop the process of tissue degeneration.
The accumulation of fat cells can become critically dangerous. The degree of threat can only be determined by a specialist and, if necessary, sent for surgical treatment.
Treatment
The treatment of the pancreatic organ, as well as the diagnosis of its pathologies, is approached in a comprehensive manner. The treatment process is based on the use of the following techniques:
- Taking medications;
- Diet therapy;
- Surgery;
- Phytotherapy.
Since the trigger mechanism for pathological processes is inflammatory damage to the organ, therapy is primarily aimed at stopping the inflammatory process.
For this purpose the following medications are prescribed:
- Antibiotics from the group of penicillins or cephalosporins, fluoroquinolones and intestinal antiseptics such as Amoxiclav, Nifuroxazide, etc. The duration of therapy lasts about 2 weeks and only as prescribed by a doctor.
- Anti-inflammatory drugs that relieve pain in the gland and stomach, such as Nimesulide, Ibuprofen, Ketorol, etc.
- Painkillers such as antispasmodics, which effectively relieve spasms and relax muscles. Such drugs include No-shpu, Spazmalgon, Drotaverine, etc.
- Replacement therapy with enzyme preparations such as Mezim, Creon or Pancreatin.
If the clinical situation is severely advanced or the cause of the pancreatic pathology is a tumor, then surgical therapy is indicated.
Preventive actions
Proper nutrition is an excellent prevention of obesity.
Fatty degeneration of the pancreas can be prevented, but not cured.
Therefore, you need to follow a number of simple steps to maintain your health and not face the need to treat lipomatosis. Advice from experts on preventing this disease is as follows:
- Weight control.
- Quitting alcohol.
- Refusal of fatty foods.
- Eliminating stressful situations from life.
Smoking also weakens pancreatic function, so it is also better to give it up. After all, pancreatitis is a consequence of smoking, and lipomatosis develops from pancreatitis. To prevent the development of pancreatic obesity, it is necessary to keep the liver, kidneys and other internal organs in normal condition. It is especially important to maintain the normal functioning of the liver and biliary tract.
It is very difficult to tell about any specific pancreatic disease based on symptoms. Since the same symptoms or similar symptoms may indicate not only the presence of pancreatic disease, but also problems in other internal organs of a person.
As practice shows, with problems with the pancreas, a person’s appetite worsens and body weight decreases. However, symptoms alone are not enough to make a diagnosis. If you notice any symptoms, you should definitely consult a doctor. After undergoing an ultrasound of the pancreas, x-rays and computed tomography, the doctor will be able to make a conclusion and make a diagnosis.
Today, there are a number of symptoms indicating pancreatic disease. In this article we will analyze them in as much detail as possible.
Pain syndrome
Pancreatitis is inflammation of the pancreas.
If there are problems with the pancreas, this will certainly affect your well-being.
Pain syndrome will develop quite quickly, which is the main symptom of a disease such as pancreatitis. With a chronic disease, the pain will be more noticeable, prolonged and intense.
In general, in the chronic form of pancreatitis, the pain syndrome is less pronounced, and in 15% of patients it does not manifest itself at all.
After some time (approximately 5-15 years), the pain may disappear altogether. This is due to the fact that over time the nerve endings simply die off. In parallel, diabetes mellitus or steataria may develop. The formation of pain can be influenced by a large number of indicators, for example:
- Ischemia
- Swelling
- Inflammation of the pancreas
The combination of these factors disables the organ, disrupting its functions. It is because of this that the pressure of pancreatic juice increases and pain occurs.
In general, such a symptom as pain is expressed only in the first 5 years of the disease, and then every year the number of painful attacks will decrease.
The presence of pain in the pancreas can indicate not only pancreatitis, but also other diseases. Quite often, pain indicates the formation of pseudocysts, which grow and compress the duodenum and bile ducts. As a result, pain occurs.
The most common complaint among patients is pain in the epigastric region. The location of pain will depend on which part of the pancreas is damaged. The pain may shift to the chest area, while echoing the pain in the groin or back.
Typically, pain appears and intensifies half an hour after eating. Especially if the food was unhealthy (spicy, fried, smoked or fatty). In addition, pain can be caused by alcohol abuse.
If a person is diagnosed with pancreatic necrosis, then he will not experience pain, since this disease causes the death of nerve endings.
Causes of pancreas enlargement
There are two reasons for detecting an enlarged pancreas:
- tissue proliferation to compensate for the reduced functions of individual cells;
- tissue swelling due to inflammation or an autoimmune reaction.
Therefore, the main factors for organ enlargement are:
- alcohol abuse;
- chronic infections;
- blockage of the Wirsung duct;
- intoxication with drugs and chemical agents;
- autoimmune process.
alcohol abuse
An enlarged pancreas can be associated with dangerous conditions:
- an abscess is a cavity containing pus, which affects the functions of the entire organ and increases the risk of sepsis;
- epithelial cysts are usually benign, but cause pain by stretching the organ capsule;
- pseudocysts are formations that contain remains of cells or enzymes and other fluids, which increases the size of the organ and impairs its function;
- cancer causes severe pain that radiates to the back. Its symptoms are associated with stool disorders and uncontrolled diabetes mellitus.
Most often, an enlarged pancreas is caused by chronic inflammation - pancreatitis. Alcoholism and other intoxications, including excess calcium and fats, are the main mechanisms of the pathology.
Dysfunction of the sphincter of Oddi is manifested by reflux of duodenal contents into the pancreatic duct, which leads to an inflammatory process. Then changes begin in the form of autolysis - tissue breakdown. The prerequisites for the disorder are: removal of the gallbladder, compression of the vagus nerve at the level of the cervical spine or diaphragmatic opening - a stress factor, as well as gastritis.
Sphincter of Oddi dysfunction
A dangerous autolytic effect occurs when the destructive effects of the gland's own enzymes are directed against its own tissues. Self-destruction of the organ is observed.
Enlargement of the gland is provoked by spasm of the arteries and ligaments. Compression of the diaphragm changes the position of the stomach and duodenum, as a result the head of the pancreas is pinched, and the outflow of secretions slows down.
At the same time, biliary dyskinesia, cholelithiasis or gastritis are diagnosed as a concomitant or underlying pathology. With severe dysfunction of the liver, worms and helminths can disrupt the functioning of the hepatobiliary tract.
Chronic pancreatitis is considered one of the factors affecting the intestinal papilla by tumors, in addition to genetic predisposition. Enlargement of the tissue of the head of the pancreas due to an abscess or adenoma leads to compression of the common bile duct, which is manifested by jaundice. Islet cell tumors are called insulomas and are found in the tail with local enlargement of the pancreas. Symptoms include hypoglycemia, drowsiness, and sweating.
The child has a stomach ache, bad breath, lethargy and vomiting - these are signs of increased acetone. This is caused by the accumulation of ketone bodies in the blood due to impaired protein or carbohydrate metabolism, liver enzyme deficiency or endocrine dysfunction. Acetonemic syndrome indicates pancreatic dysfunction and enlargement.
The release of pancreatic enzymes into the intestine is affected by the acidity of the stomach. Hydrochloric acid sends a signal to produce secretion. Low acidity increases the risk of stomach cancer caused by chronic gastritis.
The reasons for an enlarged pancreas in a child are usually sought in heredity. Osteopaths view the dysfunction as a consequence of cranial compression during childbirth and decreased vagus nerve signals. It descends along the neck and chest, innervating the organs on its side of the body.
enlarged pancreas
The cause of an enlarged pancreas in an adult is the accumulation of fat, lipomatosis or steatosis. The pathology is associated with type 2 diabetes mellitus, acute pancreatitis, and oncology. An MRI examination is required for differential diagnosis.
Intoxication syndrome
Pancreatic diseases can lead to weight loss.
Intoxication syndrome is characterized by the following indicators:
- Tachycardia
- Fever
- Lower blood pressure
- Weight loss
- General weakness
- Increased ESR and erythrocyte content
There are cases when, based on the intoxication syndrome, an intoxication psychosis is formed. This is due to swelling and hypoxia of the brain and damage to its blood vessels. This often happens in people who abuse alcohol and have liver disease. Intoxication psychosis can manifest itself in the form of euphoria, fussiness or hand tremors.
Such symptoms need to be responded to immediately. After all, if no measures are taken immediately, psychosis will progress. At first, there will be sharp emotional arousal, hallucinations or convulsions. And then there is a suppression of motor and psychological activity, as a result of which the person simply falls into a stupor.
Trophological deficiency syndrome
Diarrhea is one of the symptoms of pancreatic disease.
This syndrome occurs when digestion is impaired due to enzyme deficiency. It is noteworthy that the main indicators of trophological deficiency syndrome are:
- Atrophy of subcutaneous fat in the abdominal area
- Darkening of the skin color at the location of the pancreas
- Rapid weight loss
- Psychological disorder
- Visual impairment
- Skin turning gray
- Loss of coordination
- Exocrine disorder syndrome
If a person develops a disease of the pancreas, which is accompanied by exocrine insufficiency, then this disease will be very difficult to resolve.
This is explained by the fact that with exocrine insufficiency, up to 90% of the parenchyma dies, and, as a result, there is a reduced production of enzymes involved in the metabolic process. There are several symptoms of pancreatic disease caused by decreased excretory function:
- Diarrhea
- Steatorrhea
- Exhaustion
This video will tell you about pathologies of the pancreas:
https://www.youtube.com/watch?v=QsOoCbB0MJY
There are a number of diseases that are accompanied by a violation of the exocrine function of the pancreas. For example:
- Chronic pancreatitis. Characteristic features of this disease are weight loss and the development of steatorrhea, and quite often this disease provokes the development of diabetes mellitus.
- Cystic fibrosis. An autoimmune disease in which there is a high probability of developing exocrine insufficiency, and, as a result, the formation of cysts and atrophy of the pancreas.
- Shwachman's syndrome. Characterized by decreased production of trypsin and lipase. There is a failure in the development of the skeleton and bone marrow neutropenia.
- Pancreatic resection. Doctors decide to remove the pancreas if a chronic form of pancreatitis with increased intraductal pressure is detected, as well as with necrosis or cancer of the pancreas.
Pancreatic atrophy
Pancreatic atrophy is a condition characterized by a decrease in the size of the organ, compaction of its structure and insufficiency of functions. This process can develop as a result of physiological age-related changes, as well as diseases accompanied by damage to the parenchyma, compression, impaired blood supply, and long-term debilitating diseases. In this case, the weight of the gland, which is normally about 80-90 g, decreases to 30-40 and below. The structure of the pancreas changes, characterized by excessive development of connective tissue, which can proliferate around the lobules (perilobular sclerosis) or diffusely (intralobular sclerosis). A peculiar type of atrophy is lipomatosis, in which most of the organ parenchyma is replaced by adipose tissue.
Organ compression syndrome
An enlarged pancreas can cause itchy skin.
There are a number of symptoms that are a consequence of an increase in the size of the pancreas or nearby organs. This is often expressed like this:
- Development of obstructive jaundice
- Itchy skin
- Enlarged spleen
- Vomit
- Dark color of urine
- Lightening the color of stool
This syndrome develops with complications of pancreatic disease: complications of chronic pancreatitis, cancer, formation of pseudocysts. Compression of the duodenum is possible, which provokes the formation of intestinal obstruction. This is accompanied by such indicators as:
- Frequent and profuse vomiting
- Dehydration
- Development of trophic insufficiency
Compression of the portal and splenic vein provokes the development of pancreatic ascites.
Why is the pancreas needed?
Located deep in the abdomen between the stomach and the spine, the pancreas is a flat, leaf-shaped gland. The pancreas is divided into three parts: the wide end is called the head, the thin end is called the tail, and the middle part is the body.
The pancreas produces insulin, a hormone that regulates blood sugar levels. When the body stops producing insulin, blood sugar levels rise. The pancreas also produces digestive juices that help the body break down and absorb food. The part of the pancreas that produces digestive juices is called the exocrine pancreas, and the part of the pancreas that produces insulin is called the endocrine pancreas.
Enzymes pass through the pancreatic duct into the duodenum. The liver and gallbladder also produce digestive juices and other chemicals into the duodenum that allow the body to absorb food.
Other syndromes
With chronic pancreatitis, the patient may experience headaches.
Neurasthenic. This syndrome develops with chronic pancreatitis. Expressed in:
- In general weakness
- Insomnia
- Hot temper
- Headaches
- Motor retardation
Dyspeptic. Regarding this syndrome, it can be noted that it is manifested by the following indicators:
- Change in appetite
- Vomit
- Belching
- Flow of saliva
- Flatulence
Cholestatic. Characteristic features of this syndrome are liver enlargement, as well as the development of jaundice and skin itching. Pancreatocardiac. In this case, the signs will be as follows:
- Reduced pressure
- Rapid heartbeat
- Muffled heart tone
Thrombohemorrhagic. The name speaks for itself. Thrombohemorrhagic syndrome is characterized by the formation of blood clots in blood vessels.
To avoid pancreatic disease, you need to carefully monitor your health. Eat healthy food and visit the clinic regularly for check-ups. After all, it is better to prevent a disease than to treat it later.
We hope that this article will serve as an excellent source of information for you. And after reading it, you will decide to undergo a medical examination. And remember that self-medication can lead to disastrous consequences. Good health!
- ← On which side does the pancreas hurt?
- Why does stage 4 pancreatic cancer occur and how it progresses →