Origins of the problem
With gastric hyperplasia, cells divide and multiply in increased numbers. Moreover, in the advanced stage of the disease, changes begin in the cells themselves. They turn malignant. What causes cells to multiply so rapidly? There may be several reasons:
hormonal imbalances in the body;
advanced chronic inflammation in the digestive organ - gastritis, polyps, ulcers;
stomach infections that have not been completely cured;
impaired nervous regulation of the digestive organ;
regular exposure of the stomach to all kinds of carcinogens (including from smoking and alcohol);
a hereditary component that promotes the proliferation of epithelial cells.
If you suspect hyperplasia, you should immediately consult a doctor. And if an illness is detected, treatment must begin immediately.
Reasons for the development of various forms of hyperplasia
Hyperplasia is caused by various reasons. They are almost all the same for different forms of the disease. The disease can be provoked by:
- Hormonal imbalances in the body.
- The presence of untreated infectious diseases such as gastritis and ulcers.
- Inflammation of various stomach tissues.
- Problems in the intrasecretory work of the organ mucosa.
- Long-term exposure to the gastrointestinal tract of toxic carcinogens.
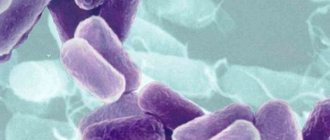
- The presence of microorganisms of the Helicobacter pylori type in the body.
- Disturbed nervous regulation of the digestive system.
- Hereditary factor.
It is very important to correctly determine the cause that provoked gastric hyperplasia. This is what the attending physician will rely on when selecting individual therapy for the patient.
What should you be wary of?
The insidiousness of the disease lies in the fact that hyperplasia is asymptomatic for a long time, so a person does not worry. As a result, when a chronic advanced form of proliferation of the integumentary epithelium of the stomach has developed, treatment begins with a delay. The thin layer of epithelium that lines the walls of the stomach begins to grow rapidly.
How not to be late and seek treatment on time:
any recurring indigestion, stomach pain, heartburn, belching should be a reason to consult a doctor;
You should regularly undergo a preventive examination and medical examination, during which a stool test for occult blood is performed;
If someone in your family suffered from chronic gastritis, peptic ulcer, or hyperplasia of the integumentary pitted epithelium of the stomach, you should also undergo a mandatory preventive examination by a gastroenterologist with appropriate examination.
Here are the signs that begin to worry when epithelial growth is already in force:
cramping and very noticeable pain in the abdominal area due to involuntary contractions;
symptoms of anemia may appear;
it is possible that indigestion may occur during or after a meal;
Pain in the digestive organ also occurs at night on an empty stomach.
To think that this is ordinary, simple gastritis and that everything will go away on its own is naive. Self-medication is strictly forbidden! You need to go to the doctor immediately.
Features of hyperplasia of the integumentary epithelium of the stomach
It is not so easy to detect hyperplasia of the integumentary epithelium of the digestive system. It manifests itself in functional changes that affect the activity of cells in the gastric mucosa. All this can be revealed only during histochemical examination or electron microscopy.
The disease can be detected by the following signs:
- The appearance of small gastric pits.
- Changing the appearance of an organ. It takes a corkscrew shape.
Hyperplasia of the integumentary pit epithelium of the entire stomach requires the same treatment as foveolar type disease. This is despite the fact that the two diseases have different symptoms.
Starts from the hearth
The focus of hyperplasia in the stomach is a polyp in its early development, which has a benign course and is located in one specific place, the focus. Hence the name.
This disease is determined by the endoscopic method and using special dyes. The lesion is immediately colored. It can be large, small, multiple or single. It is usually formed as a result of erosion of the gastric mucosa.
Erosion of the mucous membrane, as a rule, provokes quite noticeable pain. Therefore, those suffering from this disease may experience cramping pain. They recur periodically, often arising as a reaction to provoking foods.
In addition, another sign of the presence of focal hyperplasia is developing anemia. Its symptoms may appear from time to time. And this is also a reason to contact a gastroenterologist.
In the treatment of focal hyperplasia, medications are used, as well as dietary nutrition that completely excludes fats. Medicines are selected depending on the root cause of the disease. In most cases these are hormonal drugs.
Moderate proliferation of the gastric epithelium - what is it?
The wall of the stomach consists of 4 layers: the inner mucosa, the submucosa, the muscular layer and the outer serosa.
The mucous membrane (MS) is normally folded, it has depressions - pits, flat areas (fields) and folds.
The mucosal epithelium is highly prismatic (columnar) cells that line the entire stomach and all its folds in one layer.
The cells of this epithelium secrete special mucus; it forms a layer up to 1-1.5 mm thick.
During the production of enzymes and hydrochloric acid, temporary channels are formed in this layer. Mucus protects the wall from digestion by stomach juice and various damage.
The epithelium is renewed every 1-3 days.
What is proliferation
Cell proliferation is a normal process necessary for the body to renew itself. In other words, this is the physiological reproduction of cells with the result in the form of an increase in tissue volume. This process is controlled by hormones. Proliferation occurs in any organ and tissue.
It controls the state of the immune system, leads to the destruction of tissue defects, regenerates them and restores the previous functioning of organs.
Due to proliferation, connective tissue grows, new vessels are formed, burns are scarred, damage is eliminated, tissue is replaced with new cells or connective tissue.
This applies to blood cells, epithelium and mucous membranes, cartilage, myocardial walls, etc. The most active process occurs in the gastric mucosa.
But proliferation under certain conditions can become pathological, that is, excessive. For example, with increased concentrations of somatropin, it leads to enlargement of organs and limbs. If cell differentiation is disrupted during the process of proliferation, this becomes the beginning of oncology with the appearance of atypical growths.
This uncontrolled active (abnormal) cell division is called hyperproliferation or hyperplasia.
This can also be explained by the predominance of proliferation over differentiation of mucosal cells. Then the number of narrowly differentiated cells decreases and the epithelium begins to lose its “legal properties” due to immature cells.
Proliferation of the integumentary epithelium can and is often accompanied by processes of intestinal metaplasia of the stomach.
Hyperplasia
Proliferation of the integumentary pitted epithelium of the stomach is one of the subtypes of mucosal proliferation. The name is given because as a result of tissue growth, corkscrew-shaped pits are formed.
This proliferation means hyperplasia of mucus-producing cells (goblet cells), which play a protective role.
The integumentary epithelium undergoes mutation, the content of mucin in the cells increases, pushing the nuclei to the base of the cell, pathological cells begin to replace healthy ones.
Pits form in the mucosa, which are shaped like a corkscrew pin. The process is a harbinger of oncology.
Most often, proliferation of the integumentary pitted epithelium occurs with hyperplastic gastritis, peptic ulcer disease, and ulcer-like cancer. Clinically and morphologically, they are identical, so a biopsy is required.
Cytological examination can reveal pronounced proliferation of the integumentary pitted epithelium of the stomach.
In fact, this is a precancerous condition, and such patients should be registered with an oncologist and undergo a systematic examination.
Reasons for development
the cause is chronic or long-term damage and irritation of the mucous membrane, which causes the appearance of wounds and ulcers.
In addition to the above pathologies, the cause may be:
- hereditary predisposition;
- hormonal imbalances;
- the presence of Helicobacter pylori - its waste products contaminate the entire body, which suppresses the immune system, destroys the mucous membrane and causes proliferation of the integumentary pitted epithelium; this bacterium leads to inflammation of the gastric mucosa and the development of gastritis in 90% of cases;
- nutritional disorders, which contain a lot of E additives, preservatives, alcohol;
- taking NSAIDs;
- stress;
- changes in the functioning of the duodenum (it provokes excess gastrin, which irritates the gastric mucosa; backflow of bile during reflux) and the pancreas.
Classification
Several types of gastric hyperplasia have been identified. They differ in type and areas affected.
The main ones include the following:
- antral;
- focal;
- foveal;
- glandular;
- polypoid;
- lymphofolicular;
- proliferation of the integumentary pitted epithelium of the stomach;
- lymphoid.
Briefly about the types
There are the following types of pathology:
- Foveal hyperplasia of the stomach. In this case, the folds and gastric pits are deformed, they are elongated and curved. The most common and harmless type. Develops when taking NSAIDs.
- Antral - tissue grows at the junction of the gastric mucosa and duodenum. The cause is malnutrition. These changes look like multiple small growths.
- Lymphofollicular - the mucous membrane thickens and grows due to the accumulation of lymphocytes that form follicles. Possible malignancy. With lymphoid hyperplasia, the antrum of the stomach is most often affected, when the number of lymphocytes in the lymph nodes increases. With an increase in lymphocytes, the mucous membrane thickens and hyperplasias. Moreover, the enlargement of lymph nodes in this case is not inflammatory in nature. Causes: peptic ulcer and infectious diseases of the digestive tract.
- Glandular is the rarest form, with the proliferation of glandular cells and the formation of round and oval polyps. Occurs when the stomach stretches.
- Polypoid – the appearance of multiple polyps in any part of the stomach. The reason is unknown.
- Focal – “wart” – the appearance of additional tissue in one or several places. The process is observed in the initial stages of hyperplasia and is benign.
That is, we can say that the proliferation of cells of the integumentary pit epithelium is the proliferative growth of cells that produce mucus.
Degrees of proliferation
Today, hyperplasia is divided into 3 stages:
- First degree – mucus production decreases, hyperchromatosis is noted. The process is initial, it is reversible with proper treatment.
- The second degree is moderate proliferation of the integumentary pitted epithelium. The process is already more obvious, cell division accelerates and becomes more frequent, the number of Paneth and goblet cells decreases. The process can still be stopped with timely and modern treatment.
- The third degree is pronounced proliferation of cells of the integumentary pit epithelium of the stomach. Large areas proliferate, mucus is not secreted, there is no protection, the process becomes precancerous.
Foveal, lymphoid, glandular hyperplasia
During an endoscopic examination, an asymptomatically developing disease, foveolar hyperplasia of the stomach, can be discovered completely by accident. The foveal form of the disease is the uncontrolled proliferation of cells in the mucous membrane or tissues of the digestive organ. It leads to curvature and thickening of the folds of the mucous membranes of the stomach, lengthening its sections. The disease does not form either a malignant or benign tumor. But it is the initial stage to the development of hyperplastic polyps.
Lymphoid hyperplasia leads to inflammation of the lymph nodes.
Glandular hyperplasia leads to the formation of growths in place of the internal glands.
Polyp-like hyperplasia occurs with the formation of polyps, which can affect not only the digestive organ, but also the intestines.
Forecast and some recommendations
The most favorable prognosis occurs when the disease is detected in a timely manner and urgent measures are taken to prevent further growth of the gastric mucosa.
No less important is the type of disease and the degree of its intensity.
If you strictly follow all the doctor’s recommendations, it is usually possible to bring the pathological process under control.
In addition, the following instructions from specialists in diseases of the digestive system must be observed:
- Diagnose any disorders in the gastrointestinal tract in a timely manner.
- Get tested regularly for H. Pylori.
- Monitor prescribed therapy.
- Stabilize the pH level of gastric juice.
- Follow the diet strictly.
- Give up bad habits forever.
- Chew food thoroughly.
- Watch the chair.
- Normalize the activity of the nervous system.
Follicular problem
Follicular hyperplasia of the stomach is also disguised as other diseases in the early stages. But this type of disease is insidious in that it can unnoticeably develop into a malignant form. It should be noted that follicular gastritis is quite rare - one in a hundred. What it is is when white blood cells accumulated at the site of mucosal damage transform into follicles.
The cells grow gradually without causing problems. And only when there are a lot of these cells does the patient experience painful and unpleasant sensations. The following symptoms should alert you:
seemingly causeless increase in body temperature;
weakness in the body;
occasional pain in the digestive organ.
Treat - and nothing else
Gastric hyperplasia requires long-term treatment. This includes both diet and medication. The most successful solution is surgery.
Drug treatment is:
drugs to reduce gastric acidity (antisecretory drugs - PPIs: Omez, Rabeprazole, etc.);
in the presence of Helicobacter, antibiotics are prescribed that destroy the pathogens that cause the disease (first- and second-line treatment regimens or the official combination drug - Pilobact or Clatinol);
drugs for the treatment of other gastric pathologies that were identified during the examination);
following a strict diet prescribed by your doctor.
The diet involves eating protein, but the food should not be fatty. You will have to eat fractionally and little by little. Depending on the severity of the disease, the causes of its occurrence, the doctor will determine a number of products necessary for health and healing, and will also tell you which ones are not recommended.
Surgical treatment is sometimes inevitable, but the only effective solution. Surgery is prescribed when the proliferative processes do not stop even after taking medications.
Gastric hyperplasia is a benign disease characterized by pathological proliferation of stomach cells. Due to the increase in the number of cells, the mucous membrane of the organ thickens and polyps appear. Pathology can occur not only in the stomach: enlargement can occur in any internal organ. The disease manifests itself in any person, regardless of gender and age.
Treatment methods
A drug therapeutic course involves the use of a standard regimen used for all types of disease:
- The use of antibiotics to eliminate inflammation and pain. The most effective are Amoxicillin, Ciprofloxacin, Clarithromycin, Levofloxacin.
- Medicines from the group of inhibitors that help reduce stomach acidity. These are Pantoprazole, Vasonate, Omeprazole.
- Agents that restore the gastric mucosa and its structure, as well as prevent the development of infections and bacteria - bismuth preparations.
In case of a complex form of the disease (for example, polypoid hyperplasia) and the absence of a favorable effect of treatment, surgery is recommended to remove polyps and affected organ tissue.
Therapeutic diet
Compliance with dietary norms is due to the need to minimize the load on the digestive organs. If you have gastric hyperplasia, you should follow diet No. 5. Here are general recommendations:
- fractional meals;
- exclusion of fatty, fried, spicy foods;
- inadmissibility of drinking juices, carbonated and alcoholic drinks;
- preference should be given to products rich in complex fiber, that is, cereals;
- For meat, it is advisable to eat chicken, rabbit, turkey;
- Only low-fat varieties of fish are allowed.
All dishes are steamed, oven-baked, stewed or boiled.
From folk remedies
As a supplement to treatment, you can turn to folk recipes. Here are some medicinal plants that help improve the condition:
- Chamomile is a good antiseptic. In addition, it eliminates muscle spasms and pain.
- Peppermint is a cure for heartburn. Relieves the feeling of nausea.
- Ginger root has antiseptic and antibacterial properties.
Teas prepared on their basis can alleviate the general condition, reduce the inflammatory process and resist various bacteria, which sometimes cause hyperplasia. But relying only on the help of these simple recipes means contributing to the further development of the disease.
Treatment should be comprehensive, based on the recommendations of qualified physicians. It is necessary to strictly follow the doctor's instructions regarding the intended course of therapy and diet. Only with this approach can one hope for a favorable outcome.
Please note that the medications mentioned above are provided for informational purposes only. Self-medication does not help get rid of the disease; it delays the healing process and can lead to irreversible consequences when medicine is powerless.
Etiology
Gastric hyperplasia develops due to unfinished treatment of diseases of the gastrointestinal tract. As a result, active cell growth begins and polyps appear.
The main causes of hyperplasia:
- changes in hormonal balance, especially when the amount of estrogen is increased;
- genetic predisposition, in particular adenomatous polyposis (characteristic of polyps in the stomach) - if the pathology is diagnosed in a woman, the disease can be inherited by a daughter or granddaughter;
- long-term use of medications that can affect changes in the structure of the gastric mucosa;
- unfavorable environment - a pathological increase in the number of cells may begin.
The cause is the bacterium Helicobacter pylori and other infectious diseases.
The role of nutrition in the treatment of pathology
In case of gastric hyperplasia, a special role must be given to nutrition. In most cases, the disease develops as a result of poor nutrition. It is imperative to adjust the diet, otherwise the therapy may not give any result.
Patients with any form of hyperplasia, including focal hyperplasia, must follow the following food intake rules:
- You need to eat food in small portions - no more than 200 g at a time. Eat often - up to 5-6 times a day.
- Consume only foods that do not irritate the gastric mucosa. It is useful to include any cereals, lean meats and fish, fruits and vegetables in your diet.
- It is advisable to cook food by steaming, baking in the oven, boiling or stewing.
- You can only eat warm food. Too cold or hot food can negatively affect the condition of the mucous membrane.
- Eliminate fried, spicy, smoked and pickled foods from your diet. Such dishes irritate the gastric mucosa, so they can slow down recovery.
If a person is diagnosed with hyperplasia, he must be prepared for the fact that he will have to follow a diet according to the above rules throughout his subsequent life. This will help prevent relapse in the future.
Classification
In medicine, experts distinguish between many different types of hyperplasia:
- Focal developing hyperplasia of the gastric mucosa. The first stage of development of the anomaly, when certain polyps begin to appear. Focal diagnosed hyperplasia of the stomach covers only some areas (“foci”), which is why it got its name. The lesions look like growths of various shapes and sizes, painted in a different color, so they are clearly visible during examination. Formations arise at the site of previously received damage or erosion.
- Follicular identified gastric hyperplasia. This type of pathology is often diagnosed. Lymphatic cells begin to grow. The reasons for the development of the anomaly are different: the influence of carcinogens, hormonal imbalance, the presence of the bacterium Helicobacter pylori, stressful situations and much more. A distinctive feature of this type of disease is the formation of follicles in the stomach.
- Hyperplasia of the integumentary pitted epithelium of the stomach. A dangerous type of pathology that can contribute to the appearance of a malignant tumor in the intestine. The structure of the epithelium changes under the influence of unfavorable factors: cells grow and become larger.
- Hyperplasia involving the antrum of the stomach. The antrum is the last part of the organ before it exits into the intestine. In this place, with the development of hyperplasia, multiple small growths, pits and ridges begin to form.
- Foveal hyperplasia of the gastric mucosa. This type of pathology is characterized by an increase in the length of the folds of the mucous membrane and an increase in their curvature. Pathology occurs due to prolonged inflammation or self-administration of anti-inflammatory drugs.
There are also other types of pathology: glandular, polypoid, lymphoid.
Reasons for development
The main reason is prolonged irritation of the mucous membrane, leading to injuries and wounds. The reasons are:
- Chronic diseases (gastritis, ulcers and other inflammations) and advanced infections (intestinal, rotavirus). Excessive division is a defensive reaction to the aggressor. For example, against the background of chronic lymphoid gastritis (focal accumulation of lymphocytes in the epithelium in the form of follicles), lymphofollicular hyperplasia of the stomach of the 1st degree may develop. It is important to note that it begins to manifest itself only from stage 3, before which it can be detected by chance during FGS.
Various inflammatory processes in the stomach can lead to hyperplasia
- Predisposition at the genetic level.
- Hormonal imbalance or formation affecting hormones. For example, a pancreatic tumor provokes excess acid production in the stomach, to which the organ responds with additional cell proliferation.
- The parasite Helicobacter pylori is a bacterium that contaminates the body with its waste products, weakening its defenses and destroying the upper layer of the stomach, gradually penetrating deeper. It is fraught with the development of the most dangerous type - hyperplasia of the integumentary pitted epithelium of the stomach. Structural and secretory changes occur, and cancer may develop.
- Unhealthy diet, which is dominated by additives, preservatives, carcinogens (additives of group E), excessive addiction to alcohol.
- Long course of taking non-steroidal drugs.
- Stress, regular overexertion.
- Impaired functioning of the parasympathetic nervous system and secretory function of organs. Changes in the functioning of the duodenum provoke the release of gastrin, which irritates the mucous membrane. Against this background, lymphofollicular hyperplasia of the antrum of the stomach can develop.
Stress can also trigger this disease
Symptoms
In the first stages of the development of the disease, it is very difficult to identify the pathology, because there are practically no symptoms: an increase in the number of cells does not cause discomfort to a person, there is no pain even when small polyps appear. When they increase, difficulties begin with the passage of food, which can cause severe bleeding or pain.
As the disease progresses, disruptions in the functioning of the stomach begin, and these are problems with digestion. The following symptoms begin to appear:
- constant or short-term pain that occurs after eating, sometimes during prolonged fasting;
- heartburn;
- flatulence and constipation;
- sour belching;
- nausea and vomiting;
- refusal to eat;
- general weakness, body aches, dizziness;
- anemia.
If such symptoms occur, you should consult your doctor so that the doctor can prescribe an examination.
Diagnostics
During the examination, the medical officer collects the patient’s medical history and clarifies the complaints. It is impossible to establish a correct diagnosis using these data alone. Other studies are prescribed:
- gastroscopy - using an endoscope tube inserted into the stomach, the walls of the organ and polyps are examined;
- biopsy - a histological examination will establish an accurate diagnosis; using the procedure, the type of pathology and the main cause of the development of the anomaly are determined.
After an accurate diagnosis is made, effective treatment is prescribed.
Treatment
Gastric hyperplasia is treated by a gastroenterologist. If necessary, the patient may be scheduled for a consultation with an oncologist or surgeon. Surgery is performed only in extreme cases; usually the treatment regimen is limited to taking medications.
- Drug therapy. Treatment of gastric hyperplasia is aimed at eliminating the underlying cause of the pathology. If the anomaly has developed due to a bacterial infection in the body, the person is prescribed antibacterial drugs. To protect the mucous membrane, the doctor prescribes gastroprotectors. A gastroenterologist may prescribe medications to reduce acidity if the patient's test results show an elevated pH. The doctor prescribes hormonal medications when the disease is associated with hormonal imbalances.
- Carrying out surgery. If too many polyps of a significant size appear, the growths may need to be removed. Usually limited to endoscopic polypectomy. In severe cases, open gastric surgery is performed or part of the stomach is removed.
- Diet. The patient must adhere to dietary nutrition. You can only eat food that does not harm the mucous membrane. The menu will depend on the primary disease that caused the pathology. Fractional nutrition is suitable for any patient with such a deviation, regardless of the cause of the development of the anomaly. There should be up to 5 meals per day, small portions. List of products whose consumption is not recommended: alcohol, strong tea, coffee, carbonated drinks. Lean fish and meat, cereals are useful. It is better to cook if the food is steamed, stewed or boiled. Fried and spicy foods should be excluded from the diet. Hot dishes cannot be eaten. A strict diet will help you recover faster.
- Traditional medicine recipes. Can only be used in combination with traditional medicine after consultation with a doctor.
Treatment and diet
It is important to follow a diet.
Treatment of hyperplasia in the stomach can be carried out with medications, diet or surgery, or traditional medicines. The basis of treatment for hyperplasia is nutrition, since poor nutrition is the most common cause of the development of the disease. It is impossible to get rid of pathology without a diet.
The diet should not contain junk food, especially those containing carcinogens or harmful fats. The mode of eating is important. You need to eat small portions (200 g) 5-6 times a day. It is better if the patient’s diet is prepared by a specialist based on blood tests. It is recommended to lead an active lifestyle.
Therapy with pharmaceuticals consists, first of all, in eliminating the causes that provoked the development of hyperplasia. Most often, hormonal therapy is prescribed, with the help of which adequate cell division is restored. If the disease is caused by Helicobacter, antiviral agents are prescribed.
If therapy does not help, another such course may be prescribed. If the patient does not feel better after the second course of treatment, the doctor may recommend surgery. If a patient is diagnosed with hyperplastic polyps (foveal type of disease), the size of which is more than 10 mm, they must be cut out, as there is a danger that they will transform into oncology. After such an operation, the surrounding tissue is taken for histological analysis.
During surgery, the polyp and tissues in which there is abnormal division at the cellular level are excised. Surgical treatment is not performed often. Most often, conservative therapy helps. Treatment is carried out until the patient fully recovers.
Treatment with traditional methods
After consulting a doctor, you can include traditional methods in the treatment of hyperplasia in the stomach. Folk remedies can be used as auxiliary methods. A decoction of St. John's wort is useful in the treatment of the disease. To prepare it, you need to pour a tablespoon of the plant into a glass of just boiled water and let it sit for 120 minutes. After this, filter the broth. Drink a glass twice a day.
It is useful to drink sea buckthorn oil. To get the maximum effect from the beneficial properties of this folk medicine, you need to take 5 ml of sea buckthorn oil before meals.
You can treat hyperplasia with folk remedies such as decoctions of parsley roots. To prepare, you need to grind the roots of the plant and steam it in a glass of boiling water. The medicine should stand overnight, after which it is filtered. Take a spoonful of the decoction 5 times a day.
Another useful grandmother's recipe is horseradish with honey. Grind the horseradish and place in a glass jar. Eat horseradish before meals, one teaspoon at a time, adding honey. Horseradish promotes the production of enzymatic juice and destroys tumors. Treatment of hyperplasia with folk remedies is not complete without massage. The procedure is not difficult to perform. To do this in the morning, without getting out of bed, you need to massage the abdominal cavity clockwise. It is necessary to do at least 60 circles.
Another recipe for the disease is a decoction of onion peels. A glass of husk should be washed and steamed in 500 ml of boiling water. Then simmer over low heat for 5-10 minutes and let sit for a little less than an hour. The broth is filtered and honey is added to it when cooled. You need to take 100 ml of the decoction three times a day for 5 days. After this, take a break for 5 days and repeat. The pharmacy sells a herbal mixture for hyperplasia. Contains celandine, linden, St. John's wort and chamomile. It is recommended to drink it as tea.
Prevention
Basic preventive measures for hyperplasia:
- healthy and balanced diet;
- active lifestyle;
- rejection of bad habits;
- use of medications only as prescribed by a doctor;
- regular preventive examinations;
- urgent treatment of gastric diseases.
Depending on the area of intestinal damage, the gastroenterologist will recommend individual methods of prevention to the person. Self-medication is excluded - you need to consult a doctor at the first symptoms of pathology.
Important! A remedy for heartburn, gastritis and ulcers, which has helped a huge number of our readers. Read more >>>
Hyperplasia is a pathological growth of any tissue as a result of increased cell division. This process can develop in different organs of the human body: in the uterus, in the adrenal glands, in the mammary glands, but hyperplasia of the gastric mucosa is most often observed. Hyperplasia is considered a dangerous process, since rapid cell division and growth can lead to the appearance of tumors.
Sometimes hyperplasia leads not only to an increase in the number of cells, but also to structural changes in them, which is the beginning of the process of formation of a malignant tumor. At the same time, cell division during hyperplasia does not differ from normal division, their number simply increases sharply. Structural changes in cells are observed already at advanced stages of the disease.
As a result of hyperplasia, the mucous membrane grows; it can be either diffuse or focal.
There are a large number of types of gastric hyperplasia. The classification is based on the location of the pathology in the organ, as well as on what type of cells is involved in the pathological process.
What is hyperplasia of the gastric mucosa?
Hyperplasia is a disease that can affect any internal organ of the body, but most often in practice it is gastric hyperplasia that can be encountered.
The disease is quite complex and requires a quick solution to the problem, and self-medication in a particular case is simply impossible! Hyperplasia is an accelerated intensive growth of cells of the stomach and adjacent tissues. Reproduction occurs by cell division, that is, naturally. Gastric hyperplasia is a pathology of the mucous membranes of the stomach, the result of which is a sharp increase in the number of cells of mucous tissue. As a result of such rapid cell growth, the walls of the stomach thicken and polyps (small tumors) appear.
At more serious stages of the development of the disease, changes occur in the structure of the cells themselves, and this is direct evidence of the beginning of the development of a malignant tumor. Hyperplasia is not a clinical diagnosis, but only states histological changes in the gastric mucosa. There are many forms of hyperplasia.
Causes and signs of gastric hyperplasia
The causes of gastric hyperplasia (as well as similar processes occurring in other organs) are currently not well understood. Probably, a variety of factors can lead to the development of such processes. Among them are the following:
- disruption of hormonal regulation of the stomach;
- various infections (for example, Helicobacter pylori);
- disorders of the nervous regulation of the stomach;
- genetic predisposition to such pathologies;
- exposure to substances with carcinogenic properties;
- inflammatory processes;
- gastritis or ulcers;
- dysfunction of secretory function.
Hyperplasia of the gastric mucosa often occurs without any obvious symptoms and does not in any way affect the patient’s quality of life. This often happens in the initial stages of this disease.
Advanced stages of the disease have clearly expressed symptoms. First of all, these are pain sensations that can appear immediately after eating or, conversely, after prolonged fasting. Patients often complain of heartburn, constipation, and belching.
The reason for the appearance of such symptoms is very simple: hyperplasia causes disruption of the functioning of the stomach, which causes a wide variety of digestive problems.
In general, it should be noted that this pathology is very difficult to diagnose; it is most often possible to determine it in the later stages of development or by chance, during a routine examination.
Symptoms of both types of hyperplasia
In the initial stages, the disease does not make itself felt. A person remains in good health, so he does not worry about his health again. Complaints begin to appear only after hyperplasia of the digestive organ begins to progress at an accelerated pace. This happens if a person continues to lead the same lifestyle that led to such an illness.
In later stages, the disease can be recognized by the following signs:
- Severe pain in the upper abdomen, where the stomach is located. Unpleasant sensations are caused by involuntary muscle contractions. The pain can be either temporary or permanent.
- Stomach dysfunction.
- Anemia cannot be ruled out.
When stomach pain occurs, many people try to suppress it with painkillers. But in this case you can’t do that. You should immediately contact a specialist so that he can find the cause of the discomfort and offer suitable treatment. This is especially important in the case of hyperplasia, since pain indicates its rapid development.
Types of disease
There are many types of gastric hyperplasia. Different types of this disease have differences in pathogenesis, affecting different parts of the stomach and different types of cells of its mucous membrane.
Focal gastric hyperplasia
Focal hyperplasia of the stomach is characterized by damage to clearly limited areas of the mucous membrane of the organ. This type of disease is considered an early type of polyp; the focus of the disease can have a different shape and size. Usually this is a small growth, the structure of which is modified. Such lesions are very well stained and stand out against the background of healthy tissue of the gastric mucosa. This property is used to diagnose this disease.
Focal gastric hyperplasia may have a single lesion or be accompanied by multiple focal lesions. Such lesions may have the appearance of a tubercle or have a stalk. Sometimes focal hyperplasia is called warty.
The appearance of focal hyperplasia is often preceded by damage to the mucous membrane of various etiologies. Often this pathology develops at the site of erosion.
Lymphoid hyperplasia
Another type of this stomach disease is lymphoid hyperplasia, which is characterized by an increase in the number of lymphocytes. Typically, such processes are the result of some kind of infection that activates the body's immune system. But sometimes the proliferation of lymph nodes is the result of pathological processes that occur in the nodes themselves.
In the mucous membrane, under the epithelium, there are a large number of lymphatic vessels and nodes, pathological processes in them cause this disease, which can have different localizations in the organ.
Lymphofollicular hyperplasia
This is a very common disease that is diagnosed in people of different ages, gender, place of residence and eating habits. Lymphofollicular hyperplasia is characterized by excessive division of cells of the lymphatic system, which is located in the mucosa.
Proliferation of the intestinal epithelium: symptoms, causes, treatment, prevention
Intestinal epithelial proliferation is a process of cell growth and division that can be caused by physiological or pathological reasons.
Proliferation cannot be called a disease; it is a normal, natural phenomenon that is necessary for the restoration of cells and tissues.
But if cell division occurs excessively, it is considered a pathology and requires treatment.
What is proliferation?
The cells and tissues of the glandular epithelium of the stomach are systematically renewed, so proliferation does not stop.
It is necessary to control the level of immunity, eliminate existing tissue defects, regenerate and restore their normal functioning.
At the initial stages, cellular growth is regenerative, but over time, with active development, the mucous membrane ceases to recover.
The surface of the epithelial glands is covered with nonspecific cells that have an elongated shape and dark color. In the normal state, such structural elements are located only in the glandular necks.
If the process of cell differentiation is disrupted, this leads to the occurrence of extensive atypical growths. The condition is considered very dangerous, as it leads to the development of cancer - carcinoma.
Causes
Proliferation of the intestinal epithelium develops against the background of trauma and damage, as well as diseases of the digestive tract.
The main causes of the pathology:
- gastritis;
- stomach and duodenal ulcers;
- polyps;
- benign or malignant neoplasms.
Acute and chronic forms of ulcers and gastritis lead to damage to the intestinal mucosa and contribute to accelerated proliferation of the epithelium.
The process is especially often activated with thickening of the mucosa, hyperplasia, and also with polyps.
Symptoms of the disease
In most cases, proliferation of the intestinal epithelium is detected accidentally, during the next medical examination.
The pathological process does not have pronounced symptoms, so diagnosis is most often carried out in late, advanced stages.
As proliferation progresses, it causes the following symptoms:
- Painful cramps in the upper abdomen, which are noticeably worse after eating.
- Attacks of nausea, vomiting.
- Sour belching.
- Bloating , flatulence.
- Hiccups.
- bowel disorder that manifests itself as diarrhea or constipation.
- Deterioration of appetite up to its complete disappearance.
The patient also experiences a deterioration in general health, he is worried about weakness, chronic fatigue, severe headaches and dizziness, increased body temperature, pale skin and other symptoms of general intoxication of the body.
Diagnostics
When detecting proliferation of the intestinal epithelium, it is necessary to identify the exact cause of the pathological process, after which an effective treatment regimen is selected. The main diagnostic measure is gastroscopy, which is combined with a biopsy and further histology of the material taken.
X-rays are also prescribed, which helps to identify polyps in the cavity of the digestive tract. A blood test is performed for the presence of antibodies, an analysis to determine Helicobacter pylori.
Treatment of proliferation
Since proliferation is not an independent disease, but only a symptom of another pathology, medications are prescribed to treat the underlying disease.
For gastritis, gastric or duodenal ulcers, agents are used to restore damaged mucous membranes of the digestive tract.
If the pathological process develops against the background of inflammation, antiviral, antibacterial and anti-inflammatory drugs are used.
Prescribed medications:
- antibiotics – Clarithromycin, Tetracycline, Amoxicillin;
- painkillers - Drotaverine, No-shpa, Papaverine;
- enzymes - Festal, Mezim, Creon;
- antimicrobial – Metronidazole;
- multivitamin complexes.
Treatment of the precancerous form of intestinal epithelial proliferation is complex and lengthy. In most cases, drug therapy is combined with surgery, during which the surgeon excises part of the affected organ or its tissues.
The main indications for surgical intervention are the risk of degeneration of altered cells into cancer cells, the presence of polyps, gastric or intestinal bleeding, and a complicated form of proliferation.
After treatment of the underlying disease is completed, the patient needs to undergo a cytological analysis or biopsy, which will show the effectiveness of therapy and the likelihood of developing a cancerous tumor.
Complications
The main complication of proliferation of the intestinal epithelium is the development of carcinoma - a malignant neoplasm consisting of pathologically altered elongated dark-colored cells.
In addition, proliferation may be accompanied by the formation of polyps and internal bleeding. In the absence of proper treatment, general signs of severe intoxication of the body appear - weakness, apathy, excessive pallor of the skin and mucous membranes.
Forecast
The prognosis for proliferation of intestinal epithelium depends on the stage at which pathological changes were detected. At the initial stages of development, the pathology responds well to treatment.
If treatment is started in a timely manner, proliferation can be eliminated with the help of medications without resorting to surgery.
The precancerous form of the pathology requires surgical treatment. During resection, a specialist removes the affected intestinal tissue.
Prevention
There is no specific prevention of the development of proliferation of intestinal epithelium. Doctors recommend maintaining a healthy lifestyle and giving up smoking and alcoholic beverages. The diet must be complete and balanced, containing all the necessary vitamins and microelements.
Proliferation of the intestinal epithelium is a pathological process that requires mandatory treatment. Therapy helps to normalize the state of the digestive system and prevent the development of such a dangerous complication as carcinoma.
Diagnostics
Several diagnostic methods are used to detect hyperplasia of various types. First of all, this is an x-ray, which can show the contours, shape and size of polyps in the stomach.
The second group of methods that is used to determine this disease is endoscopy. Endoscopic methods include FGDS, colonoscopy, and sigmoidoscopy. If radiography allows you to determine the amount of hyperplastic tissue, then endoscopy allows you to take a biopsy and conduct histological analysis.
Fibrogastroduodenoscopy (FGDS) allows the doctor to visually examine the walls of the stomach and see whether the neoplasm is a polyp or tumor.
Moderate proliferation of the epithelium of the gastric mucosa - Treatment of gastritis
Gastritis is a group of diseases based on inflammation of the gastric mucosa, which develops under the influence of damaging factors.
With different types of chronic gastritis, the etiology, pathogenesis, clinical picture and morphological changes in the mucosa are different.
As a result of exposure to various agents aggressive to the stomach, physiological regeneration of the mucous membrane is disrupted.
Over time, the glandular epithelium atrophies, all functions of the stomach decrease and are disrupted: secretory, evacuation and often endocrine.
The basis of pathogenesis is impaired mucosal regeneration
Violation of the physiological regeneration of the mucous membrane, as research in recent years has shown, plays a major role in the pathogenesis of chronic gastritis.
Normally, surface epithelial cells die under the influence of acidic gastric contents and are completely regenerated every 2–6 days. In this sense, the gastric mucosa is one of the most renewed cellular systems of the body.
Regeneration of the mucous membrane normally goes through two phases:
- cell proliferation;
- specialization (differentiation of epithelial cells).
All etiological and risk factors influence the second phase of regeneration - differentiation (formation of lining and main ones), sharply suppressing it.
The first phase is proliferation (cell reproduction), while the epithelial cells continue to multiply. Defective epithelial cells develop, the number of which increases.
What occurs is not a dystrophic change, but a predominance of proliferation over differentiation of mucosal cells - “malignancy”, when with an increase in proliferation the number of narrowly differentiated cells decreases, and the epithelium loses its morphological and functional properties due to the replacement of differentiated cells with immature ones.
In chronic gastritis, the pathogenesis leading to the fact that the epithelium “does not age” is crucial.
In addition, damage to the mucous membrane is uneven. Initially, the glands and cells of the integumentary epithelium become inflamed. Subsequently, destruction, atrophy or metaplasia of part of the glands occurs.
The surviving cells become “mucused”, structures that are uncharacteristic for the stomach appear and secrete mucus: intestinal metaplasia occurs - areas of the intestinal epithelium in the stomach. Areas of connective tissue and cellular infiltrates appear in the gastric mucosa.
This process progresses rapidly: more in the antrum of the stomach (the bottom of the stomach, where the bulk of the glands are located), less in the body of the stomach.
Reversal does not occur either spontaneously or under the influence of medications.
Polyetiology of the disease
Both exogenous and endogenous factors play a role in the etiology of chronic gastritis. This is a polyetiological process.
Despite the differences in the etiology and pathogenesis of chronic gastritis, the basis of all forms of inflammation of the stomach is damage to its mucous membrane. The etiological factor acts through the blood or affects it directly.
All exogenous and endogenous factors previously considered etiological are now considered risk factors.
Exogenous risk factors:
- food;
- occupational hazards;
- food allergies;
- allergic diseases leading to hypersecretion;
- helminthiases;
- acute pancreatitis and chronic diseases of other gastrointestinal organs;
- chronic infections;
- toxic substances;
- smoking.
Endogenous factors:
- diseases of the cardiovascular, endocrine, respiratory systems, with kidney pathologies, which, in case of circulatory disorders, lead to hypoxia of stomach tissue and the development of gastritis;
- dysfunction of the internal secretion and metabolic organs;
- hypovitaminosis.
Etiological factors, according to modern ideas, are:
- infectious factor: 85 - 90% of gastritis are caused by Helicobacter Pylori - the pathogenesis of the disease and the role of the microbe in it have been proven by numerous studies;
- autoimmune diseases;
- heredity;
- some medications (NSAIDs - non-steroidal anti-inflammatory drugs, hormones, etc.);
- reflux of bile during reflux.
Classification Features
Taking into account the characteristics of the course and clinical picture of chronic gastritis, etiology and pathogenesis, the classification, which was adopted in 1990 in Sydney - the “Sydney system”, is based on histological and endoscopic changes in the stomach.
Later it was modified (in 1994–1996 - Houston modification).
Currently, the classification includes the type of gastritis and three criteria: etiology of chronic gastritis, topography and morphology.
According to the “Sydney system”, which is widely used nowadays, the classification of gastritis is as follows:
- Gastritis type A (autoimmune) - 10 - 15%.
- Type B gastritis (exogenous, caused by Helicobacter Pylori) - 80%.
- Mixed gastritis (type A+B).
- Reflux gastritis.
- Special forms of gastritis: lymphocytic, granulomatous eosinophilic - about 5%.
Another classification is based on changes in the gastric mucosa of a morphological nature:
- Normal mucosa.
- Acute gastritis.
- Chronic gastritis: there are 4 degrees of severity of infiltration by lymphocytes and plasma cells (minimal, slight, moderate, severe).
- Three types of intestinal metaplasia.
Such changes in the mucosa are detected when the disease is diagnosed.
The main method is endoscopic, since it is during esophagofibrogastroduodenoscopy (EFGDS) that the doctor can visually determine changes in the mucosa in all its parts. When a biopsy is taken during EGD, a morphological assessment is made.
Diagnosis of the disease, in addition to questioning, objective examination, medical history and routine tests, includes, in addition to endoscopy, such research methods as fluoroscopy, pH-metry, probing to determine gastric acidity, and determination of Campylobacter.
Treatment
Treatment of various types of gastric hyperplasia can be carried out using drug therapy, a special diet, and also through surgery.
This pathology is very often the result of poor nutrition. Therefore, in the initial stages of the disease, a properly selected diet is a fairly effective remedy. For example, drug therapy may be effective against infections caused by Helicobacter pylori.
Polyps larger than 1 cm should be removed because the risk of them turning into a malignant tumor is very high. Moreover, even after removal of the polyp, a biopsy of the surrounding tissue of the organ mucosa is performed.
A very important factor in the prevention of hyperplasia and various neoplasms in the stomach is the timely treatment of ulcers and gastritis.
Treatment of various forms of hyperplasia of the digestive system organ
When treating the disease, it is impossible to do without drug therapy. Merely following a diet will not achieve any special results, since special nutrition is only an auxiliary means.
Treatment directly depends on the severity of hyperplasia:
- In the early stages, for recovery it is enough to take medications whose action is aimed at eliminating the infection and pathogenic bacteria that have settled in the stomach.
- If the disease progresses to a severe form, which is characterized by the appearance of malignant tumors, then the patient will have to agree to surgery. After the cancerous tumors in his stomach are removed, he will have to take a course of medications. Diet in this case is mandatory.
Only those whose disease was diagnosed in the early stages can manage without surgical intervention. To avoid serious complications and long-term treatment, it is recommended to regularly visit a doctor to examine the gastrointestinal tract for benign and malignant neoplasms. Taking care of your own health will protect a person from serious problems.
Hyperplasia refers to the abnormal activity of cells, which results in their excessive growth and deformation (metaplasia), and the formation of benign formations that can develop into malignant ones (malignization). All organs are susceptible to pathology, but gastric hyperplasia is more common. Literally translated as “overeducation.” All tissues and layers of an organ can change.
Gastric hyperplasia is a fairly common phenomenon.