Gastrointestinal diseases are a common phenomenon among people of all ages. Lymphofollicular hyperplasia of the gastric mucosa is one of the diseases that causes significant discomfort and, in certain cases, leads to complications that can threaten human life. Timely diagnosis of stomach diseases allows you to avoid serious pathologies and disorders.
Etiology
Lymphofollicular hyperplasia of the stomach is an increased proliferation of tissues and cells in the gastric mucosa. This condition occurs as a result of the negative impact of external and internal factors, which, as they influence, modify the structure of the membrane, significantly increasing the number of new cells. The reasons for these changes may be various factors, namely:
- internal secretion disorders;
- hormonal imbalances;
- influence of carcinogens;
- disruptions in the digestive tract;
- the influence of specific tissue breakdown products;
- bacteria Helicobacter pylori;
- constant stress;
- autoimmune diseases;
- hereditary predisposition;
- herpes infection;
- chronic gastritis;
- inflammatory processes in the body.
Hyperplasia of the gastric mucosa is characterized by the formation of an abnormal number of cells and tissues; over time, the follicular tissue of the submucosal layer increases, which leads to the formation of the disease. This process can be triggered by obesity, various liver dysfunctions or hyperglycemia. In medicine, a hereditary factor is considered as a risk of a disease. Active cell proliferation leads to the formation of compactions, diagnosed as gastric polyposis. These accumulations increase over time and can trigger the formation of tumors.
Manifestations of the disease are similar to other pathological conditions and are easy to confuse. Only a specialist can make a diagnosis and prescribe treatment.
Diagnostics
Lymphoid hyperplasia of the stomach or gastrointestinal tract can be diagnosed using instrumental or laboratory methods. The following studies are usually prescribed:
- General blood and urine analysis. With the disease, the level of red blood cells and white blood cells changes.
- Biochemical analysis. Total protein levels change.
- Stool analysis. Blood particles may be present in the excrement, which indicates the presence of a wound in one of the sections of the gastrointestinal tract.
- X-ray. The patient first drinks a barium-based contrast agent, and after this an X-ray or several images are taken in different projections. With such a study, it is possible to detect the exact location of polyps, their size, shape, and the presence of legs.
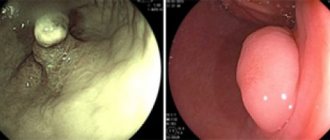
- FGDS. It is a procedure in which an endoscope, a thin tube with a video camera at the end, is inserted through the mouth and esophagus into the stomach. Using such a device, the doctor can see the condition of the gastric mucosa and the presence of tumors in the area. The procedure also allows you to inject the medicine directly into the stomach and even take material for histological examination. Other endoscopic procedures can also be performed if hyperplasia of other parts of the gastrointestinal tract is suspected - colonoscopy or sigmoidoscopy.
- Biopsy. Can be performed during FGDS or during surgery. It involves sampling the affected tissue - a small section of the mucous membrane is taken. Then the taken material is sent for histological examination. This allows you to distinguish hyperplasia from dysplasia, assess the aggressiveness of the pathology - is it benign, is there a likelihood of developing oncology.
- Testing for the presence of the bacterium Helicobacter pylori. To detect it, a breath test with urea and labeled carbon atoms can be performed. The patient drinks this solution. If there is a bacterium in the patient's body, it splits the urea into carbon dioxide and water. By using a special scanner, labeled atoms are detected in the patient's exhaled air. The patient's blood and stool can also be examined to detect bacteria.
A blood test is a method for diagnosing lymphoid hyperplasia of the stomach.
Carrying out MRI and CT scans for gastric hyperplasia is not advisable, since such studies do not directly show modifications of the mucosa. However, with their help you can detect polyps, as well as identify the root cause of the disease.
Types of pathology
The pathology may be of the glandular type.
In medical practice, there are several characteristic types of lymphofollicular hyperplasia, which differ only in the characteristics of their course. The following types are distinguished:
- Focal appearance. It is an early form of the development of polyps, characteristic of certain areas of the mucosa. It appears as a slight growth with a changed structure. Upon careful examination, both single and multiple outgrowths are determined.
- Lymphoid. A significant increase in the number of lymphocytes, which pathologically change the structure of tissues. It occurs as a result of the penetration of viruses into the blood, provoking a reaction from the immune system.
- Lymphofollicular hyperplasia. Consequences of the negative influence of factors on flora and soft tissues, leading to cell proliferation.
- Hyperplasia of the integumentary epithelium of the stomach. A dangerous pathology that leads to the formation of tumors. This is due to the proliferation of the epithelium, which gradually changes its structure abnormally.
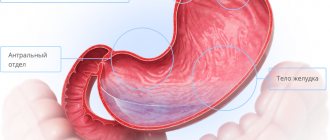
- Hyperplasia of the antrum of the stomach. Damage to the section that closes the stomach and serves to release food into the intestines. Often affects the duodenal bulbs.
- Glandular. The formation of polyp-shaped growths consisting of glandular cells.
- Polypoid. Benign neoplasm, single or multiple compactions with dense structural changes.
Treatment
You should not try to cure the disease on your own; if you detect the first signals of an impending disease, you should consult a gastroenterologist for advice
Benign lymphofollicular hyperplasia does not require treatment.
If a malignant growth of gastric lymphoid tissue is diagnosed at an early stage, antibiotic therapy can help eliminate Helicobacter pylori.
Most lymphofollicular hyperplasia of the gastric antrum respond to modern treatment methods - radiotherapy and chemotherapy.
In later stages, surgery may help by removing only the affected part or the entire stomach. Complete removal of the stomach is called a gastrectomy.
Tumors that are limited to the inner layer of the stomach wall (mucosa) can be removed during gastroscopy. In this case, only part of the tumor and immediately adjacent tissue are removed. For deep-seated tumors, part or all of the stomach, including surrounding lymph nodes, the spleen, and part of the pancreas, must be removed. To restore the passage of food, the rest of the stomach, or the end of the esophagus, is connected to the small intestine.
Additional chemotherapy (given both before and after surgery) may improve the chances of survival for patients with locally advanced tumors that have an increased risk of recurrence.
If the tumor has spread to the abdomen (peritoneal carcinomatosis), the patient's life can be prolonged by surgical removal of the affected peritoneal membrane in combination with so-called hyperthermic intraperitoneal chemotherapy.
If the tumor cannot be completely removed, surgery is not performed. In this case, drug treatment (chemotherapy, possibly in combination with other medications) can relieve symptoms, prolong and improve quality of life.
If the stomach is severely compressed by a tumor, inserting a plastic or metal tube (called a stent) may help you eat normally.
Many patients suffer from digestive problems after surgery.
First symptoms of the disease
When sick, patients may experience a fever.
The disease is considered latent, so manifestation does not always occur in the first stages of formation. This significantly complicates the diagnosis of the disease and its presence is determined at the advanced stage. Common signs of pathology are fever, weakness and apathy, a quantitative increase in lymphocytes and a decrease in albumin levels. Benign tumors have no symptoms; malignant tumors are characterized by severe abdominal pain and dyspeptic disorders. Patients with lymphofollicular hyperplasia often suffer from nausea, heartburn and vomiting.
What is lymphofollicular hyperplasia?
Generalized signs of lymphofollicular hyperplasia are considered to be an increase in temperature, a feeling of weakness, a quantitative increase in lymphocytes
Lymphoid hyperplasia of the gastrointestinal tract is divided into local (local) and diffuse (scattered). With local lymphoid hyperplasia of the colon, visible polyps are formed. Diffuse lymphoid hyperplasia is a scattered benign neoplasm; it is thought to be a general response of mucosal lymphoid cells to an unknown stimulus.
Nodular lymphoid hyperplasia of the duodenal bulb is characterized by multiple individual mucous nodules. The most common cause of malignant lymphofollicular hyperplasia of the intestine or stomach is extranodal B-cell lymphoma from marginal zone cells (maltoma, or MALT lymphoma).
Some studies show that maltoma is slightly more common in women than in men. No significant racial differences in disease prevalence were identified; Some studies suggest that lymphofollicular hyperplasia of the ileum is slightly more common in white people than in black people.
Symptoms
Symptoms of LFH vary greatly and depend on the underlying cause. In some cases, they can also be similar to the symptoms of stomach cancer. However, some patients are more likely to suffer from heartburn, nausea, vomiting, diarrhea and flatulence.
Prolonged vomiting and nausea are signs of late stage maltoma. If you suddenly lose your appetite, experience unexplained diarrhea or stomach discomfort, it is recommended to consult a doctor. Maltomas in the early stages can be cured. Later stages of the disease are difficult to treat.
Initially, patients feel weak, suffer from loss of appetite, and sometimes nausea. Sometimes there is a diffuse feeling of pressure in the abdomen. Only at the last stage, in addition to night sweats, abdominal pain and fever occur. Sometimes body weight decreases.
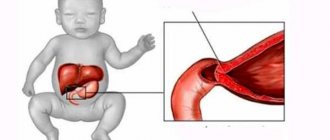
With LFG of the intestine, intestinal bleeding is possible.
Causes
Concomitant problems - obesity, liver dysfunction - can trigger the pathogenic mechanism of lymphofollicular hyperplasia
During infections or inflammations in the body, the work of the immune system is enhanced: the division of immune cells - lymphocytes - accelerates in the lymph nodes. The main function of lymph nodes is to filter lymph. To ensure immune functions, the lymph nodes become significantly enlarged - this is a normal and healthy sign of increased immune activity.
The lymph node may also become enlarged due to the growth of malignant cells. As a rule, lymph nodes affected by cancer do not cause pain when touched and are difficult to move because they merge with the surrounding tissue.
There are numerous lymph nodes in the wall of the stomach. If they are malignantly enlarged, they are called gastric lymphoma. Most gastric lymphomas are malignant maltomas that are limited to the gastric mucosa. MALT stands for mucosa-associated lymphatic tissue.
There are primary and secondary gastric lymphomas. Primary make up about 80% of all lymphomas of the digestive tract. They develop directly from lymphoid cells of the gastric mucosa. There are no other diseases that would contribute to the development of the disease. Secondary gastric lymphomas develop as a result of metastasis of tumors located in other organs.
The ileum constitutes approximately 60% of the entire length of the small intestine and is thus up to 3 m in adults. The ileum contains a large number of lymphoid follicles called Peyer's patches. Lymphofollicular hyperplasia of the ileum occurs due to primary or secondary immunodeficiency, as well as chronic inflammatory bowel disease - Crohn's disease.
Lymphoid hyperplasia of the colon often occurs in combination with polyposis. Lymphofollicular intestinal hyperplasia is common in newborns and children under 6 years of age. The exact cause of lymphoid hyperplasia has not been established. It is believed that lymphoid hyperplasia may be a response to various irritants (medicines, food components).
Complications
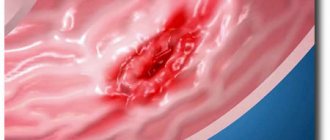
Like other gastrointestinal lesions, lymphofollicular hyperplasia can lead to undesirable consequences. Benign formations do not particularly affect the complication of the problem, but sometimes polyps form at the sites of erosion and begin to bleed, forming open wounds. This leads to the formation of lesions on the stomach walls, ulcers and malignant tumors. Large accumulations of compactions form a degenerative membrane unable to perform functions, which is why disorders and pathological dysfunctions occur. The most dangerous outcome of such processes is a malignant tumor of various sizes.
Traditional methods of treatment
If you want to forget forever what lymphoid follicles in the stomach are, then along with drug treatment and diet, you can follow the following popular advice:
- In order for the source of inflammation to heal faster and the walls of the stomach to be protected, plantain juice-extract should be consumed internally. For 2 weeks it is taken 50 ml three times a day.
- Propolis has an antibacterial effect. 10 drops of its tincture (available freely in pharmacies) are diluted with 100 ml of water. For 2 weeks, drink half a glass of this liquid 20-30 minutes before meals.
- Honey will help the epithelium and acidic environment recover faster. You can either take it in its pure form or prepare honey water - 15-20 grams per glass of water. Drink this solution three times a day, half an hour before meals.
- Sea buckthorn oil is both an anti-inflammatory and a healing agent. Dosage - 1 teaspoon also half an hour before meals.
- For low acidity, take half a glass of blackcurrant juice three times a day.
- It is the freshly squeezed juice of white cabbage or young potato tubers that has bactericidal properties. Dosage - 1/2 cup 3 times a day.
- Anti-inflammatory collection - peppermint leaves, calamus root, flax seeds, linden flowers. They are poured with 0.5 liters of boiling water and allowed to steep for 1-2 hours. Drink 1/2 cup of the strained mixture half an hour before meals.
- The antibacterial healing composition is chamomile, yarrow, flaxseeds (all 10 grams). Pour a glass of boiling water over the herbs and let it brew. The strained drink should be taken 2-3 tablespoons immediately before meals.
- Aloe juice is also recommended for restoring stomach functions - for three weeks, 20 ml twice a day before meals.
- Drinking flaxseed jelly has a good effect. To prepare it, 10 grams of seeds are crushed into dust and filled with cold water. Cook the mixture over low heat for 10 minutes. After an hour of infusion, it is ready for use - 10 ml 15 minutes before meals. The course lasts a month.
Early diagnosis is the basis of treatment
All diagnostic measures are carried out to establish the characteristics of the disease; it is impossible to diagnose the disease without the use of medical equipment. Treatment of lymphofollicular hyperplasia begins with diagnosis and examination of the patient. For this they widely use:
The FGDS procedure will help determine the presence of pathology.
- Radiography, which helps determine the contours, shape and size of polyps on the walls.
- Endoscopy. Carry out for histological analysis of polyp tissue.
- Fibrogastroduodenoscopy. Used for visual inspection of the gastrointestinal tract. The procedure is appropriate for making a diagnosis and determining the nature of the formation: polyp or tumor.
Reasons for development
It is impossible to determine the exact causes of the disease. Today, most gastroenterologists believe that the disease develops against the background of individual intolerance to gluten, which is part of most bread and other baked goods, and cereal products.
In people suffering from lymphofollicular gastritis, the body's defenses attack this protein (gluten), considering it a health threat. Having dealt with gluten, immune cells are mistaken for the tissues of the digestive tract.
Doctors are convinced that Helicobacter pylori, which causes various pathological processes in the gastrointestinal tract, also makes its destructive contribution. Her favorite organs are the stomach and duodenum. With lymphocytic gastritis, lesions characteristic of this pathogenic bacterium are found in the tissues of these organs, and its presence is confirmed by the results of laboratory tests.
Doctors believe that people who abuse sweet soda, alcoholic beverages, and “junk” foods (chips, crackers, sandwiches) are at risk and can develop this type of gastritis. The list of potential victims also includes fans of fatty, spicy, fried and smoked foods.
In addition to lymphocytic, there is also plasmacytic gastritis, and also of unclear etiology. This form is characterized by the accumulation of a large number of leukocytes in the organs of the digestive tract. The symptoms of the disease are similar to typical manifestations of chronic inflammation of the inner lining of the stomach. Without a thorough medical examination and laboratory test results, pathology cannot be diagnosed.
Treatment of pathology
Treatment of the disease is closely related to the causes of its occurrence. The factors that caused pathological changes in the structure of the mucous membrane determine the methods of influencing the problem. A fundamentally important nuance in the selection of treatment measures is the individual characteristics of the patient, since many of the techniques have a number of contraindications. Hyperplasia is treated with:
- drug therapy;
- diets;
- surgical intervention.
A special diet is effective for a disease caused by poor nutrition. This condition is easily stabilized through proper nutrition and restrictions. The medicinal method using antibiotics helps cure the disease caused by the bacterium Helicobacter pylori. Polyps that reach sizes greater than 1 cm must be removed surgically.
Several types of rare gastritis
There are several other forms of gastritis, which occur in 1% of the total number of cases:
- Granulomatous gastritis, developing in patients with tuberculosis, mycosis of the stomach and sarcoidosis. The symptoms are similar to all forms of gastritis, only with vomiting there is bloody discharge. Identified by cellular granulosa formations in the stomach.
- Eosinophilic gastritis appears with food allergies, eczema and bronchial asthma. The appearance of polyps on the mucous surface of the stomach is observed. The main symptom is bleeding from the stomach.
- Hypertrophic gastritis is a poorly studied form in which there is significant thickening of the gastric mucosa. Caused by yeast and other infections.
- The review concludes with radiation gastritis, as the name suggests, which appears when receiving radiation exposure, which causes damage to the mucous surface of the stomach.
Prevention
An important aspect in preventing the disease is the competent and complete treatment of ulcers and gastritis, which can provoke cell proliferation in the affected areas and lead to malignant tumors. It is recommended to undergo regular medical examinations, which will help identify the problem in a timely manner. Proper and balanced nutrition, proper rest and adherence to a daily routine will have a positive effect on the condition of the microflora and stomach tissues. It is worth avoiding stressful situations and evenly distributing loads throughout the day. It is recommended to give up bad habits and foods.
Treatment and dangers of lymphoid gastritis
Lymphoid gastritis is a dangerous disease that can develop into forms that threaten the patient’s life. However, it responds well to treatment, subject to timely consultation with a specialist, compliance with prescribed therapeutic recommendations and mandatory adherence to a diet. A healthy diet should be followed even after the intensity of symptoms has decreased and gastritis has gone into remission.
Therapeutic measures are individual in nature and depend on the etiology and clinical picture of the disease. This type of inflammation of the gastric mucosa makes it difficult to choose medications and draw up a comprehensive treatment program.
If an instrumental study confirms the presence of Heliobacter in the gastric microflora, specialists prescribe antibiotics. As an auxiliary therapy, drugs are used that gently envelop the walls of the stomach, reducing the aggressiveness of the digestive juice.
If an instrumental study confirms the presence of Heliobacter in the gastric microflora, specialists prescribe antibiotics
The main attention in the treatment of any form of gastritis is paid to a special diet. Food products are selected depending on the degree of acidity of the gastric enzyme. Food should be taken in small portions up to five to six times a day. Naturally, it is necessary to exclude the consumption of alcohol and foods that irritate the walls of the stomach. The black list consists of fried, salted, smoked, spicy, spicy dishes. This also includes soda, confectionery, strong tea, coffee.
The chronic course of the disease can unnoticeably turn into a malignant form. In order to avoid irreversible consequences, it is advisable to systematically carry out medical diagnostics and adjust lifestyle.
Following simple rules will significantly reduce the risk of complications:
- Avoid psycho-emotional overload and stress as much as possible;
- engage in moderate exercise daily;
- walk in the fresh air for at least an hour every day;
- balance work and rest;
- create a favorable microclimate in the family and at work;
- learn and practice relaxation techniques;
- say a convincing “no” to bad habits.
Stress and poor lifestyle form a favorable basis for the proliferation of Heliobacter. In this regard, following the above rules will be the best preventive and therapeutic measure in the fight against follicular gastritis.
Diagnosis of gastric hyperplasia
To establish the exact cause and form of the disease, a number of measures are necessary.
It is necessary to conduct histology and cytology of the biomaterial obtained from the inner surface of the stomach.
It is imperative to do a test for the presence of H. Pylori, as well as antibodies to it in the patient’s blood. Stool is examined to detect antigen.
A breath test using urea is often performed to identify traces of the bacteria.
It is mandatory to undergo ultrasound, CT and MRI,
To determine the exact cause and essence of the process, gastroscopy and other endoscopic studies are required. It is also necessary to carry out radiography using a contrast agent.